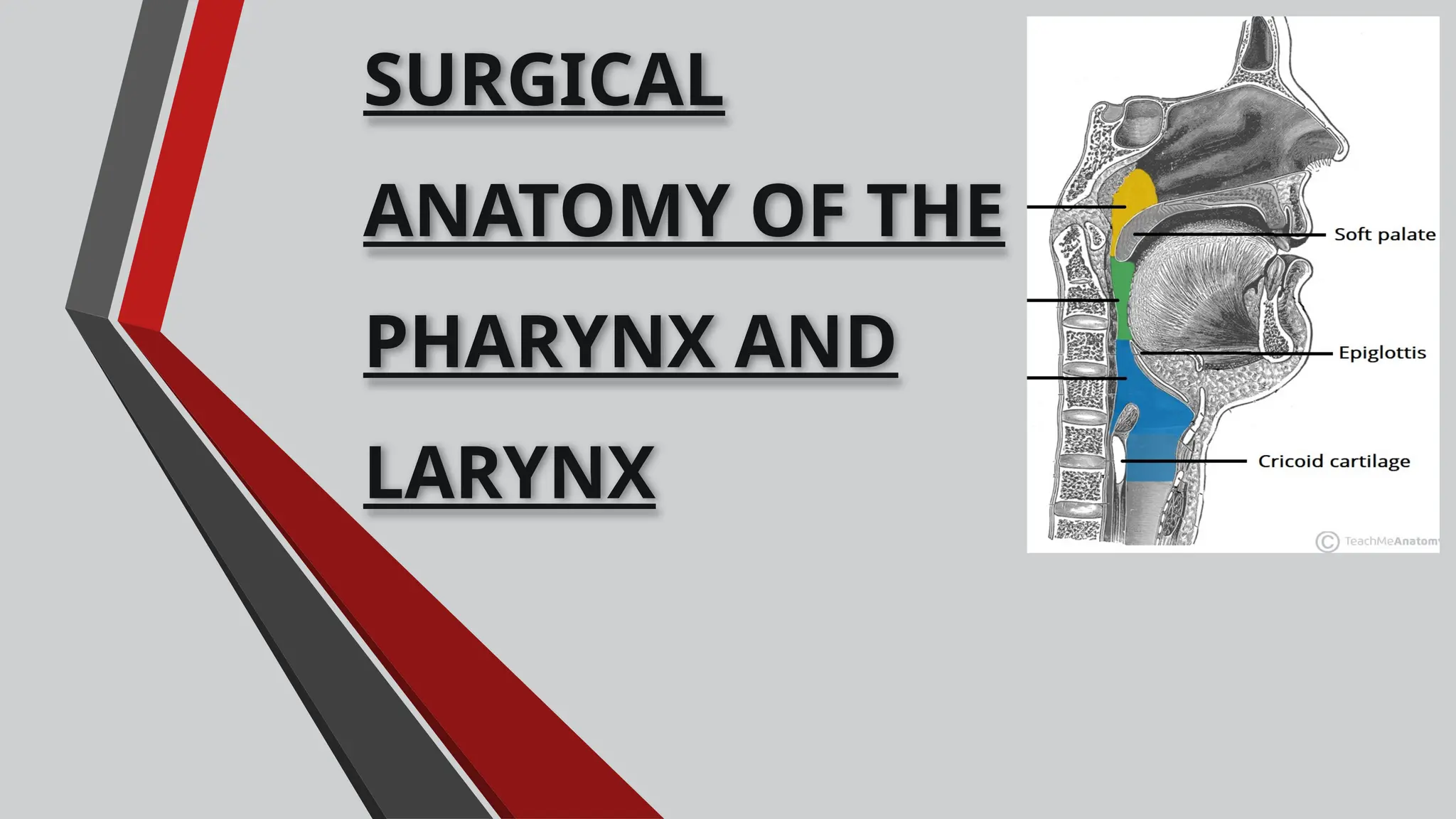
The document provides a comprehensive overview of the surgical anatomy of the pharynx and larynx, including their embryology, structure, and physiological functions. It details the anatomy and function of various anatomical components such as the walls of the pharynx, cartilages of the larynx, and their associated muscles, blood supply, and nerve innervation. Additionally, the document addresses applied clinical aspects including developmental anomalies and airway management techniques.