asthma .pptx
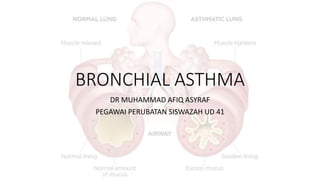
- 1. BRONCHIAL ASTHMA DR MUHAMMAD AFIQ ASYRAF PEGAWAI PERUBATAN SISWAZAH UD 41
- 2. APPROACH TO MANAGING ASTHMA A) Education of patient and family B) Identifying & avoiding the common triggers : 1. Environmental allergens : house dust mites, pollens, animal dander, insects and mould 2. Cigarette smoke 3. URTI 4. Food allergy 5. Exercise C) Drugs
- 3. CONTROL-BASED ASTHMA MANAGEMENT • Asthma treatment is adjusted in a continuous cycle to assess, adjust treatment and review response.
- 6. STEPWISE APPROACH FOR ADJUSTING TREATMENT STEP 1: As-needed SABA with no controller This is indicated only if symptoms are rare, there is no night waking due to asthma, no exacerbations in the last year, and normal FEV1. Other options: regular low dose ICS for patients with exacerbation risks. STEP 2 : Regular low dose ICS plus as-needed SABA Other options: LTRA are less effective than ICS ***For purely seasonal allergic asthma, start ICS immediately and cease 4 weeks after end of exposure.
- 7. STEP 3 : Low dose ICS/LABA as maintenance treatment plus as needed SABA, or as ICS/formoterol maintenance and reliever therapy Other options: Medium dose ICS; for adult patients with rhinitis and allergic to house dust mite (HDM) with exacerbations despite ICS, consider adding sublingual immunotherapy (SLIT), provided FEV1 is >70% predicted. Children (6–11 years): Medium dose ICS. Other options: low dose ICS/LABA STEP 4: Low dose ICS/formoterol maintenance and reliever therapy, or medium dose ICS/LABA as maintenance plus as-needed SABA Other options: Add-on tiotropium by mist inhaler for patients 12 years with a history of exacerbations; high dose ICS/LABA, but more side-effects and little extra benefit; extra controller, e.g. LTRA or slow-release theophylline (adults); for adult patients with rhinitis and allergic to HDM with exacerbations despite ICS, consider adding SLIT, provided FEV1 is >70% predicted. Children (6–11 years): Refer for expert assessment and advice.
- 8. STEP 5: Refer for expert investigation and add-on treatment Add-on treatments include tiotropium by mist inhaler for patients with a history of exacerbations age 12 years, anti-IgE (omalizumab) for severe allergic asthma >6 years anti-IL5 (SC mepolizumab or IV reslizumab) for severe eosinophilic asthma (age 12 years. Other options: Some patients may benefit from low dose OCS but long-term systemic side-effects commonly occur.
- 9. Medications / Drugs Medication Action Side effect CONTROLLER ICS (pMDI or DPIs) - beclomethasone, fluticasone, budesonide Reduce sx, increase lung function, reduce risk of exacerbation Long term : (high doses) - osteoporosis, cataract, glaucoma ICS + LABA - Beclomethasone + formoterol, budesonide + formoterol, fluticasone + formeterol Addition of LABA will improve the sx more rapidly , and reduce risk of exacerbation Tachycardia, headache, cramps LEUKOTRIENE MODIFIER - Montelukast, pranlukast, zafirlukast Target one part of the inflammatory pathway in asthma Risk of serious behaviour and mood changes CHROMONES - Sodium chromoglycate and nedocromil sodium Weak anti-inflammatory effect Less effective than low dose ICS Uncommon – may include cough upon inhalation
- 10. Add on controller medications LAMA - Beclomethasone + formoterol + glycopyrronium - Fluticasone + vilanterol + umeclidinium Uncontrolled asthma despite of ICS + LABA Dry mouth (uncommon) Anti-IgE (SC) - omalizumab Severe allergic asthma uncontrolled with high dose ICS-LABA Local reaction to injection site Anti–IL5 or Anti –IL5R - Mepolizumab - Reslizumab Severe eosinophilic asthma uncontrolled with high dose ICS – LABA Headache, local reaction at injection site Anti – IL4R - Dupilumab Severe eosinophilic asthma ot Type 2 asthma uncontrolled with high dose ICS – LABA Reaction at injection site - common SYSTEMIC CORTICOSTEROID (tablets, suspension, IV, IM) - prednisone, prednisolone, methylprednisolone, hydrocortisone Short term (5-7 days) is important in treatment of severe acute exacerbation. Tappering is required if treatment >2weeks Short term : sleep disturbances, reflux, increase appetite, mood changes Long term : cataract, glaucoma, HPT, DM, adrenal suppression osteoporosis
