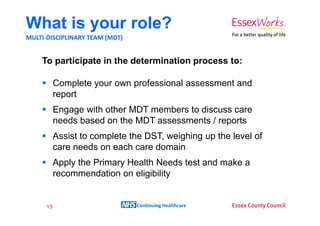
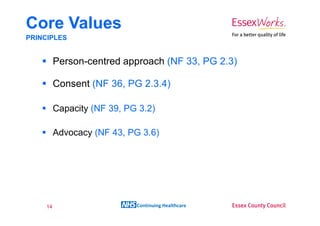
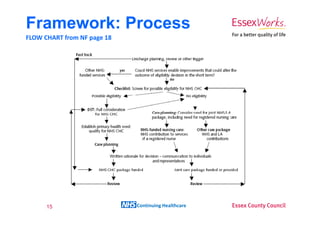
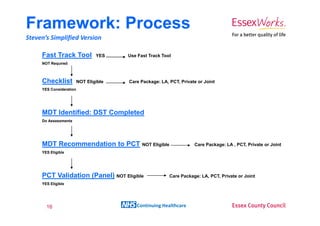
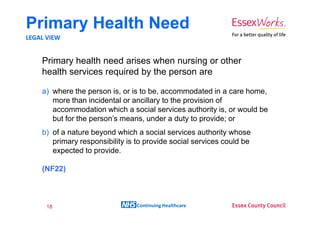
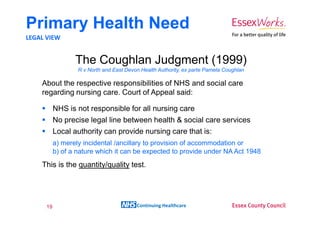
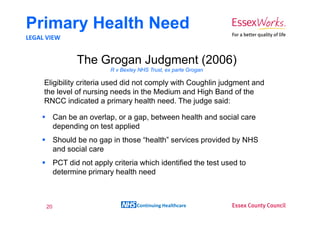
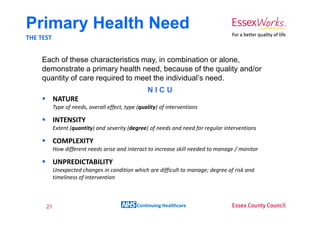
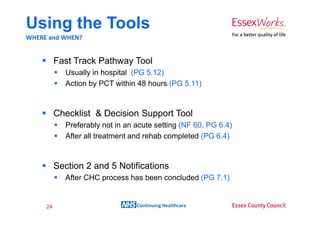
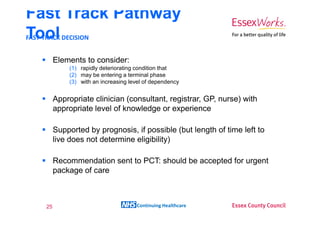
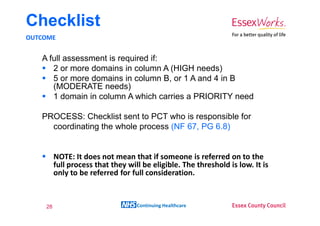
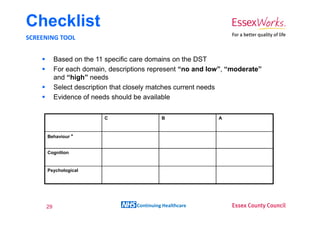
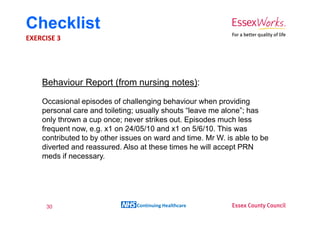
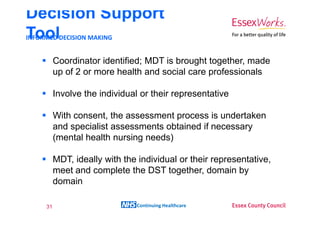
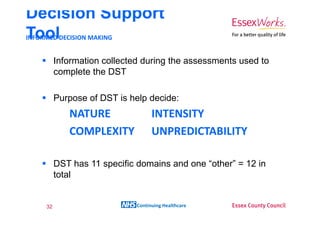
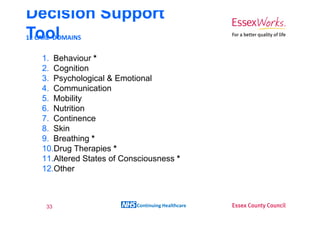
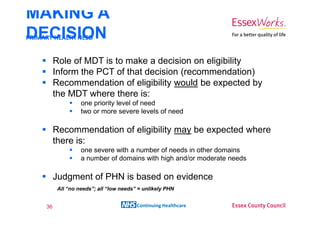
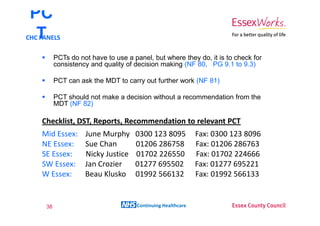
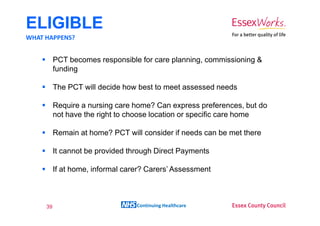
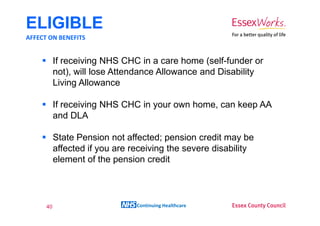
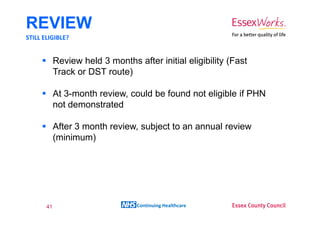
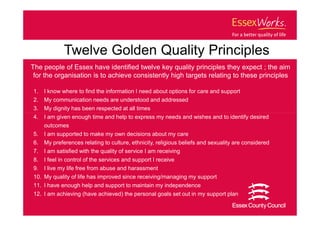
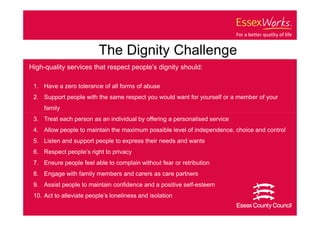
This document provides an overview of NHS Continuing Healthcare. It discusses the differences between health care and social care, and outlines the framework and tools used to determine eligibility for NHS Continuing Healthcare, including the Fast Track Pathway Tool, Checklist, and Decision Support Tool. The document emphasizes that eligibility is based on the level of an individual's care needs and whether their primary need is for health care rather than social care. It provides guidance on assessing needs against the criteria of nature, intensity, complexity and unpredictability to determine if someone has a primary health need.