Prolapse .ppt
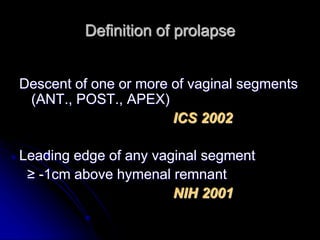
- 1. Definition of prolapse Descent of one or more of vaginal segments (ANT., POST., APEX) ICS 2002 Leading edge of any vaginal segment ≥ -1cm above hymenal remnant NIH 2001
- 2. Lifetime risk for surgery for prolapse / urinary incontinence 11% (ACOG 2007) >30% require repeat surgery (Progress 2007)
- 3. Possible risk factors Genetic predisp. Vaginal birth Parity Menopause Advancing age Prior pelvic surgery Connective tissue dis. ↑ IA pressure Obesity Chronic constipation ↑ Straining ACOG 2007
- 4. Established risk factors Vaginal delivery (levator ms injury/ endopelv.fascia ) Advancing age Obesity Lancet 2007
- 5. Baden & Walker (1972) Prolapse not due to stretching but rather breaks in the fascia which could & should be repaired individually.
- 6. 3 Delancey’s three levels of pelvic support.
- 7. The vagina can be divided into three levels. Reprinted from DeLancey (1992, AJOG) Ischial spine & sacrospinous ligament Levator ani Pubocervical fascia Rectovaginal fascia
- 8. Copyright ©2007 BMJ Publishing Group Ltd. Doshani, A. et al. BMJ 2007;335:819-823 Delancey's three levels of pelvic support. Reprinted from Barber,8 with permission from the Cleveland Clinic Foundation
- 9. Level 1: The cardinal-uterosacral ligament complex provides apical attachment of the uterus and vaginal vault to the bony sacrum. Uterine prolapse occurs when the cardinal-uterosacral ligament complex breaks or is attenuated. Level 2: The arcus tendineous fascia pelvis and the fascia overlying the levator ani muscles provide support to the middle part of the vagina. Level 3: The urogenital diaphragm and the perineal body provide support to the lower part of the vagina.
- 10. LEVEL I SUPPORT This level consists of the cardinal and uterosacral ligaments attachment to the cervix and upper vagina
- 11. LEVEL II SUPPORT This support consists of the paravaginal attachments that are contiguous with the cardinal/uterosacral complex at the ischial spine. These are the connective tissue attachments of the lateral vagina anteriorly to the arcus tendineus fascia pelvis and posteriorly to the arcus tendineus rectovaginalis. Detachment of this connective tissue from the arcus tendineus fascia pelvis leads to lateral or paravaginal anterior vaginal wall prolapse.
- 12. Level II POP at this level can be described as a central hernia through the pubocervical fascia—i.e. a cystocoele and/or an enterocoele or rectocoele—when herniation is occurring through the rectovaginal fascia in the upper or middle part
- 13. LEVEL III SUPPORT The perineal body, superficial and deep perineal muscles, and fibromuscular connective tissue comprise level III. Collectively, these support the distal one-third of the vagina and introitus. The perineal body is essential for distal vaginal support as well as proper function of the anal canal. Damage to level III support contributes to anterior and posterior vaginal wall prolapse, gaping introitus, and perineal descent.
