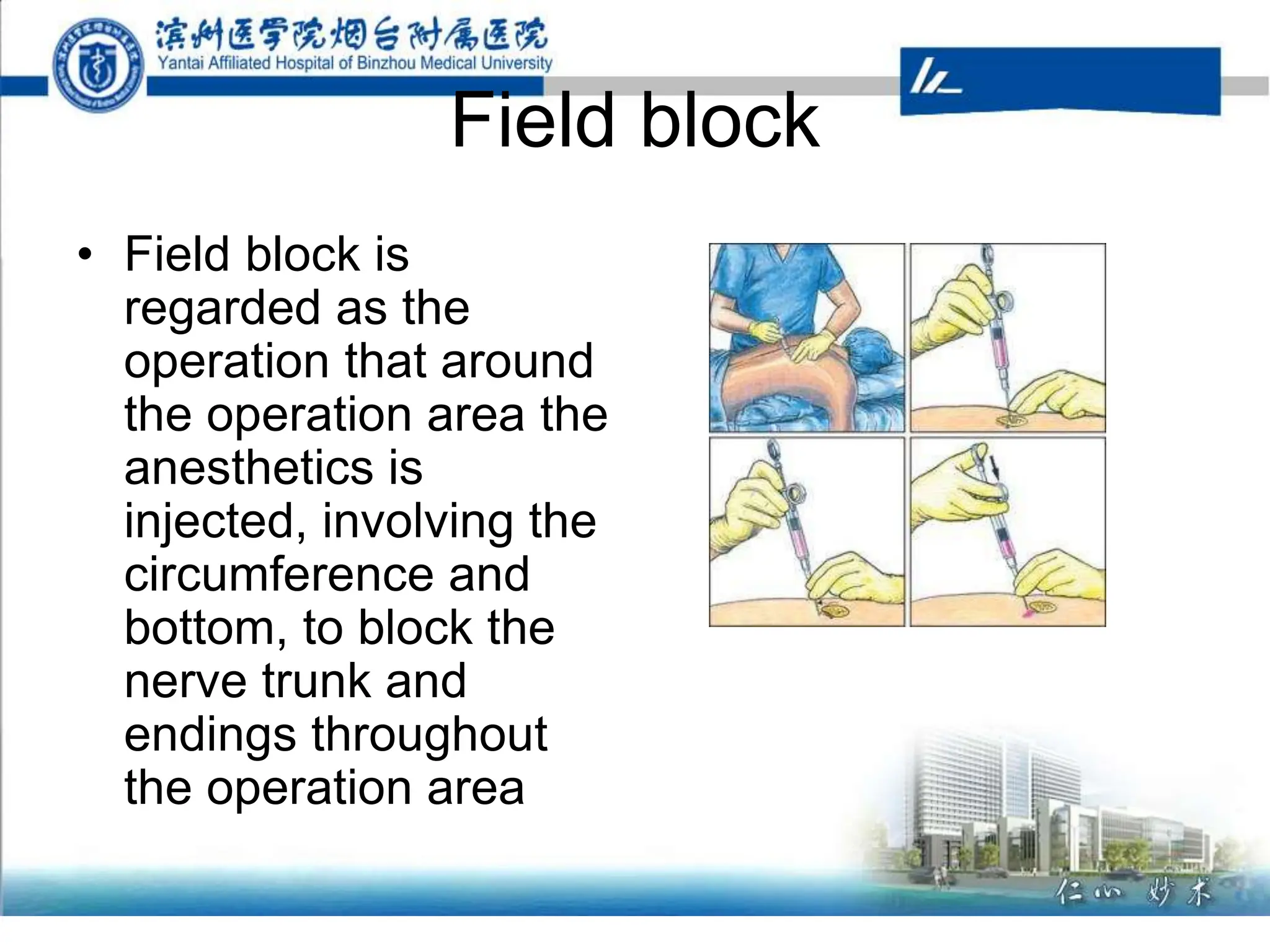
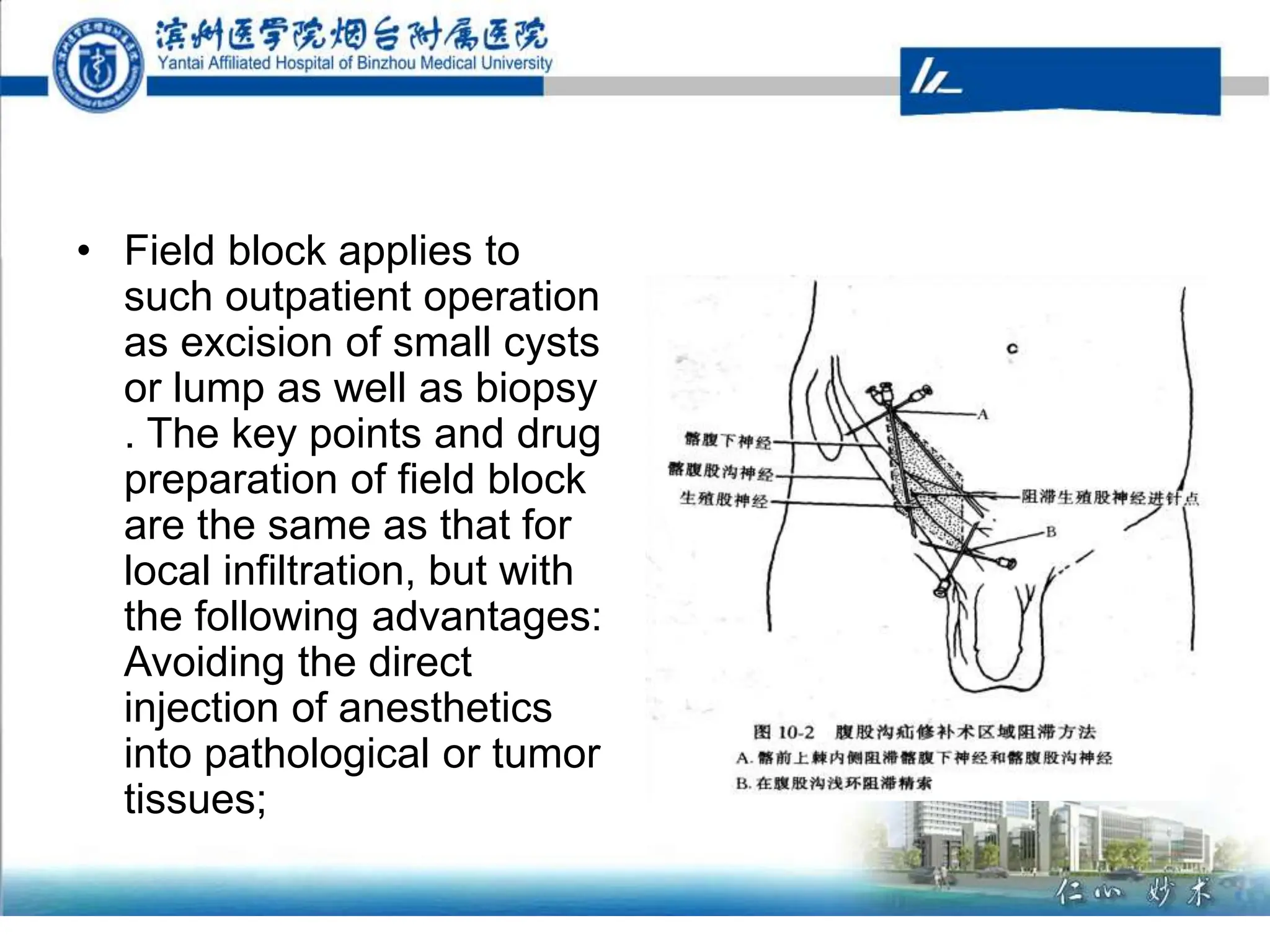
Regional anesthesia techniques include topical anesthesia, local infiltration, field block, and nerve blockade. Common nerve blockades are brachial plexus and sciatic nerve blocks, as well as epidural and spinal analgesia. The greatest risk is local anesthetic toxicity from accidental intravascular injection or excessive dosing. Symptoms involve the central nervous system and treatments focus on supportive care, sedation, and ventilation support if needed. Proper technique and cautious dosing can help prevent local anesthetic toxicity risks.