Thyroid and Anti-thyroid drugs
- 1. Thyroid & Antithyroid Drugs 1 09-02-2021
- 2. Thyroid & Antithyroid Drugs 2 09-02-2021 Thyroid & Anti-thyroid Drugs Presentation by, Dr Pooja S G Guide: Dr Nirmala N Rege
- 3. Thyroid Drugs Levothyroxine • History • Pharmacokinetics • Pharmacodynamics • Drug interactions Liothyronine Combination of T3:T4 Hypothyroidism • Treatment & Complications Anti-thyroid drugs Classification • Thionamides • Iodides • Ionic inhibitors • Radioactive-iodine Hyperthyroidism • Treatment & Complications 09-02-2021 3 Flow of seminar Thyroid drugs in Non-thyroidal illnesses Introduction
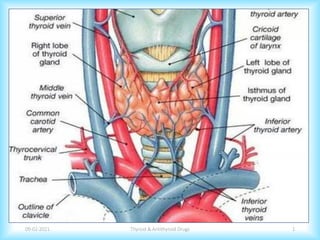
- 4. Important Actions • Metabolic actions • Cellular respiration • Metabolism of Carbohydrates, proteins and lipids. • Growth & development 09-02-2021 Thyroid & Antithyroid Drugs 4 Introduction: Thyroid Physiology Thyroxine (T4) and Triiodothyronine (T3)
- 5. Thyroid & Antithyroid Drugs 5 09-02-2021 Thyroid Drugs
- 6. 09-02-2021 Thyroid & Antithyroid Drugs 6 Levothyroxine (T4) Liothyronine (T3) Liotrix (T4:T3) Thyroid Preparations
- 7. 1891 1914 1926 1949 1962 History of Levothyroxine 09-02-2021 Thyroid & Antithyroid Drugs 7 Thyroid hormone was used for first time High yield synthetic technique C R Harrington established its structure Thyroxine discovered by Edward C Kendall Levothyroxine came into the market
- 8. 09-02-2021 Thyroid & Antithyroid Drugs 8
- 9. • Levothyroxine - an iodine-containing aminoacidic derivative embedded in a glycoprotein (thyroglobulin). • Synthetic preparations: Sodium salts • Levothyroxine sodium is available as: ➢Tablets ➢Liquid-filled capsules for oral administration ➢Lyophilized powder for injection ➢Strength- 12.5,25,50,75,88,100,112,125,150,200,300 mcg Levothyroxine is 2nd the most commonly prescribed medication in the US; 22.3 million prescriptions in 2017. Levothyroxine 09-02-2021 Thyroid & Antithyroid Drugs 9
- 10. Absorption • Stomach and small intestine and is incomplete (~80% ) • Serum T4 peaks 2–4 h after oral ingestion • Plasma t1/2 of about 7 days Factors decreasing absorption: • Antacids • Bile acid sequestrants • Malabsorption syndromes • Calcium and Iron supplements Pharmacokinetics of Levothyroxine 09-02-2021 Thyroid & Antithyroid Drugs 10
- 11. 09-02-2021 Thyroid & Antithyroid Drugs 11 Distribution ➢ Thyroid Binding Globulin (TBG) ➢ Transthyretin (TTR) ➢ Albumin The higher affinity of both TBG and TBPA for T4 partially explains the higher serum levels, slower metabolic clearance, and longer half-life of T4 compared to T3 . Clofibrate, Estrogens ↑TBG Androgens, Glucocorticoids ↓TBG
- 12. 09-02-2021 Thyroid & Antithyroid Drugs 12 Metabolism ➢ De-iodination - iodothyronine deiodinases, D1,D2,D3 ➢ Conjugation – Glucuronide and sulfate ➢ CYP3A4 Phenobarbital induce UGT Rifampin, carbamazepine, phenytoin, sertraline Amiodarone
- 13. 09-02-2021 Thyroid & Antithyroid Drugs 13 Elimination • 80% - Kidney • 20% -stools Other drug interactions • Anticoagulants • Antidepressants • Antidiabetic drugs • Drug food interactions with Dietary fibres, soyabean flour Narrow therapeutic index