- 14. Weakening of / Dysfunction ↓ ↓ ↓ Lev.ani Endopelvic fascia Direct injury & its condensn. Denervation Congenital Age related Child birth injury
- 15. Potential risk factors (cont..) Shape / orientation bony pelvis Family H/O Race / Ethnicity Occup. Heavy weight lifting Constipation Connective tissue disorder H/O hysterectomy (esp.for prolapse) SERM Lancet 2007
- 16. Potential risk factors OBSTETRICS Preg. irrespective of mode of delivery Forceps Young age at 1st delivery Prolonged 2nd stage Large baby Lancet 2007
- 17. R. Shaw S. Stanton Ant. Vag. wall prolapse 51% Post. Vag. wall prolapse 27% Uterine / Vault prolapse 20%
- 18. Midline or distension cystocele. Note the characteristic loss of vaginal wall rugae
- 19. a lateral cystocele, also termed paravaginal or displacement cystocele. Rugae are present, which indicates that loss of support is lateral rather than central
- 22. Subtotal hysterectomy not protective Prophylactic culdoplasty protective
- 23. Demonstarting uterine descent Single tooth valsellum to cervix Gentle traction
- 24. SYMPTOMS VAG. URINARY BOWEL SEXUAL ACOG RECOMMENDATIONS (Level A): The only symptom specific to prolapse is the awareness of a vaginal bulge or protrusion. For all other pelvic symptoms, resolution with prolapse treatment cannot be assumed
- 25. VAGINAL SYMPTOMS Bulge / Protrusion Pressure Heaviness Discharge (if ulcer)
- 26. URINARY SYMPTOMS Frequency Urgency Incontinence Weak / Prolonged stream Hesitancy Manual reduction- void Position change to start or complete voiding Retention (rare)
- 27. Urinary Frequency Most women void 8 times per day or less. Without a history that reflects increased fluid intake, increased voiding may indicate urge incontinence, urinary tract infection, calculi, or urethral pathology, and should prompt additional evaluation. In women with IC, the number of voids may commonly exceed 20 per day. Williams Gynecology
- 28. Urinary Retention It is important to determine if the patient adequately empties her bladder. Often incomplete emptying can result in incontinence associated with either stress or urgency. The term overflow incontinence is no longer used. Williams Gynecology
- 29. Williams Gynecology The volume of urine lost with each episode may also provide diagnostic clues. Large volumes are typically lost following the spontaneous detrusor contractions associated with urge urinary incontinence and may often involve loss of the entire bladder volume. In contrast, women with SUI usually describe smaller volumes lost.
- 30. Postvoid dribbling is classically associated with urethral diverticulum, which may often be mistaken for urinary incontinence
- 31. BOWEL SYMPTOMS Incontinence (because of common risk factors) Feeling of incomplete emptying Straining during defecation Urgency Splinting / Digital pushing
- 32. OTHERS ? Back pain (Advanced prolapse- ↓ back pain) ? Dysparenunia
- 33. Lancet 07 Although patients with pelvic organ prolapse sometimes attribute back and pelvic pain to their prolapse, very little evidence is available to show that the disorder causes pain. The complaint of pain in a woman with prolapse should prompt clinicians to search for other sources of the pain before attributing it to the disorder.
- 34. Examination Resting Straining Retract post wall to see Dorsal / Squatting / Lt. lateral / ant wall Lithotomy / standing prolapse & Sims speculum vice versa. Bivalve speculum P/V P/R R/V
- 35. The extent of prolapse of the anterior vaginal wall can be assessed by placing a Sim’s speculum in the vagina to retract the posterior vaginal wall The blade is then placed to retract the anterior vaginal wall and she strains again to reveal any posterior prolapse.
- 36. Lancet -07 A bivalve speculum is inserted and the cervix or—in women who have had a hysterectomy—vaginal cuff is identified to assess apical vaginal support. While the patient strains the speculum is slowly withdrawn and the descent of the vaginal apex is noted A rectovaginal examination can be useful to identify presence of a rectocoele and establish the integrity of the perineal body A bimanual and rectal examination is undertaken to rule out coexistent gynaecological or rectal pathological fi ndings.
