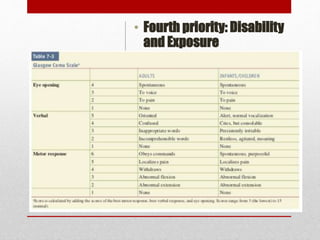
1. Trauma is a leading cause of death, especially for those aged 1-44. The Advanced Trauma Life Support (ATLS) protocol emphasizes interventions in the "golden hour" to prevent death.
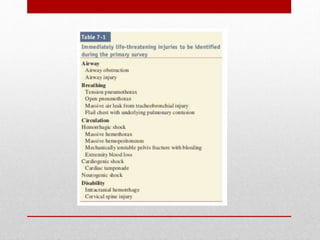
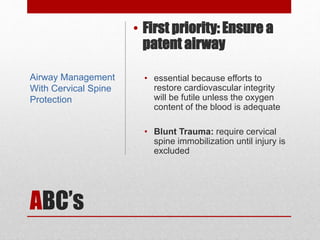
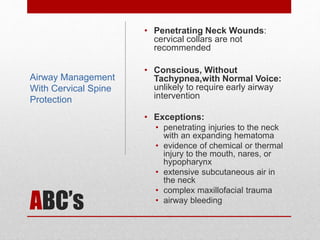
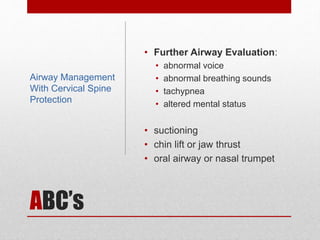
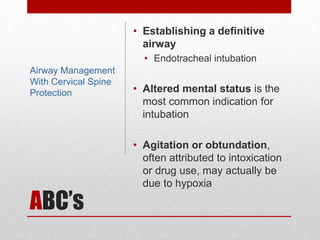
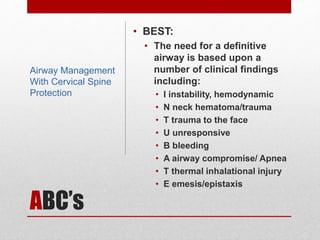
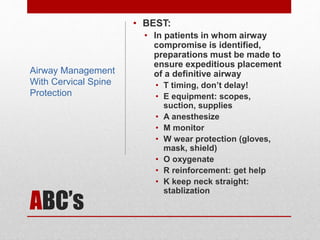
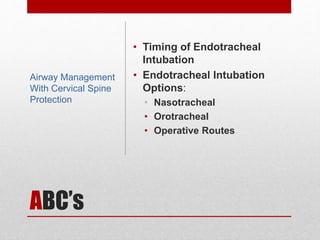
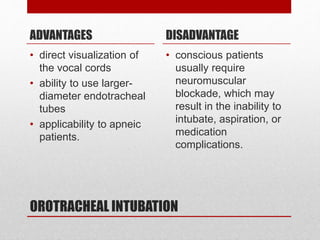
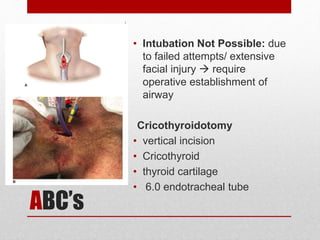
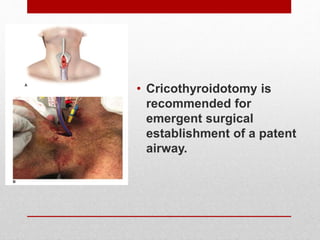
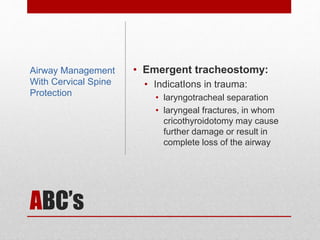