- 14. • Liothyronine sodium is the salt of T3 and is available in tablets and in an injectable form. • Absorption is nearly 100%, with peak serum levels 2–4 h following oral ingestion. • T1/2- 18-24 hours, requires BD/TID dosing • Strengths : 5/25/50 mcg tablets • Use: When more rapid onset of action is desired, • Myxedema coma • When preparing a patient with thyroid cancer for 131I therapy. Liothyronine 09-02-2021 Thyroid & Antithyroid Drugs 14
- 15. 09-02-2021 Thyroid & Antithyroid Drugs 15 • Requires multiple daily dosing • Expensive • Transient elevation of TSH • Tissues depending on local conversion of T3 – low intracellular T3. ATA – Long-term controlled clinical trials needed before routine use Disadvantages in exclusive T3 replacement
- 16. Mechanism of action Pharmacodynamics 09-02-2021 Thyroid & Antithyroid Drugs 16
- 17. • 10- 15% of the thyroxine treated patients: persistent symptoms • 3 meta-analysis : No advantage. • Other RCT’s : Improved compliance, weight reduction. • Genetic polymorphism • ATA and ETA guidelines: L-T4 remains the therapy of choice in hypothyroidism :lack of long-term safety data • Consider L-T4 and L-T3 as an experimental approach • L-T4 and L-T3 are not recommended in pregnancy and in patients with cardiac arrhythmias Liotrix : Combination of T3 &T4 09-02-2021 Thyroid & Antithyroid Drugs 17 De Castro JPW, et al. Differences in hypothalamic type 2 deiodinase ubiquitination explain localized sensitivity to thyroxine. J Clin Invest. 2015;125(2):769–81.
- 18. 09-02-2021 Thyroid & Antithyroid Drugs 18 • Armour Thyroid: natural, porcine-derived. (1 grain=60 mg=88 mcg of T4)) (Prothyroid, Novothyral, Thyreotom, Thyrolar-3, and Diotroxin) • A mixture of levothyroxine and T3 around 4:1 by weight and desiccated thyroid preparations with a similar T4:T3 ratio also are available. • Recent RCT: • No improvement in QOL • Increased weight loss Hoang TD, et al. Desiccated thyroid extract compared with levothyroxine in the treatment of hypothyroidism: a randomized, double- blind, crossover study. J Clin Endocrinol Metab. 2013;98: 1982–1990. )
- 19. • Absorption of levothyroxine is enhanced by a lower gastric pH. • Rationale: Studies have demonstrated that gastric acid secretion is at its circadian peak during the nighttime hours. • 2 out of 4 studies ; Significant decrease in TSH. Morning V/s bedtime dosages 09-02-2021 Thyroid & Antithyroid Drugs 19 Moore JG, Englert E Jr. Circadian rhythm of gastric acid secretion in man. Nature. 1970; 226:1261-2. Geer M, Potter DM, Ulrich H. Alternative schedules of levothyroxine administration. Am J Health Syst Pharm. 2015 Mar 1;72(5):373-7.
- 20. • Soft gel Capsules1 - T4 dissolved Glycerin with a gelatin capsule • Oral liquid Solution2 – Ethanol and glycerol (Tirosint-SOL) • TICO study • Change from tablet to liquid – normalisation of TSH • Switching back to tablets caused worsening of TSH Newer formulations 09-02-2021 Thyroid & Antithyroid Drugs 20 1. Fallahi P, Ferrari SM, Antonelli A. Oral L-thyroxine liquid versus tablet in patients with hypothyroidism without malabsorption: a prospective study. Endocrine. 2016 Jun;52(3):597-601. 2. Fallahi P, Ferrari SM, Ruffilli I, Antonelli A. Reversible normalisation of serum TSH levels in patients with autoimmune atrophic gastritis who received L-T4 in tablet form after switching to an oral liquid formulation: a case series. BMC Gastroenterol. 2016 Feb 24;16:22.
