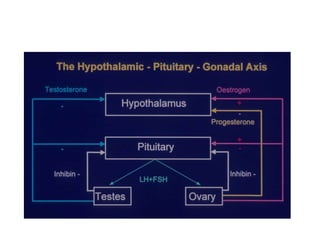
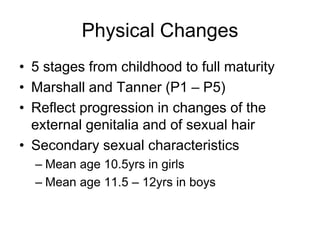
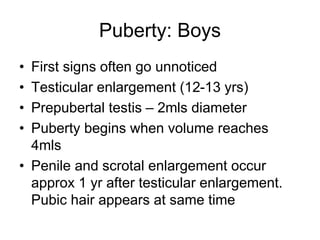
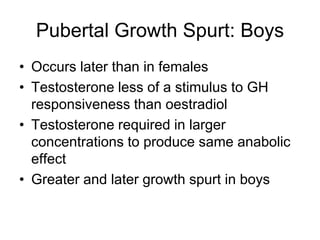
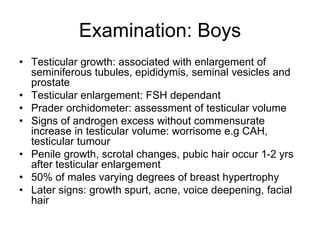
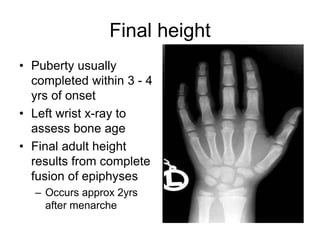
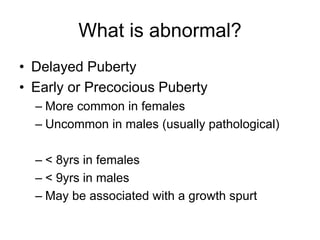
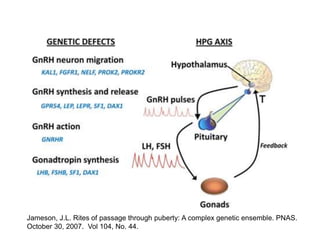
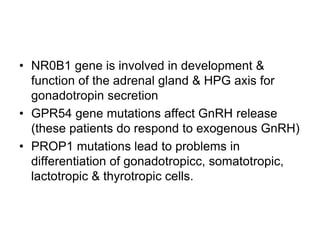
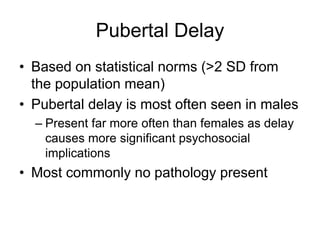
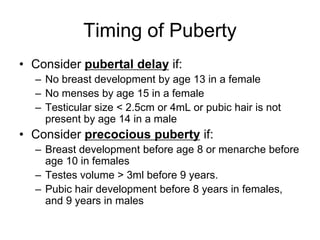
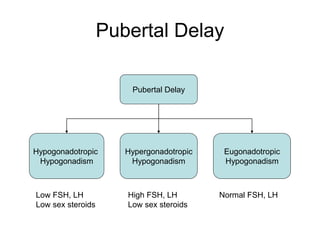
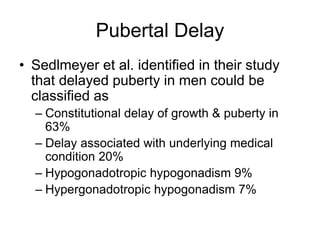
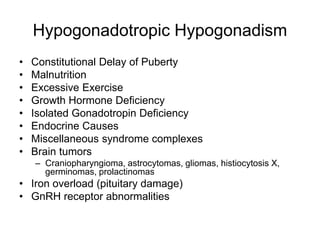
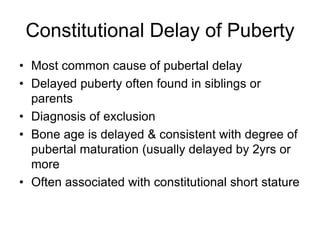
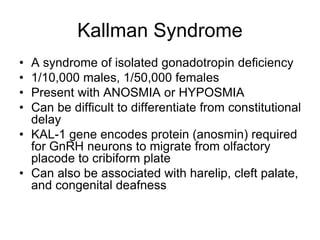
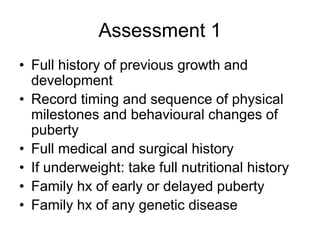
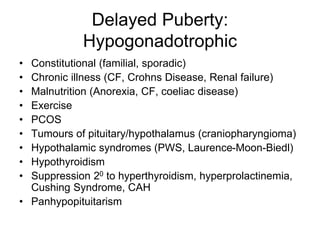
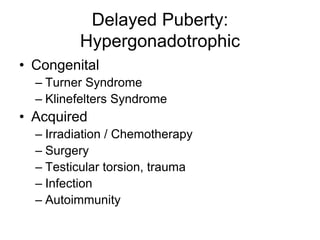
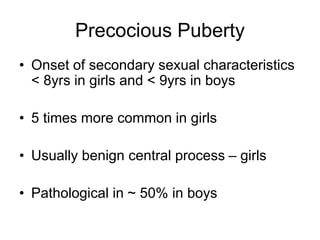
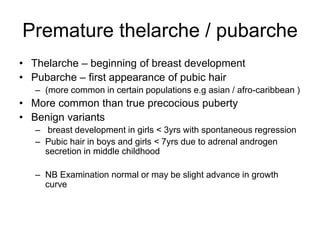
Puberty is controlled by the hypothalamic-pituitary-gonadal axis. Normal puberty occurs between ages 8-14 in girls and 9-14 in boys. It involves physical changes like growth spurts and development of secondary sex characteristics. Abnormal puberty can be delayed or precocious. Delayed puberty is usually due to constitutional factors but may have underlying causes. Genetic factors influence the timing of puberty.