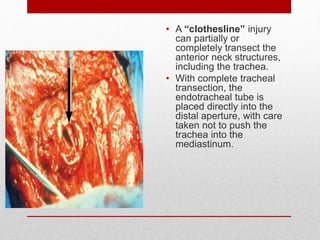
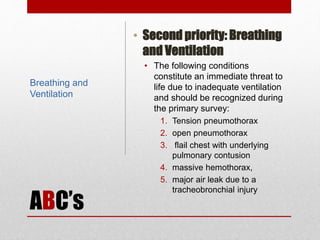
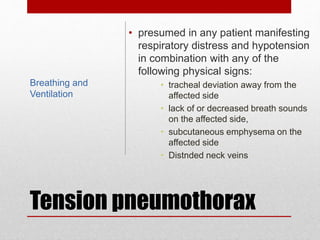
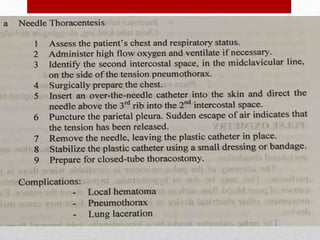
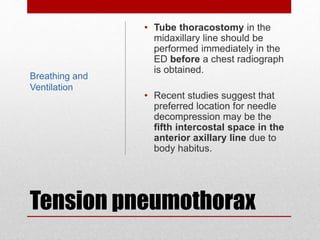
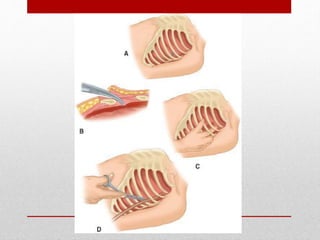
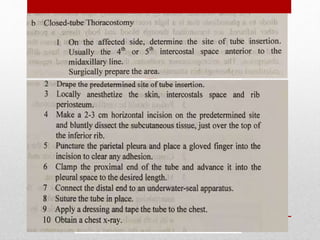
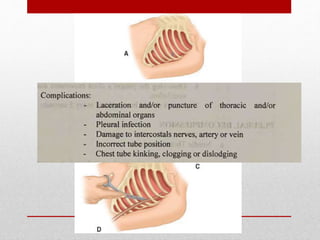
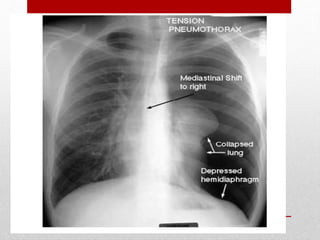
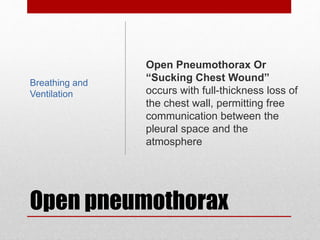
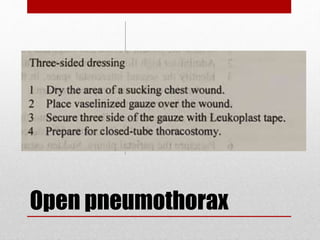
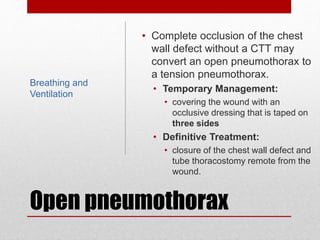
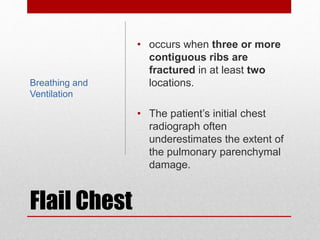
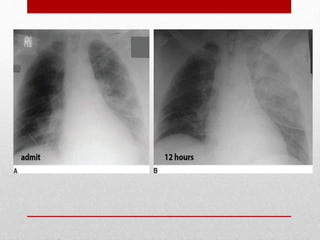
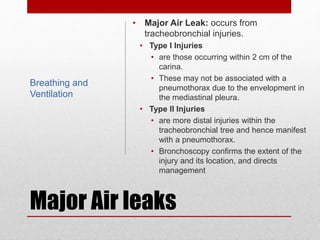
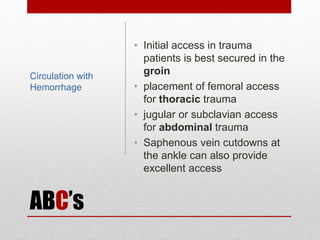
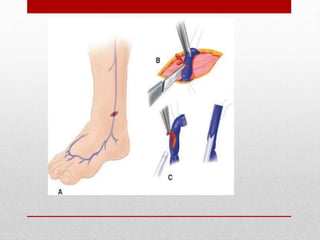
