Radiotherapy in the Treatment of Sarcomas in Adolescents and Young Adults
•
9 likes•1,671 views
Daniel Indelicato, MD, University of Florida, Jacksonville, FL Presented at the 2010 Texas Adolescent and Young Adult Oncology Conference, Methodist Healthcare-San Antonio
Report
Share
Report
Share
Recommended
More Related Content
What's hot
What's hot (20)
How Radiation Therapy is Used to Treat Soft Tissue Sarcoma

How Radiation Therapy is Used to Treat Soft Tissue Sarcoma
NEOADJUVANT RADIOTHERPAY IN SOFT TISSUE SARCOMA- A DEBATE

NEOADJUVANT RADIOTHERPAY IN SOFT TISSUE SARCOMA- A DEBATE
Gynecologic Malignancies, Penny Daugherty, RN, MS, OCN, ONN-CG

Gynecologic Malignancies, Penny Daugherty, RN, MS, OCN, ONN-CG
Retroperitoneal Soft-Tissue Sarcoma: Retrospective Study at Shaukat Khanum Ca...

Retroperitoneal Soft-Tissue Sarcoma: Retrospective Study at Shaukat Khanum Ca...
Viewers also liked
Breast Cancer Radiation Therapy: RT Plan evaluation & Recent Advances - 4DCT ...

Breast Cancer Radiation Therapy: RT Plan evaluation & Recent Advances - 4DCT ...Kidwai Memorial Institute of Oncology, Bangalore
Viewers also liked (13)
Rhabdomyosarcoma radiotherapy indications and outcome

Rhabdomyosarcoma radiotherapy indications and outcome
Richard Amos (UCLH) - Introducing proton beam therapy into the NHS #HCS15

Richard Amos (UCLH) - Introducing proton beam therapy into the NHS #HCS15
Current and emerging partnerships in imaging and radiotherapy by musila mutala

Current and emerging partnerships in imaging and radiotherapy by musila mutala
Breast Cancer Radiation Therapy: RT Plan evaluation & Recent Advances - 4DCT ...

Breast Cancer Radiation Therapy: RT Plan evaluation & Recent Advances - 4DCT ...
Similar to Radiotherapy in the Treatment of Sarcomas in Adolescents and Young Adults
Similar to Radiotherapy in the Treatment of Sarcomas in Adolescents and Young Adults (20)
Externalbeam rt in ews3.12.20 - frida yseminar-finallll

Externalbeam rt in ews3.12.20 - frida yseminar-finallll
Soft tissue sarcomas, treatment (surgical, radiation, chemotherapy)

Soft tissue sarcomas, treatment (surgical, radiation, chemotherapy)
Examenes radiologicos y riesgo de cancer en pacientes

Examenes radiologicos y riesgo de cancer en pacientes
More from Methodist HealthcareSA
Adolescents and Young Adults With Cancer Treatment and Transition to An Adult...

Adolescents and Young Adults With Cancer Treatment and Transition to An Adult...Methodist HealthcareSA
Sexual and Intimate Needs of Adolescents and Young Adults with Cancer: A Qual...

Sexual and Intimate Needs of Adolescents and Young Adults with Cancer: A Qual...Methodist HealthcareSA
Informed Consent for the Treatment of Adolescents and Young Adults with Cancer

Informed Consent for the Treatment of Adolescents and Young Adults with CancerMethodist HealthcareSA
More from Methodist HealthcareSA (20)
Adolescents and Young Adults With Cancer Treatment and Transition to An Adult...

Adolescents and Young Adults With Cancer Treatment and Transition to An Adult...
Sexual and Intimate Needs of Adolescents and Young Adults with Cancer: A Qual...

Sexual and Intimate Needs of Adolescents and Young Adults with Cancer: A Qual...
Informed Consent for the Treatment of Adolescents and Young Adults with Cancer

Informed Consent for the Treatment of Adolescents and Young Adults with Cancer
Recently uploaded
Ahmedabad Call Girls Book Now 9630942363 Top Class Ahmedabad Escort Service A...

Ahmedabad Call Girls Book Now 9630942363 Top Class Ahmedabad Escort Service A...GENUINE ESCORT AGENCY
Recently uploaded (20)
Jual Obat Aborsi Di Dubai UAE Wa 0838-4800-7379 Obat Penggugur Kandungan Cytotec

Jual Obat Aborsi Di Dubai UAE Wa 0838-4800-7379 Obat Penggugur Kandungan Cytotec
Gorgeous Call Girls Dehradun {8854095900} ❤️VVIP ROCKY Call Girls in Dehradun...

Gorgeous Call Girls Dehradun {8854095900} ❤️VVIP ROCKY Call Girls in Dehradun...
Gastric Cancer: Сlinical Implementation of Artificial Intelligence, Synergeti...

Gastric Cancer: Сlinical Implementation of Artificial Intelligence, Synergeti...
Bhawanipatna Call Girls 📞9332606886 Call Girls in Bhawanipatna Escorts servic...

Bhawanipatna Call Girls 📞9332606886 Call Girls in Bhawanipatna Escorts servic...
Ahmedabad Call Girls Book Now 9630942363 Top Class Ahmedabad Escort Service A...

Ahmedabad Call Girls Book Now 9630942363 Top Class Ahmedabad Escort Service A...
Call Girls Shahdol Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Shahdol Just Call 8250077686 Top Class Call Girl Service Available
Bandra East [ best call girls in Mumbai Get 50% Off On VIP Escorts Service 90...