- 21. 09-02-2021 Thyroid & Antithyroid Drugs 21 Kashiwagura Y, Uchida S, Tanaka S, Watanabe H, Masuzawa M, Sasaki T, Namiki N. Clinical efficacy and pharmacokinetics of levothyroxine suppository in patients with hypothyroidism. Biol Pharm Bull. 2014;37(4):666-70. • Rectal Suppository • Low bioavailability • 1.8 times higher dose than tablet ✓ Alternative in situations like dysphagia
- 22. 09-02-2021 Thyroid & Antithyroid Drugs 22 Switching between formulations FDA’s methods of establishing bioequivalence is flawed!! ✓ AUC ✓ Cmax ⌦ TSH Endogenous factors that influence the Thyroxine bioavailability are not taken into account. Therefore, switching between the brands is not recommended.
- 23. Hypothyroidism 09-02-2021 Thyroid & Antithyroid Drugs 23 • Hypothyroidism is a clinical state resulting from underproduction of the thyroid hormones T4 and T3. • 95% are primary, 5% are secondary. • Most common cause - Iodine deficiency, Autoimmune disease Clinical Manifestations: Tiredness, weakness Dry skin Feeling cold Hair loss Difficulty concentrating Constipation Weight gain with poor appetite Dyspnea Hoarse voice Paresthesia Menstrual irregularities
- 24. Treatment 09-02-2021 Thyroid & Antithyroid Drugs 24 • Treatment is indicated in all symptomatic patients • Goal: Reduction of symptoms and prevention of long-term complications. Treatment is to be given lifelong. • Patients should be started on the full replacement dose of levothyroxine.
- 25. 09-02-2021 Thyroid & Antithyroid Drugs 25 • Adults age <50-60 years – • levothyroxine: 1.6 mcg/kg/day orally, • Adjust dose in increments of 12.5 to 25 micrograms to normalize TSH. • Pre-existing CAD or age >60 years – • 25-50 mcg orally once daily, • Adjust dose in increments of 12.5 to 25 micrograms every 6-8 weeks TSH should be measured 4 to 6 weeks after initiation of therapy or dosage change. Confirmed overt Primary Hypothyroidism
- 26. • Angina – initial high dose • Resistant hypothyroidism – Non adherence • Atrial fibrillation - overtreatment • Osteoporosis – overtreatment • Rarely, pseudotumor cerebri in children. Presentation appears to be idiosyncratic and occurs months after treatment has begun. Complications of Treatment 09-02-2021 Thyroid & Antithyroid Drugs 26 FDA warning : The use of thyroid hormones in the therapy of obesity, alone or combined with other drugs, is unjustified and has been shown to be ineffective.
- 27. • Incidence: 0.3% to 0.5% for overt hypothyroidism and 2% to 3% for subclinical hypothyroidism • Increased risk of adverse neonatal outcomes Preterm birth Low birth weight Increased perinatal morbidity and mortality. • Screening: Current thyroid therapy Personal/Family history of autoimmune thyroid disease , Goiter Previous delivery of infant with thyroid disease Type 1 diabetes mellitus Hypothyroidism in Pregnancy 09-02-2021 Thyroid & Antithyroid Drugs 27
- 28. 09-02-2021 Thyroid & Antithyroid Drugs 28 • Reference range for TSH lower: cross-reactivity of the alpha subunit of HCG with the TSH receptor. • Goal of TSH : less than 2.5 mIU/L during T1 less than 3.0 mIU/L during T2 & T3 After delivery, thyroxine doses typically return to prepregnancy levels • 20%-40% increase in thyroid hormone requirement: Increase in thyroid binding globulin Increased volume of distribution of thyroid hormone Placental transport and metabolism of maternal thyroxine