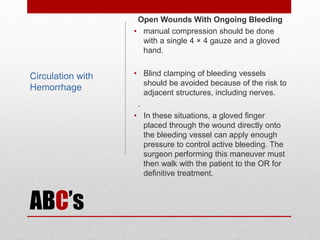
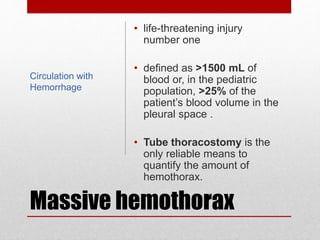
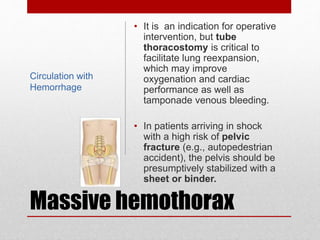
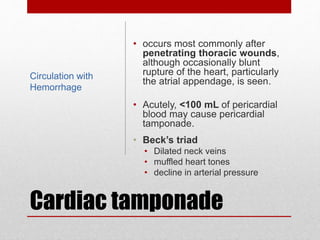
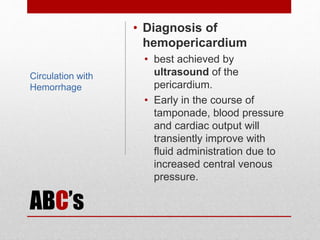
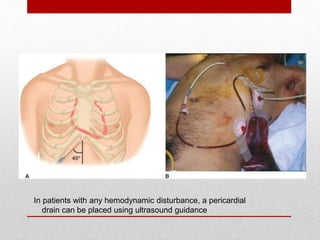
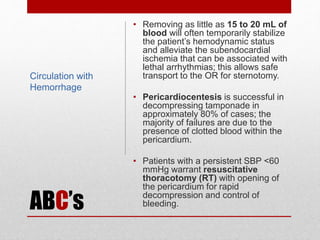
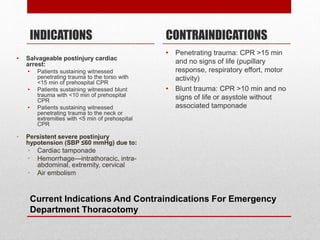
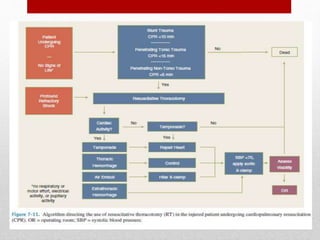
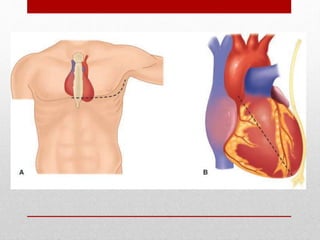
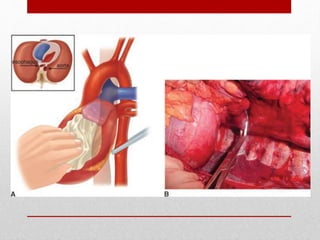
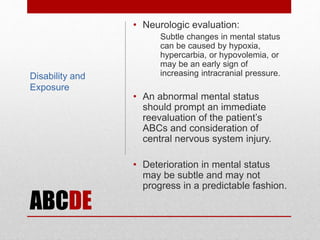
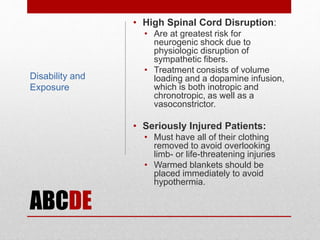
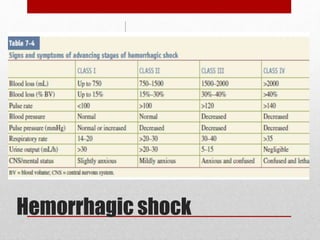
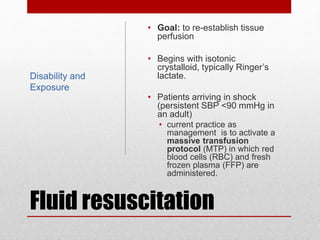
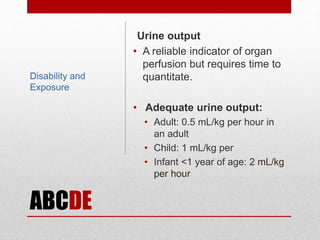
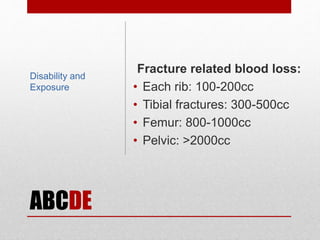