Bandra East [ best call girls in Mumbai Get 50% Off On VIP Escorts Service 90...
💚Chandigarh Call Girls 💯Riya 📲🔝8868886958🔝Call Girls In Chandigarh No💰Advance...

💚Chandigarh Call Girls 💯Riya 📲🔝8868886958🔝Call Girls In Chandigarh No💰Advance...
VIP Hyderabad Call Girls KPHB 7877925207 ₹5000 To 25K With AC Room 💚😋

VIP Hyderabad Call Girls KPHB 7877925207 ₹5000 To 25K With AC Room 💚😋
ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx

ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx
Kolkata Call Girls Naktala 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Girl Se...

Kolkata Call Girls Naktala 💯Call Us 🔝 8005736733 🔝 💃 Top Class Call Girl Se...
Call 8250092165 Patna Call Girls ₹4.5k Cash Payment With Room Delivery

Call 8250092165 Patna Call Girls ₹4.5k Cash Payment With Room Delivery
Most Beautiful Call Girl in Chennai 7427069034 Contact on WhatsApp

Most Beautiful Call Girl in Chennai 7427069034 Contact on WhatsApp
Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...

Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...
Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...

Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...
👉Chandigarh Call Girl Service📲Niamh 8868886958 📲Book 24hours Now📲👉Sexy Call G...

👉Chandigarh Call Girl Service📲Niamh 8868886958 📲Book 24hours Now📲👉Sexy Call G...
Premium Call Girls Nagpur {9xx000xx09} ❤️VVIP POOJA Call Girls in Nagpur Maha...

Premium Call Girls Nagpur {9xx000xx09} ❤️VVIP POOJA Call Girls in Nagpur Maha...
Radiotherapy in the Treatment of Sarcomas in Adolescents and Young Adults
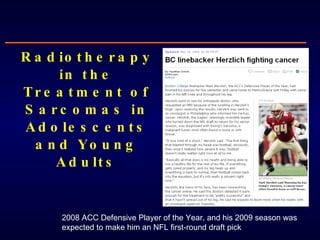
- 1. Radiotherapy in the Treatment of Sarcomas in Adolescents and Young Adults 2008 ACC Defensive Player of the Year, and his 2009 season was expected to make him an NFL first-round draft pick
- 2. No conflicts of interest to disclose
- 3. Scope of Problem in AYAs Sarcomas 15% Leukemia 14% Germ Cell Tumors 13% Brain Tumors 10% Thyroid Carcinoma 8% Melanoma 8% Other 9% Lymphoma 23% Bone sarcoma 8% Soft tissue sarcoma 7%
- 4. How Radiation is Perceived Seminars in Oncology, 2009 Number of times “radiation” is mentioned relative to side effects: 11 Number of times “radiation” is mentioned as a treatment modality: 7
- 8. Value of RT for Adolescent and Young Adult Bone Sarcomas Remember: Sarcoma type determines radiosensitivity, disease control outcomes
- 13. Value of RT for Adolescent and Young Adult Soft Tissue Sarcomas
- 14. “ The management of this condition should be radical surgery and that no help should be expected from radiotherapy either as a pre- or postoperative procedure” - Dr. Ralston Paterson (1963) Holt Radium Institute at the Christie Cancer Hospital, founded by Ralston Patterson Soft Tissue Sarcoma: Then
- 15. Annals of Surgery, 1982 27 pts WLE+RT 16 pts Amputation 43 pts High grade STS Extremity
- 16. Level I Data: General Population
- 22. Bone Tumors Soft Tissue Sarcoma
- 23. Challenges of Using Radiation for AYA Sarcoma Remember: Sarcoma location dictates treatment side effects and complications
- 26. Local Management of Lower Extremity Ewing Tumors at the University of Florida: 1970-2006 (Indelicato 2007)
- 27. 1987 1969 65 Gy 60 Gy + 20 years
- 31. Musculoskeletal Complications of Radiation Treatment
- 32. Bone Complications of Radiation Treatment Traditional risk factors for fracture: ● radiation dose (mean dose >37 Gy) ● periosteal stripping ● female gender Pathogenesis: microvascular supply; osteoclast alteration? Rate of fracture in patients with Ewing sarcoma of weight bearing bone: 30% Slipped femoral capital epiphysis radiation injury to the proximal femoral growth apparatus + weight-bearing stress After only 12 Gy
- 42. Guidelines: Minimizing Toxicity in AYA Sarcoma Male with synovial sarcoma of the proximal medial thigh Protons Photons
- 44. "He hasn't lost anything“ - ESPN commentator Curt Warner 9/6/2010
Editor's Notes
- In 1970’s, 30-40% extremity sarcoma’s were treated with amputation Now, its <15%
- AP view of a knee in a teenager treated with 54.8 Gy for a synovial sarcoma Transverse pathologic fracture of the paroximal tibial metaphysis 4 years later, healed fracture but extensive radiation osteitis of the distal femur and proximal tibia 9 years later, osteosarcoma developed in the proximal tibia
- AP view of the knee of a Ewing sarcoma patient shows growth impairment with metasphseal widening and sclerosis 14 months laters, the distal femoral metaphysis is markedly sclerotic and irregegular. The epiphyseal cartilage plate appears hypertrophied.
- Teenager treated for Ewing sarcoma of the right humerus, photo 11 years post RT. Note difference in the muscule development when he started lifting weights.
- Maynard
