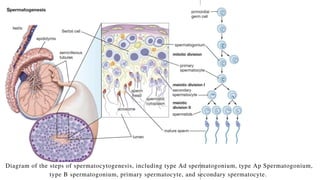
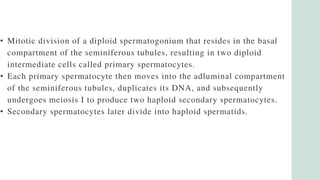
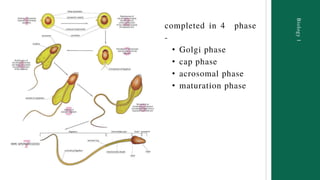
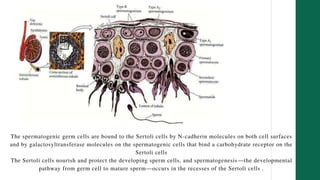
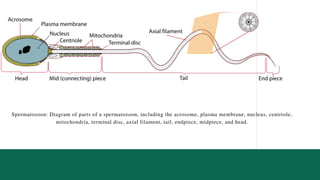
The presentation on spermatogenesis discusses the anatomy and physiology of male reproduction, outlining the steps involved in the production of mature spermatozoa from primordial germ cells. It emphasizes the importance of hormonal regulation, environmental factors, and the role of Sertoli cells in nourishing and protecting developing sperm. Additionally, it highlights factors affecting spermatogenesis, such as temperature and dietary deficiencies.