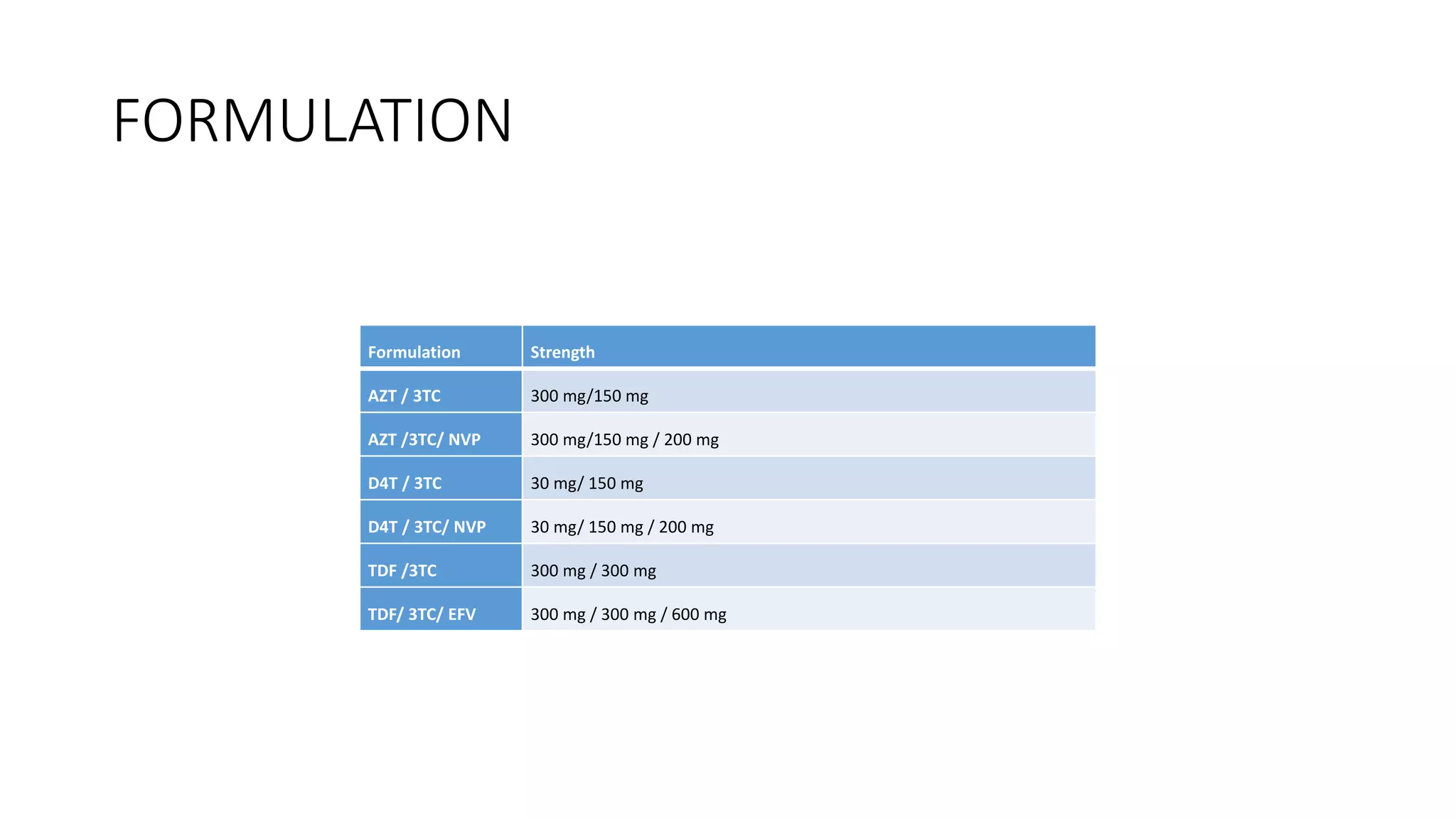
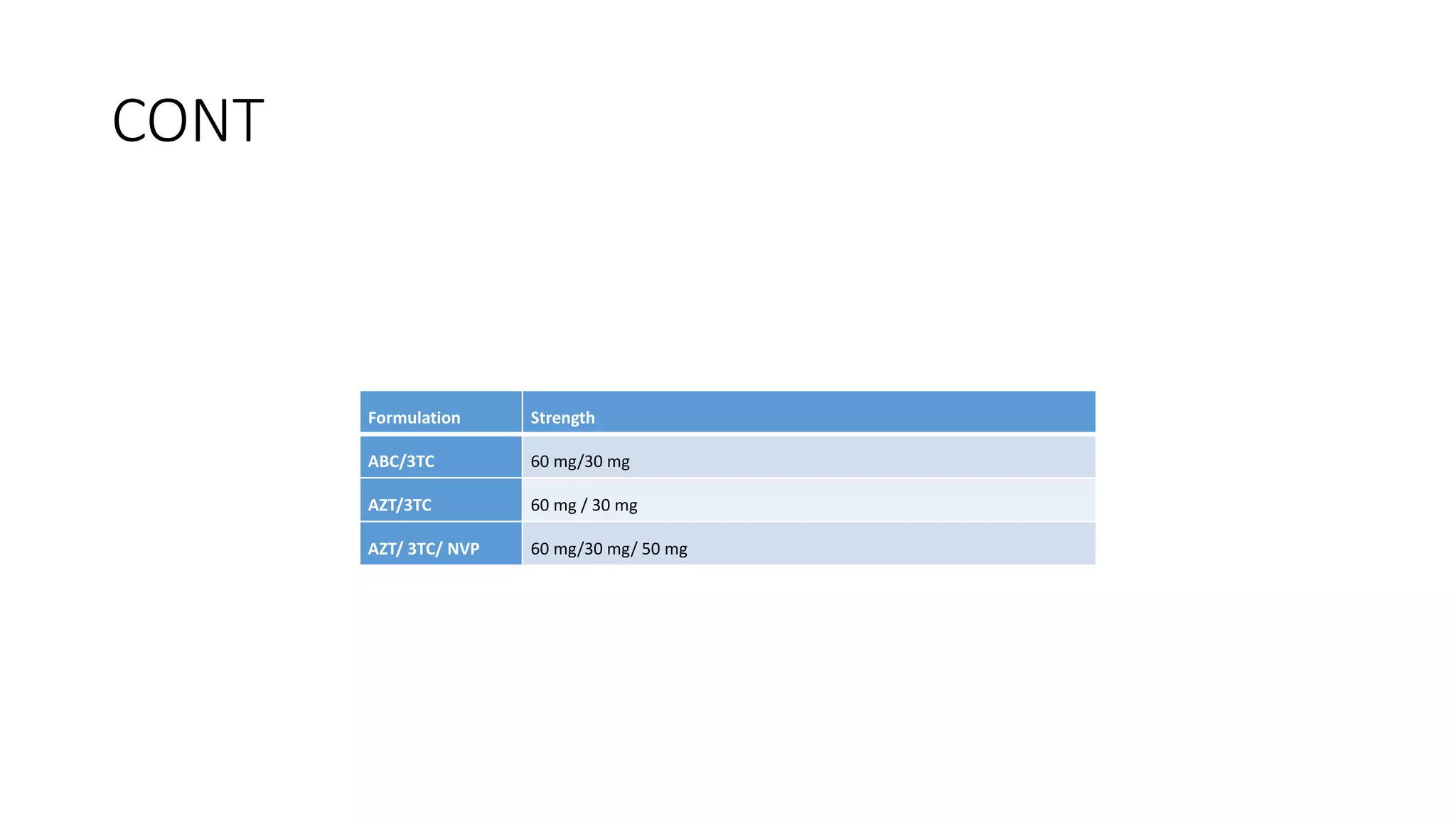
This document discusses HIV/AIDS, including that HIV is a retrovirus with two types that cause AIDS through different transmission methods. It then summarizes the virus lifecycle and the classes of antiretroviral drugs that target different stages of the viral lifecycle, including nucleoside/nucleotide reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, protease inhibitors, entry inhibitors, CCR5 receptor antagonists, and integrase strand transfer inhibitors.