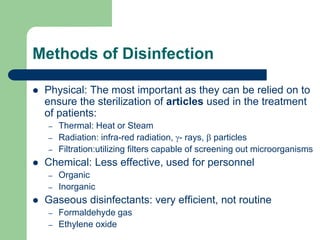
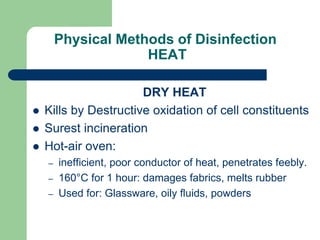
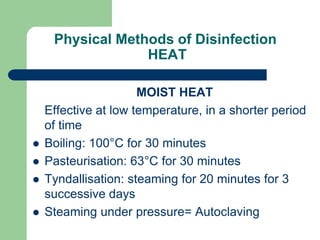
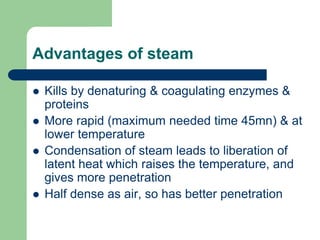
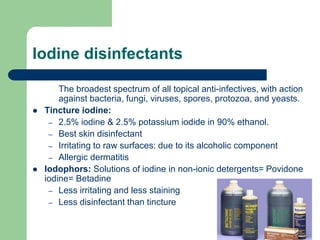
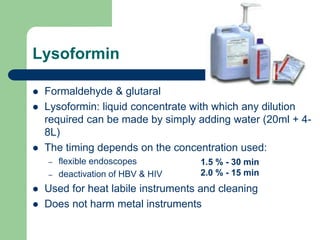
The document discusses sterilization and disinfection, outlining methods such as physical (heat, radiation, filtration) and chemical (inorganic, organic agents) approaches. It emphasizes the importance of surgical disinfection processes, particularly high-risk items, and details the operation and effectiveness of autoclaves. Additionally, it provides guidelines for chemical disinfectants, their actions, and standards for surgical scrubbing, gowning, and gloving.