- 37. Bivalve speculum to assess apical vaginal support (cervix / vaginal cuff) Patient strains --speculum gradually withdrawn
- 38. The Marshall test, otherwise known as the Marshall- Bonney test, is performed by placing an index finger and the second finger on either side of the bladder neck. With the bladder relatively full, the patient is instructed to perform Valsalva or cough. The 2 fingers at the bladder neck serve to support the proximal urethra during Valsalva maneuver. The absence of leakage with bladder neck elevation and the presence of leakage with loss of bladder neck support confirms stress urinary incontinence due to urethral hypermobility. However, the Marshall test is neither sensitive nor specific enough to diagnose stress urinary incontinence by today's standards. Thus, the Marshall test is not widely practiced today.
- 39. BJOG Bonney's test—fact or fiction? Bonney test produced significant increases in the urethral closure pressure and transmission of impulse from the abdomen to the urethra which indicated occlusion of the urethra rather than elevation of the bladder neck. The Bonney test does not differentiate between patients with sphincter weakness and those with bladder instability and therefore should be discarded. Received 5 December 1985, Accepted 10 May 1986
- 40. Q-tip test: This test is performed by inserting a sterile lubricated cotton swab (Q-tip) into the female urethra. The cotton swab is gently passed into the bladder and then slowly pulled back until the neck of the cotton swab is fit snugly against the bladder neck. The patient then is instructed to perform a Valsalva maneuver or to contract the abdominal muscles. Excessive motion of the urethra and bladder neck (hypermobility) with straining is an important finding for type II stress incontinence. A Q-tip excursion angle greater than 35° indicates urethral hypermobility
- 41. NICE UI The Q-tip, Bonney, Marshall, and Fluid-Bridge tests are not recommended in the assessment of women with UI. A urine dipstick test should be undertaken in all women presenting with UI to detect the presence of blood, glucose, protein, leucocytes and nitrites in the urine.
- 42. R / V Rectocoele / Enterocoele Integrity of perineal body
- 43. Williams Gynecology Enterocele can only definitively be diagnosed by observing small bowel peristalsis behind the vaginal wall In general, bulges at the apical segment of the posterior vaginal wall should implicate enteroceles, whereas bulges in the distal posterior wall are presumed to be rectoceles. Further distinction may be found during standing rectovaginal examination. A clinician's index finger is placed in the rectum and thumb on the posterior vaginal wall. Small bowel may be palpated between the rectum and vagina, confirming enterocele.
- 44. Danforth Detection of an enterocele is performed best in the awake, straining patient by noting a mass of small intestine between the rectum and vagina; it may not be suspected in a supine individual at rest.
- 45. Valsalva / Cough stress testing with full bladder with reduced prolapse
- 46. Danforth In instances in which the uterus is not necessarily going to be removed, uterine support should be tested before it is assumed that the uterus is well supported. This can be done by grasping the cervix with a tenaculum or ring forceps and applying traction until it stops descending. Occult prolapse, in which the cervix comes below the hymenal ring, can be detected in this way
- 47. The five stages of prolapse Stage 0: No prolapse Stage I: The most distal portion of the prolapse is >1 cm above the level of the hymen Stage II: The most distal portion of the prolapse is ≤1cm proximal or distal to the hymen Stage III: The most distal portion of the prolapse is >1 cm below the hymen but protrudes no further than 2 cm less than the total length of the vagina Stage IV: Complete eversion of the vagina
- 48. The staging system is not as sensitive as the POPQ for description and follow-up of individual patients.
- 49. Pelvic muscle function assessment Palpate pelvic muscles a few cms. inside hymen : 4 & 8 o’clock Baseline tone / Increase with contraction
- 50. May identify women who benefit from pelvic muscles exercise Women taught
- 51. For women with positive prolapse reduction stress test results who are planning vaginal prolapse repair, tension- free vaginal tape (TVT) midurethral sling (rather than suburethral fascial plication) appears to offer better prevention from postoperative stress incontinence
- 52. Need for ancillary testing beyond a comprehensive history and physical examination depends largely on the patient’s presenting symptoms. Most women will need little additional testing. Those with pelvic organ prolapse who complain of lower urinary-tract symptoms should undergo urinalysis and post-void residual volume testing with a urethral catheter or bladder ultrasound. Lancet 07
- 53. Lancet 07 Urodynamic assessment : with substantial urinary incontinence, irritative voiding symptoms, or voiding dysfunction. Although urodynamics are currently being used to predict postoperative urinary incontinence, findings of a randomised trial have disputed the usefulness of this test as a predictor of altering surgical management
- 54. Prevention of VAULT PROLAPSE following VAGINAL HYSTERECTOMY McCALL culdoplasty Approximating the uterosacral ligaments using continuous sutures so as to obliterate the peritoneum of posterior cul- de-sac as high as possilble. After midline approximation the uterosacrals fixed to the vault.