- 29. 09-02-2021 Thyroid & Antithyroid Drugs 29 All pregnant women should ingest approximately 250 mcg iodine daily. Women with a history or high risk of hypothyroidism: ✓ Euthyroid prior to conception ✓ Thyroid function Tests: ✓ Immediately after pregnancy is confirmed ✓ every 4 weeks during the first half of the pregnancy ✓ less frequent testing after 20 weeks’ gestation
- 30. • Cretinism: Most common treatable cause of mental retardation. • May be transient, but permanent in majority. • Neonatal Hypothyroidism • Thyroid gland dysgenesis – 80-85% • Inborn errors of metabolism – 10- 15% • TSH-R antibody mediated – 5% • Neonatal screening – TSH and T4 in heel prick blood • Treatment should be started at L-T4 dose of 10 –15 µg/kg/d Hypothyroidism In childhood 09-02-2021 Thyroid & Antithyroid Drugs 30
- 31. • Mortality rate : 20% - 40% • Common precipitating factors : Hypothermia, Infections (particularly influenza, pneumonia, and sepsis), trauma Drugs (sedatives, anesthetics, antidepressants) • Manifestations: Depression of cerebral function, Hypothermia hyponatremia, hypoglycemia, respiratory acidosis Low cardiac output, water retention – hypoxia, hypercapnia, may lead to respiratory failure and coma. Myxedema Coma 09-02-2021 Thyroid & Antithyroid Drugs 31
- 32. 09-02-2021 Thyroid & Antithyroid Drugs 32 ✓ Thyroid hormone replacement ✓ Levothyroxine : Loading dose -500 µg IV bolus → 50–100 μg/d. (nasogastric) ✓ Liothyronine IV or nasogastric 10 to 25 μg every 8–12 h ✓ Supportive measures: ✓ O2 and mechanical ventilation ✓ Administration of iv fluids (5%–10% glucose in isotonic NaCl solution resuscitation plus hydrocortisone; ✓ Hypothermia: External warming ✓ Hypoglycemia: Managed with dextrose infusion ✓ Hyponatremia may be treated with saline solution and loop diuretics ✓ Parenteral hydrocortisone (50 mg every 6 h)
- 33. • Subclinical hypothyroidism is a state of usually asymptomatic, mild thyroid failure, with normal levels of T4 and T3, and minimal elevation of TSH. • No universally accepted recommendations • Treatment indicated when: ✓ Woman who is pregnant or wishes to conceive ✓ When TSH > 10 mIU/L. ✓ Elderly patients Subclinical Hypothyroidism 09-02-2021 Thyroid & Antithyroid Drugs 33
- 34. 09-02-2021 Thyroid & Antithyroid Drugs 34 • Start with – Levothyroxine 1 microgram/kg/day orally (usual dose 25–50 μg/d) • Adjust dose in increments of 25 to 50 micrograms to normalize TSH • If levothyroxine is not given, thyroid function should be evaluated annually. Replacement when TSH < 10 mIU/L, ✓ Symptoms suggestive of hypothyroidism, ✓ Positive TPO antibodies ✓ Any evidence of heart disease.
- 35. Thyroid & Antithyroid Drugs 35 09-02-2021 Anti-thyroid Drugs
- 36. 09-02-2021 Thyroid & Antithyroid Drugs 36 Anti-thyroid drugs Ionic Inhibitors Potassium perchlorate Potassium Thiocyanate Thioamide derivatives Propylthio uracil Carbimaz ole Methimaz ole Radioactive iodine 131I Iodides Lugols solution Release Inhibitors Synthesis Inhibitors SSKI: Saturated Solution of KI
- 37. Propylthiouracil, Methimazole, Carbimazole Mechanism of action Thionamides 09-02-2021 Thyroid & Antithyroid Drugs 37 Iodination Coupling • Inhibition of hormone synthesis • Depletion of the Iodinated Tg • Also reduce thyroid antibody levels – mechanism unclear • PTU – Blocks peripheral conversion of T4 to T3
- 38. 09-02-2021 Thyroid & Antithyroid Drugs 38 Pharmacological properties Propylthiouracil Carbimazole Plasma protein binding ~75% Nil Plasma t1/2 1-2.5 ~6–9 h Urinary excretion 35% 10% Concentrated in thyroid Yes Yes Metabolism of drug: Severe liver disease Severe kidney disease Normal Normal Decreased Normal Dosing frequency 1–4 times daily Once or twice daily Transplacental passage Low Low Levels in breast milk Low Low