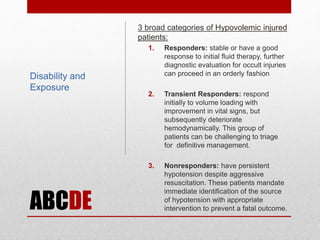
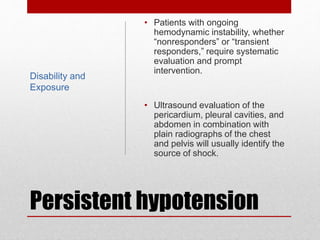
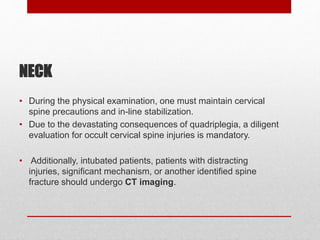
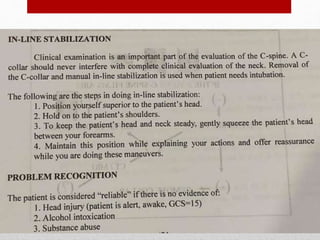
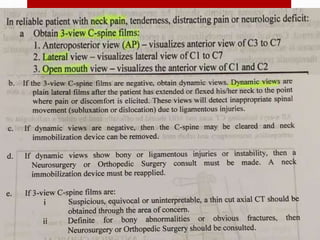
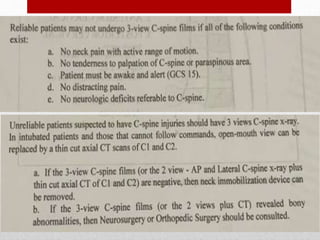
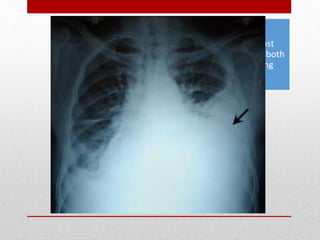
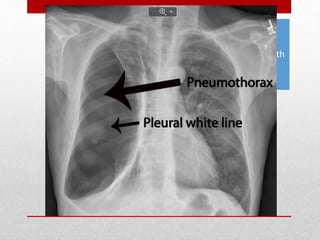
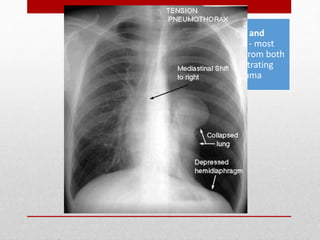
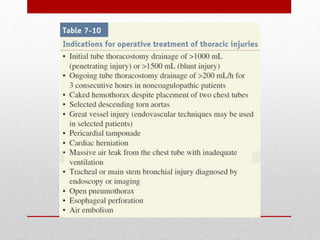
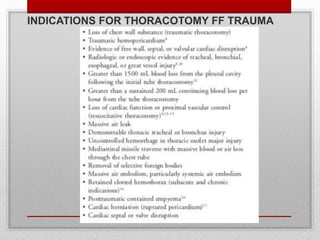
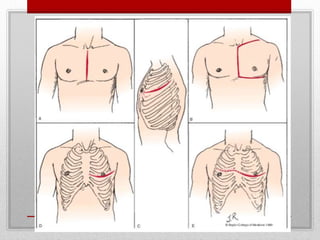
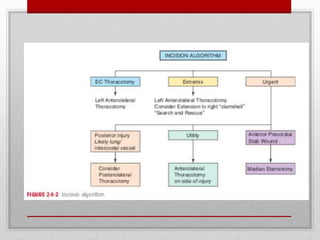
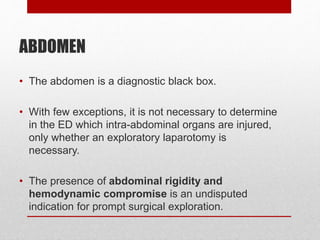
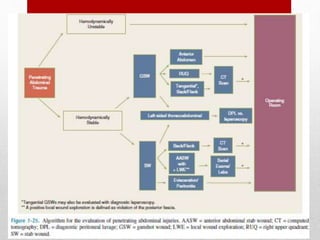
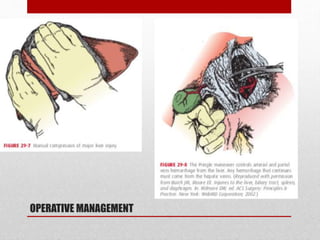
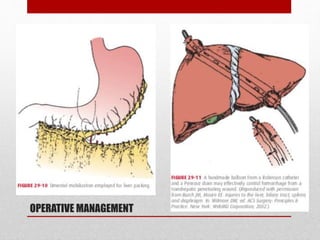
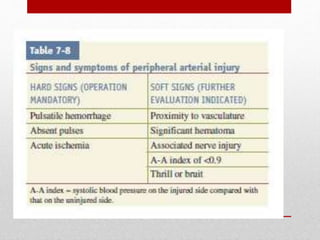