- 55. A similar procedure described for abdominal hysterectomy. Uterosacrals identified prior to dividing them from the uterus (Progress 2007)
- 56. SACROSPINOUS FIXATION at the time of vaginal hysterectomy is recommended for MARKED UTEROVAGINAL PROLAPSE WHEN the VAULT DESCENDS to INTROITUS DURING CLOSURE (at the end of ant. vag. wall closure) (RCOG 2007 oct)
- 57. Incidence of vault prolapse after hysterectomy ↓ ↓ ↓ After vag. After abd. (for prolapse) (non prolapse) 12% 2% (J Reprod Med 1999)
- 58. Urodynamic studies No urinary stmptoms – not justified Do only if significant urinary symptoms
- 59. Urodynamic studies(cont..) ↓ ↓ ↓ Obstructed Atonic Overactive voiding bladder ↓ ↓ ↓ surgery will good prog. less not improve after cystocoele favourable symptoms repair
- 60. R / V examination Anterior displacement of rectal finger towards vagina --- rectocoele Pt. asked to strain Non rugated vag. epithelium proximal to examining finger --- enterocoele
- 61. McCall culdoplasty Uterosacral ligament SUSPENSION for VAGINAL APEX Upto 3 sutures placed in each uterosacral ligament & incorporated into the ant & post vaginal (fibromuscular layers + vag epith.) Some surgeons approximate The uterosacral lights in midline Done if esp.redundant cul-de-sac
- 62. McCALL Culdoplasty (cont..) ↓ ↓ Excessive redundant Otherwise cul-de-sac suspend the rt & lt Approximate the 2 vag. apex to ipsilateral uterosacrals in uterosacral ligament midline ↓ Less post op bowel vaginally done by dysfunction McCALL
- 63. Post. Colporrhaphy Midline plication of subepithelial vaginal tissue Traditionally MEDIAL PORTION of LEVATOR ANI PLICATED Largely abandoned because of dyspareunia ACOG 2007
- 64. Reconstruction of perineal body = Perineorrhaphy
- 65. Mesh use in ANT / POST COLPORRHAPHY WHO (2005) Mesh transvaginally only in TRIALS May have place in recurrent cases
- 66. Sacrohysteropexy Junction of cervix & uterus is attached by a mesh,which is peritonised,to the ant. longitudnal ligament over S1 or S2.
- 67. Pessaries TRADITIONALLY Pregnancy Med contraindic. to surgery Debilitated patients CURRENTLY Can be fitted in most women regardless of prolapse stage or site of predominant prolapse ACOG 2007
- 68. Pessaries (cont..) Clinicians should discuss option with ALL WOMEN WHO have SYMPTOMATIC PROLAPSE Should be considered before surgery ACOG 2007 Women who fail / decline pessary are candidates for surgery LANCET 2007
- 69. Surgery compartment Ant colporrhaphy Posterior Site sp.repairs Uterine Vault colporraphy VH+repair Sacrocolpopexy Sacrohysteropexy Sacrospinous fixation Sling Operations ANT. MIDDLE POST.