- 39. Initial Dose: • 100-200 mg every 6-8 hours Maintenance: • 50 -100 mg Initial Dose: • 10-20 mg every 8-12 hours Maintenance: • 2.5 – 10 mg 09-02-2021 Thyroid & Antithyroid Drugs 39 Titration Regimen Propylthiouracil Methimazole/Carbimazole ✓ Reviewed after 4–6 weeks and the dose is titrated based on unbound T4 levels. ✓ TSH – not a sensitive marker for dose titration ✓ Response in 6-8 weeks
- 40. • Initial doses of anti-thyroid drug is continued • T4 is adjusted for normal unbound T4 levels. Remission rates: • Titration regimen: Maximum remission rates (up to 30–60% in some populations) are achieved by 12–18 months. • Block-replace regimen: By 6 months. • In case of relapse, RAI is the treatment of choice. All patients should be followed closely for relapse during the first year after treatment and at least annually thereafter. 09-02-2021 Thyroid & Antithyroid Drugs 40 Block & Replace Regimen
- 41. 09-02-2021 Thyroid & Antithyroid Drugs 41 Untoward Reactions of Thionamides • Incidence of side effects with both drugs is low. • Most common reaction: mild urticarial papular rash • Agranulocytosis – most serious reaction • First few weeks of therapy • Periodic monitoring of counts is not useful • Reversible • Instructions to patients • Carbimazole- Congenital anomalies • Others – pain and stiffness in joints, paresthesias, Drug fever, Nephritis. • Vasculitis: Antineutrophilic cytoplasmic anti-bodies (ANCA); PTU>Methimazole
- 42. 09-02-2021 Thyroid & Antithyroid Drugs 42 ! FDA Black Box warning ! From 1969, !! 34 cases of severe liver injury with propylthiouracil !! 15 deaths, 12 liver transplantations On April 21, 2010, after 63 years clinical use – Black box warning for the label of PTU. Methimazole : 5 cases of severe liver injury
- 43. • Oldest remedy, also quickest. • MOA: • Inhibition of hormone release • Acute and transient inhibition of synthesis (Wolf-Chaikoff effect) • Decrease the size and vascularity of the gland • Dose: • Lugol solution- 16-36mg (2-6 drops of 5% - 10% soln) TID • SSKI: 50-100 mg (1-2 drops) TID Thyroshield: In radiation emergency, adult dose is 2 mL (130 mg) every 24 h. Surgical preparation Iodides 09-02-2021 Thyroid & Antithyroid Drugs 43 Logols Iodine and Saturated Solution of Potassium Iodide Pregnancy
- 44. • MOA: Competitive inhibition of NIS. (Iodide entry) • Dose : potassium perchlorate – 600-800 mg , maintenance dose- 200-400 mg daily. • Perchlorate causes nephrotic syndrome and fatal aplastic anemia. • Indications: • Used in patients allergic to thionamides. • Amiodarone induced Thyrotoxicosis Ion Inhibitors 09-02-2021 Thyroid & Antithyroid Drugs 44 Potassium Thiocyanate, Potassium perchlorate
- 45. 09-02-2021 Thyroid & Antithyroid Drugs 45 Acute effects: • Angioedema, Laryngeal edema – Suffocation • Thrombotic thrombocytopenic purpura & fatal periarteritis nodosa Chronic Intoxication: • Iodism- Brassy taste, burning of mouth and throat. • Increased salivation, coryza, swelling of eyes • Parotid & submaxillary gland enlargement –Mumps parotitis • Rarely, fatal eruptions – Ioderma Symptoms disappear within few days of stopping the drug Untoward Reactions of Iodine therapy
- 46. • Isotopes – 123I and 131I (Stable isotope- 127 I) • 123I is a short-lived 𝛄-emitter with a t1/2 of 13 h; diagnostic studies. • 131I has a t1/2 of 8 days and emits both 𝛄 rays and β particles. used therapeutically for, • Destruction of an overactive or enlarged thyroid • Thyroid cancer for thyroid ablation and treatment of metastatic disease. • Dose – 10-15 mCi Radioactive Iodine 09-02-2021 Thyroid & Antithyroid Drugs 46