- 11. RELIEVER MEDICATION SABA - Salbutamol, Terbutaline Quick relief of asthma sx and bronchoconstriction Tremor and tachycardia LOW DOSE ICS – FORMOTEROL - Beclomethasone + formoterol - Budesonide + formoterol Reduce risk of exacerbation compared with using SABA as reliever, with similar sx control SHORT ACTING ANTICHOLINERGIC - Ipratropium bromide, oxitropium bromide Long term : less effective than SABA Short term in severe acute asthma : When added with SABA – reduce risk of hospital admission Dryness of mouth and bitter taste
- 12. Types of inhaler devices
- 13. AIMS OF MANAGEMENT • To prevent death • To relieve symptoms • To restore the patient’s lung function to the best possible level as soon as possible • To prevent early relapse
- 14. ASTHMA FLARE-UPS (EXACERBATIONS) - A flare-up or exacerbation is an acute or sub-acute worsening in symptoms and lung function from the patient’s usual status - It may be the initial presentation of asthma STATUS ASTHMATICUS - commonly known as acute severe asthma or a severe asthma exacerbation. - It refers to an asthma attack that doesn’t improve with traditional treatments, such as inhaled bronchodilator. - These attacks can last for several minutes or even hours.
- 15. Identifying patients at risk of asthma-related death : • A history of near-fatal asthma - intubation and ventilation • Hospitalization / emergency care for asthma in last 12 months • Not currently using ICS, or poor adherence with ICS • Currently using or recently stopped using OCS (this indicates the severity of recent events) • Over-use of SABAs, especially more than 1 canister/month • Lack of a written asthma action plan • History of psychiatric disease or psychosocial problems • Confirmed food allergy in a patient with asthma
- 16. MANAGING EXACERBATIONS IN PRIMARY OR ACUTE CARE • Assess exacerbation severity while starting SABA and oxygen. • Assess dyspnea (e.g. is the patient able to speak sentences, or only words) RR, PR, Spo2 and lung function (e.g. PEF). • Consider alternative causes of acute breathlessness (e.g. heart failure, upper airway dysfunction, inhaled foreign body or pulmonary embolism). • Arrange immediate transfer to an acute care facility if there are signs of severe exacerbation, or to intensive care if the patient is drowsy, confused, or has a silent chest. For these patients, immediately give inhaled SABA, inhaled ipratropium bromide, oxygen and systemic corticosteroids. • Start treatment with repeated doses of SABA (usually by pMDI and spacer), early oral corticosteroids, and controlled flow oxygen if available.
- 17. • Check response of symptoms and saturation frequently, and measure lung function after 1 hour. Titrate oxygen to maintain saturation of 93–95% in adults and adolescents (94–98% in children 6–12 years). • For severe exacerbations, add ipratropium bromide, and consider giving SABA by nebulizer. In acute care facilities, intravenous magnesium sulfate may be considered if the patient is not responding to intensive initial treatment.
- 18. • Criteria for admission • Failure to respond to standard home treatment. • Failure of those with mild or moderate acute asthma to respond to nebulised β₂-agonists. • Relapse within 4 hours of nebulised β₂- agonists. • Severe acute asthma ( Status Asthmaticus )
- 19. MANAGEMENT OF ASTHMA EXACERBATIONS IN ACUTE SETTINGS GINA
- 20. GINA
- 21. References • Malaysia Thoracic Society: Guidelines on Management of Adult Asthma • Pocket Guide for Asthma Management and Prevention, GINA 2015