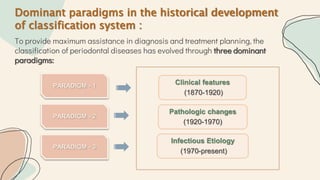
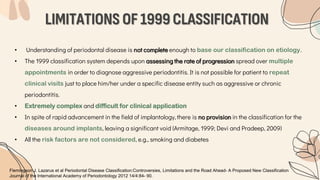
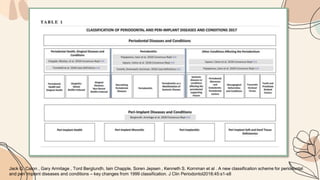
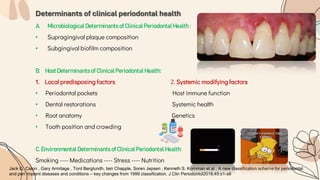
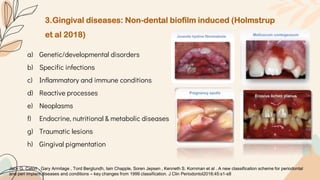
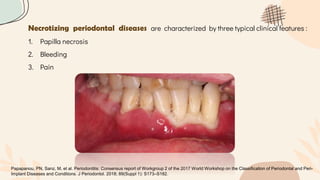
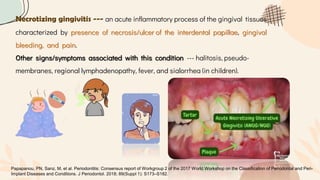
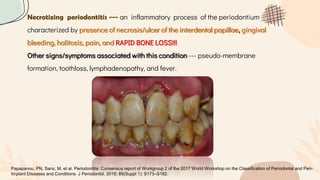
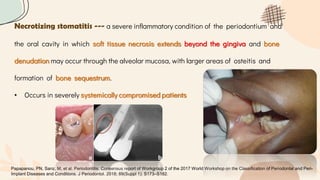
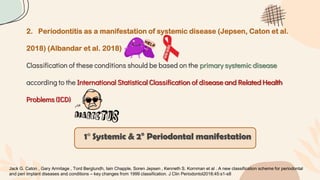
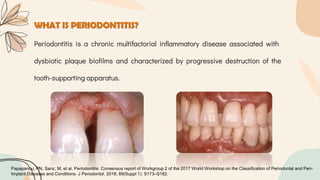
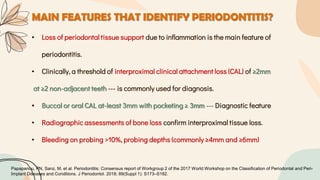
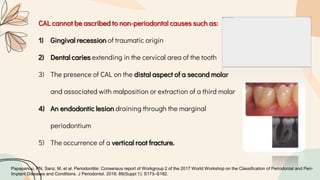
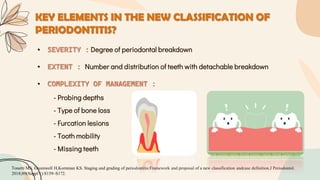
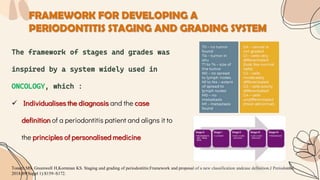
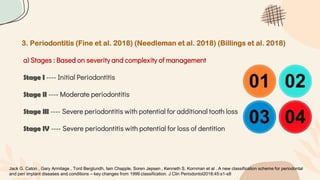
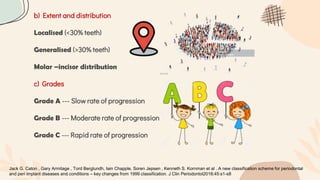
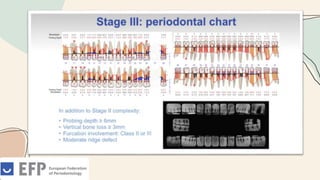
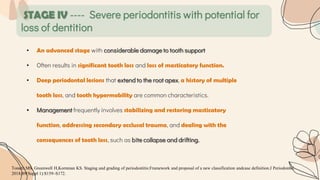
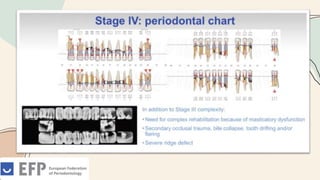
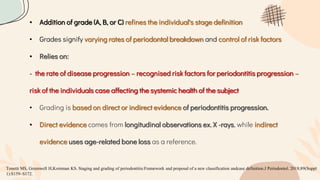
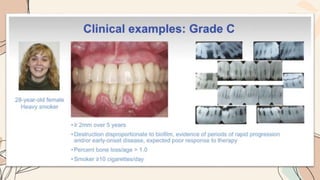
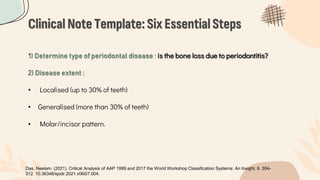
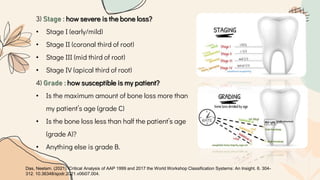
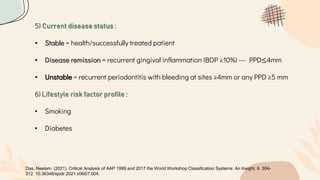
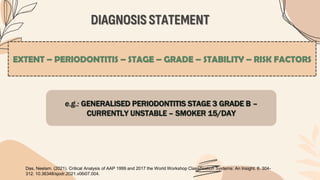
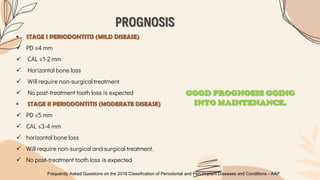
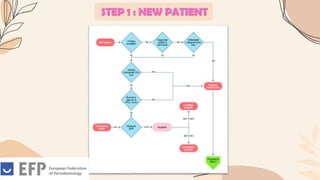
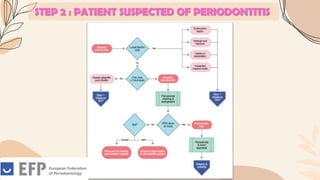
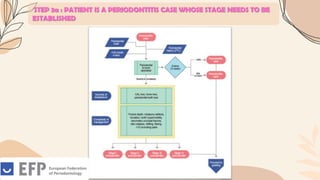