- 47. 09-02-2021 Thyroid & Antithyroid Drugs 47 Indications • Comorbidities increasing surgical risk • Previously operated or externally irradiated necks • lack of access to a high- volume thyroid surgeon • patients with contraindications to ATD use • Cardiovascular risk factors Contraindications • Pregnancy is strictly contraindicated. Conception safe after 6 months. • Nursing mothers • Children - Relative
- 48. 09-02-2021 Thyroid & Antithyroid Drugs 48 Incorporates into the thyroid hormones and Thyroglobulin • Follicles – Necrosis; bizarre cell forms and nuclear pyknosis • Destruction of small vessels • Edema and fibrosis of the interstitial tissue Mechanism of action of RAI After few weeks
- 49. • Beta blockers • Iodides – 3 to 7 days after RAI. • Prior therapy of ATD’s. • Lithium – High rate of cure, fast response and prevention of post-treatment hormone release. • Glucocorticoids – Thyroid ophthalmopathy1 Role of Adjunctive therapy with RAI 09-02-2021 Thyroid & Antithyroid Drugs 49 Bartalena L, Marcocci C, Bogazzi F, et al. Relation between therapy for hyperthyroidism and the course of Grave’s ophthalmopathy. N Engl J Med 1998;338(2): 73-78.
- 50. 09-02-2021 Thyroid & Antithyroid Drugs 50 • Acute effects: mild tenderness and dysphagia • High incidence of delayed hypothyroidism • Slight increase in cancer stomach, kidney, and breast. • Radiation thyroiditis/thyrotoxic crisis • Exaggeration of Thyroid Ophthalmopathy - Prednisone, 40 mg/d, at the time of radioiodine treatment, tapered over 6– 12 weeks. • Alterations in reproductive function Sioka C, Totopoulos A. Effects of I-131 therapy on gonads and pregnancy outcome in patients with thyroid cancer. Fertil Steril 2011. 95:1552-9. Complications of Radioiodine
- 51. • Condition of excess thyroid function. • Thyrotoxicosis is defined as the state of thyroid hormone excess and is not synonymous with hyperthyroidism. • Common causes of primary hyperthyroidism are: Graves Disease(60-80%) Toxic multinodular goiter Toxic adenoma Thyroid carcinoma Hyperthyroidism 09-02-2021 Thyroid & Antithyroid Drugs 51
- 52. 09-02-2021 Thyroid & Antithyroid Drugs 52 Clinical features Hyperactivity, irritability, Dysphoria Heat intolerance Palpitations Fatigue Diagnosis: Clinical + Laboratory Subnormal (TSH) + ↑↑ T3 +/ T4. Weight loss with increased appetite Diarrhea Polyuria Oligomenorrhea loss of libido. Treatment options: 1. Antithyroid drugs 2. Radioactive iodine 3. Surgery
- 53. 09-02-2021 Thyroid & Antithyroid Drugs 53 Beta Blockers In an RCT with Methimazole alone v/s Methimazole + Beta blockers After 4 weeks of therapy, ✓ Lower heart rate ✓ Less shortness of breath and fatigue ✓ Imroved score on SF-36 questionnaire Propranolol – 10-40 mg TID is preferred. If Beta blckers are contraindicated, ✓ Calcium channel blockers Tagami T, Yambe Y, Tanaka T,et al. BBGD Study Group. Short- term effects of beta- adrenergic antagonists and methimazole in new-onset thyrotoxicosis caused by Graves’ disease. In- tern Med. 2012; 51:2285–2290
- 54. Subclinical Hyperthyroidism 09-02-2021 Thyroid & Antithyroid Drugs 54 When to treat? • TSH Below lower limit of reference range with normal T3,T4. • Risk of atrial fibrillation and all cause mortality. • Increased hip fractures in postmenopausal women • >65 yreas whem TSH <0.1 mIU • <65 years – Depends on CVS risk factors. • ATD’s are preferred.
