This document provides an overview of spinal cord injury (SCI), including its definition, epidemiology, clinical presentation, diagnosis, management, and physical therapy approaches. Some key points:
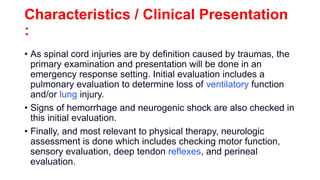
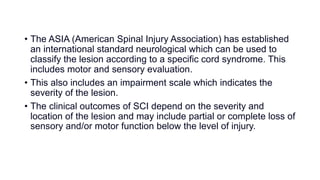
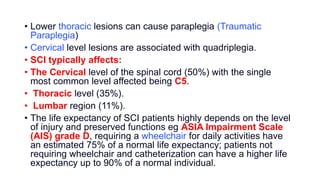
- SCI results from traumatic damage to the spinal cord or nerves and affects sensory and motor function below the site of injury. Injuries can be complete or incomplete.
- Over 12,500 new SCI cases occur annually in North America, primarily in young adults and older adults. Common causes include vehicle accidents, falls, and sports injuries.
- Physical therapy management depends on the level and completeness of injury, and may include respiratory training, strength exercises, and gait training with braces or walkers. The goal is to