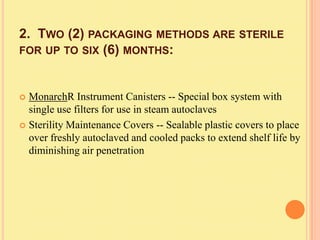
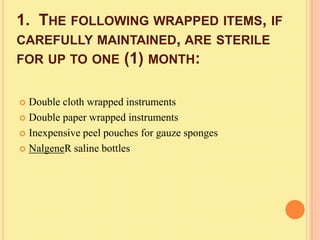
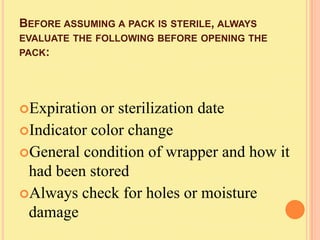
This document discusses sterilization methods for infection control in medical offices. It states that instrument sterilization is an important part of infection control. The main sterilization methods discussed are steam under pressure, dry heat, chemical vapor, and ethylene oxide gas. It provides details on cleaning, packaging, and monitoring instruments to ensure effective sterilization. Biological indicators that test for microbial kill are emphasized as the ultimate criteria for verifying sterilization.