- 55. • Hyperthyroidism is less common than hypothyroidism, with an approximate incidence of 0.2%. • Graves disease: • Exacerbation in T1. • Monthly Fetal USG. • Thyroid autoantibodies – should be measured at end of T2. Hyperthyroidism in Pregnancy 09-02-2021 Thyroid & Antithyroid Drugs 55 1. Carney LA, Quinlan JD, West JM. Thyroid disease in pregnancy. Am Fam Physician. 2014 Feb 15;89(4):273-8. Subclinical : One large prospective study of more than 25,000 pregnant women with subclinical hyperthyroidism showed no increase in adverse pregnancy outcomes; therefore, treatment is not recommended in these cases.1
- 56. 09-02-2021 Thyroid & Antithyroid Drugs 56 • Lowest possible dose of antithyroid drugs should be used. • The goal of treatment is a serum free T4 level at, or moderately above the normal range for pregnancy. • First trimester: PTU • Second Trimester: Carbimazole/methimazole • If discontinued because of side effects: second-trimester thyroidectomy is the only other option for symptomatic patients. • Radioactive iodine is contraindicated in pregnancy. Choice of therapy in pregnancy
- 57. • TFT should be monitored 3 months after initiation and 3 monthly thereafter. • AIT type 1: Iodine induced excessive thyroid hormone synthesis, especially in patients with underlying thyroid disease. • AIT type 2: destructive thyroiditis in previously normal thyroid gland with release of thyroid hormones into circulation • Unresponsive: Thyroidectomy Amiodarone Induced Thyrotoxicosis 09-02-2021 Thyroid & Antithyroid Drugs 57 Rx Carbimazole Rx Corticosteroids
- 58. Choice of therapy ✓ Remission possible; Carbimazole therapy for 1 year is first-line of choice. Dose :0.2–0.5 mg/kg daily. Majority of pediatric patients with GD will eventually require either RAI or surgery. Hyperthyroidism in Children 09-02-2021 Thyroid & Antithyroid Drugs 58 If remission is not achieved after a course of therapy with ATDs, RAI or surgery should be considered. Or ATD therapy may be continued long term or until the child is considered old enough for surgery or RAI.
- 59. 09-02-2021 Thyroid & Antithyroid Drugs 59 Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. 2016 Oct;26(10):1343-1421. ✓ RAI • Should be avoided in <5 yrs • 5-10 yrs – The calculated activity is <10 mCi. ❑ No evidence suggests that children or adults treated for GD with more than 150 µCi/g (5.55 MBq/g) of RAI have an increased risk of thyroid cancer directly attributable to RAI. ❑ If a small risk exists, a sample size of more than 10,000 children who were treated at <10 years of age would be needed to identify the risk, likely exceeding the number of such treated children. ✓ Thyroidectomy Definitive treatment:
- 60. • Sudden severe exacerbation of hyperthyroidism. • Precipitating factors: Stress Infection Following radio iodine Trauma Pregnancy. Thyroid Storm 09-02-2021 Thyroid & Antithyroid Drugs 60 • Clinical features: Hyperthermia Tachycardia Delirium Hypotension Vomiting Diarrhoea Mortality rate: 30%, due to cardiac failure, arrhythmia, or hyperthermia
- 61. 09-02-2021 Thyroid & Antithyroid Drugs 61 Management of thyroid storm ✓ Intensive monitoring and supportive care ✓ Treat precipitating cause ✓ Reduce Thyroid hormone synthesis ➢Propylthiouracil (500–1000 mg loading dose → 250 mg every 4 hrly orally or by nasogastric tube or per rectum; ➢Methimazole can be used in doses up to 30 mg 12 hrly ➢5 drops SSKI every 6 h /ipodate or iopanoic acid (500 mg per 12 h) / Sodium iodide, 0.25 g IV every 6 h ✓ Propranolol 60–80 mg PO every 4 h; or 2 mg IV every 4 h ✓ Hydrocortisone 300 mg IV bolus, then 100 mg every 8 h ✓ Antibiotics if infection is present ✓ Oxygen, IV fluids
- 62. Thyroid Hormones in Non-thyroidal illness 09-02-2021 Thyroid & Antithyroid Drugs 62
- 63. • Thyromimetics : Subtype selective, potent TR agonists and antagonists. • Sobetirome: Selective for TRb1. • It preferentially accumulates in liver. • Experimental data: It reduced LDL-cholesterol, fat mass and hepatic steatosis without increasing heart rate . • Sobetirome achieved orphan drug status for X-linked adrenoleukodystrophy. (VLCFA accumulation) Thyroid hormones in Dyslipidemia 09-02-2021 Thyroid & Antithyroid Drugs 63 Hartley MD, Kirkemo LL, Banerji T, Scanlan TS. A Thyroid Hormone-Based Strategy for Correcting the Biochemical Abnormality in X-Linked Adrenoleukodystrophy. Endocrinology. 2017 May 1;158(5):1328-1338.
