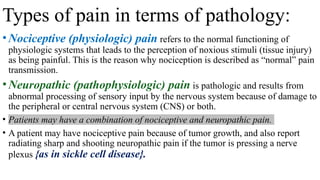
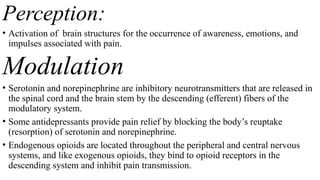
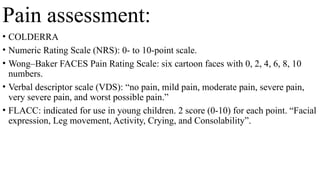
The document outlines pain management objectives for nursing students, covering the identification of pain disorders, integration of pathophysiology and pharmacology, and application of evidence-based nursing for client care. It discusses types of pain (acute, chronic, nociceptive, and neuropathic), assessment methods, and pharmacological management strategies, including nonopioid and opioid analgesics. Additionally, it addresses the implementation of a holistic approach in nursing care and emphasizes the importance of goal setting and evaluation in pain management.