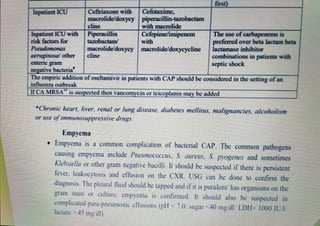
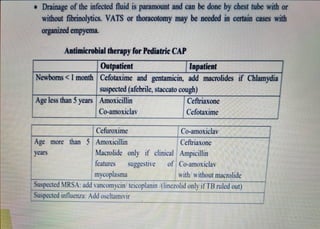
The document discusses the classification, treatment, and management of community-acquired pneumonia (CAP) in children, emphasizing the distinctions between different severity levels. It outlines treatment strategies for outpatients and inpatients, the necessity of certain laboratory investigations, and the recommendation for empirical antimicrobial therapy. Additionally, it details complications such as empyema and provides specific antibiotic dosages for various age groups and conditions.