- 70. Cystourethrocoele with USI ↓ ↓ ↓ Ant.colporrhaphy Burch + Colposuspension TVT
- 71. STRESS INCONTINENCE Improves as prolapse extends beyond hymen possibly from urethral obstruction Latent stress incontinence in symptomatically continent – also called OCCULT / MASKED
- 72. ACOG RECOMMENDATIONS (Level A): Stress-continent women with positive stress test results (prolapse reduced) are at higher risk for developing postoperative stress incontinence after prolapse repair alone compared with women with negative stress test results (prolapse reduced)
- 73. ACOG RECOMMENDATIONS (Level A): For stress-continent women planning abdominal sacral colpopexy, regardless of the results of preoperative stress testing, the addition of the Burch procedure substantially reduces the likelihood of postoperative stress incontinence without increasing urgency symptoms or obstructed voiding.
- 74. Uterine descent + Uterine preservation Manchester operation Shirodkar operation Purandare’s operation Sacrohysteropexy Sacrospinous fixation
- 75. The following recommendations and conclusions are based on limited or inconsistent scientific evidence (Level B): ACOG 2007 Compared with vaginal sacrospinous ligament fixation, abdominal sacral colpopexy has less apical failure and less postoperative dyspareunia and stress incontinence, but is also associated with more complications.
- 76. Women Considering Pregnancy Ideally, childbearing should be complete before considering surgery for prolapse to avoid the theoretical but plausible risk of recurrent prolapse after subsequent pregnancy and delivery. For women who become pregnant after prolapse repair, decisions regarding mode of delivery should be made on a case-by-case basis; evidence to guide such decisions is lacking.
- 77. Complications were more frequent in women aged 80 years and older and in women who had reconstructive rather than obliterative surgery.
- 78. Stress urinary incontinence Green 04 complaint of involuntary leakage during effort or exertion, occurs at least weekly in one third of adult women. basic evaluation of women with stress urinary incontinence includes a history, physical examination, cough stress test, voiding diary, postvoid residual urine volume, and urinalysis. Formal urodynamics testing may help guide clinical care, but whether urodynamics improves or predicts the outcome of incontinence treatment is not yet clear. The distinction between urodynamic stress incontinence associated with hypermobility and urodynamic stress incontinence associated with intrinsic sphincter deficiency should be viewed as a continuum, rather than a dichotomy, of urethral function.
- 79. Q-Tip Test If urethra is poorly supported, it may display hypermobility during increases in intra-abdominal pressures. To assess mobility, a clinician places the soft end of a cotton swab into the urethra to the urethrovesical junction. Failure to insert the swab to this depth typically leads to errors in assessment of urethrovesical junction support. Termed the Q- tip test, this evaluation may be uncomfortable and application of intraurethral analgesia may prove helpful. Commonly, 1 percent lidocaine jelly is placed on the cotton swab prior to insertion. Following placement, Valsalva maneuver is prompted, and the swab angle excursion at rest and with Valsalva maneuver is measured with a goniometer or standard protractor (Fig. 23-8). An angle excursion at rest or with Valsalva maneuver greater than 30 degrees above the horizontal indicates urethral hypermobility, and may help direct planning of surgical treatment for stress incontinence
- 80. post void residual volume of less than 50 mL is regarded as normal greater than 150–200 mL are regarded as abnormal. In older women, up to 100 mL may be regarded as normal, depending on the circumstances NOVAK:provided the patient has voided 150 mL or more, a PVR less than or equal to 100 mL is acceptable
- 81. Overactive bladder syndrome (OAB) Urgency that occurs with or without urge UI and usually with frequency and nocturia. OAB that occurs with urge UI is known as ‘OAB wet’. OAB that occurs without urge UI is known as ‘OAB dry’. These combinations of symptoms are suggestive of the urodynamic finding of detrusor overactivity, but can be the result of other forms of urethrovesical dysfunction.
- 82. Expert opinion concludes that symptomatic categorisation of UI based on reports from the woman and history taking is sufficiently reliable to inform initial, non- invasive treatment decisions.