- 64. • Depression is associated with neuronal death. • T3 increases gene expression by increasing levels of TRH,CRH and BDNF. • Increased levels of 5-HT levels. • STAR*D trial – T3 better than lithium in augentation of antidepresent effect. T3 in Depression 09-02-2021 Thyroid & Antithyroid Drugs 64 Nierenberg AA, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006 Sep;163(9):1519-30.
- 65. 09-02-2021 Thyroid & Antithyroid Drugs 65 Garlow SJ, Dunlop BW, Ninan PT,et al. The combination of triiodothyronine (T3) and sertraline is not superior to sertraline monotherapy in the treatment of major depressive disorder. J Psychiatr Res. 2012 Nov;46(11):1406-13. • 8 week Double blind ,RCT of 153 patients between 18 and 60 yrs with DSM-IV Major depressive disorder. ---No difference in the treatment arm
- 66. 09-02-2021 Thyroid & Antithyroid Drugs 66 Touma KTB, Zoucha AM, Scarff JR. Liothyronine for Depression: A Review and Guidance for Safety Monitoring. Innov Clin Neurosci. 2017 Apr 1;14(3-4):24-29. • Most trials were published earlier than 10 years ago • Small samples of patients, and there are limited data available for liothyronine’s efficacy with newer antidepressants • Larger studies of longer duration are needed to evaluate T3’s efficacy with newer and other classes of antidepressants.
- 67. Summary 09-02-2021 Thyroid & Antithyroid Drugs 67 ✓ Hypothyroidism is most often due to iodine deficiency or autoimmune disorder known as Hashimoto’s thyroiditis. ✓ The drug of choice for replacement therapy in hypothyroidism is levothyroxine. ✓ Studies of combination therapy with levothyroxine and liothyronine have not shown reproducible benefits. This approach to treatment requires further study. ✓ Monitoring therapy is achieved by observing clinical signs and symptoms and by measuring the serum TSH level.
- 68. 09-02-2021 Thyroid & Antithyroid Drugs 68 ✓ Hyperthyroidism may be treated with antithyroid drugs such as Carbimazole or propylthiouracil, radioactive iodine (RAI) or surgical removal of the thyroid gland; ✓ Selection of the initial treatment approach is based on patient characteristics such as age, concurrent physiology (eg, pregnancy), comorbidities (eg, chronic obstructive lung disease), and convenience. ✓ Response to MMI and PTU is seen in 4 to 6 weeks and therefore β-blocker therapy may be concurrently initiated to reduce adrenergic symptoms. ✓ Therapy is monitored by clinical signs and symptoms and by measuring the serum concentrations of TSH and free thyroxine (T4).
- 69. 09-02-2021 Thyroid & Antithyroid Drugs 69 ✓ Adjunctive therapy with β-blockers controls the adrenergic symptoms of thyrotoxicosis; iodine may also be used adjunctively in preparation for surgery and acutely for thyroid storm. ✓ Many patients choose to have ablative therapy with 131I rather than undergo repeated courses of ATD treatment; most patients receiving RAI eventually become hypothyroid and require thyroid hormone supplementation