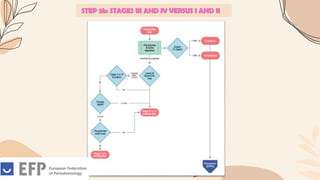
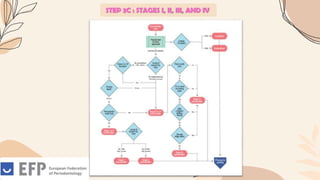
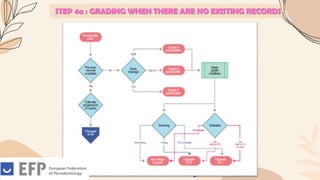
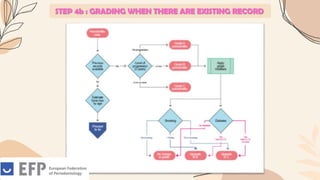
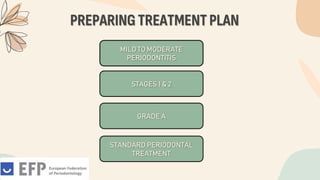
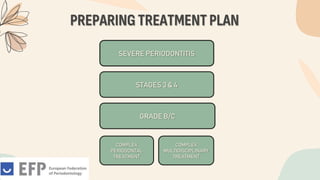
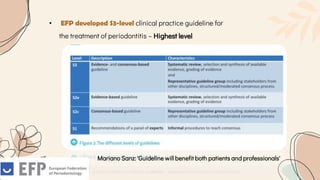
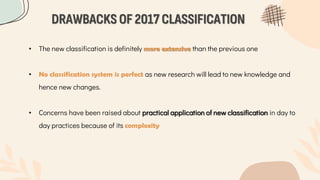
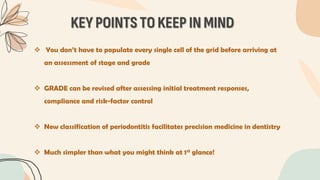
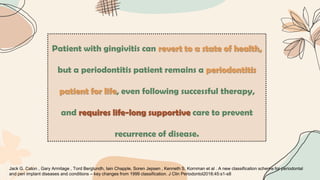
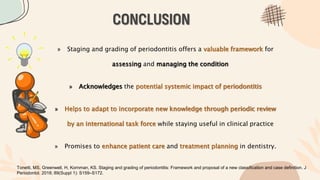
This document discusses the 2017 classification of periodontal and peri-implant diseases. It begins with introducing classifications and their importance. It then discusses the historical aspects and limitations of previous classifications from 1999. The highlights of the new 2017 classification are presented, which was developed by an international workshop with 130 experts. The new classification has four main categories: I) Periodontal health, gingivitis and gingival conditions, II) Periodontitis, III) Necrotizing periodontal diseases, and IV) Periodontitis as a manifestation of systemic diseases. Key aspects of the new classification are staging and grading of periodontitis to better aid in diagnosis, prognosis and treatment planning.