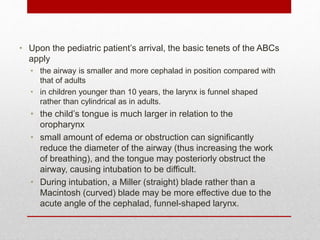
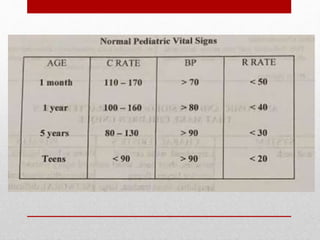
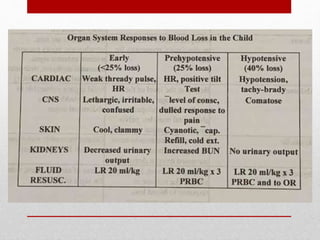
2. The initial evaluation of an injured patient follows the ABCs - Airway, Breathing, and Circulation. Airway management requires cervical spine protection. Tension pneumothorax and open pneumothorax require tube thoracostomy. Circulation assessment focuses on hemorrhage control through intravenous access, wound packing, and identifying life-threatening internal bleeding.
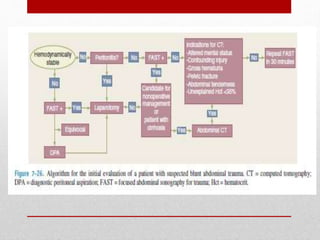
3. Proper application of the ATLS protocol during the initial trauma evaluation focuses on rapid identification and treatment of immediate threats to life