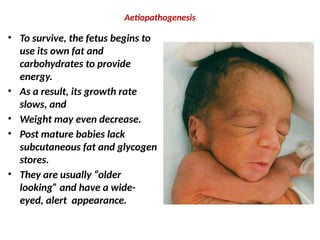
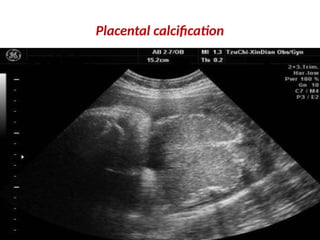
Post-maturity refers to newborns delivered after 42 weeks of gestation, impacting less than 6% of all births. The condition is associated with risks such as fetal malnutrition due to aging placenta and may lead to complications for both mother and baby, including hypoglycemia and the need for assisted deliveries. Monitoring and potential induced labor are recommended strategies to manage post-mature pregnancies effectively.