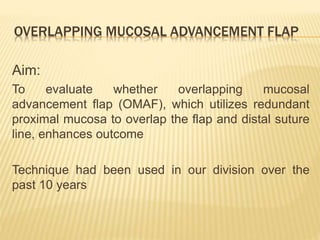
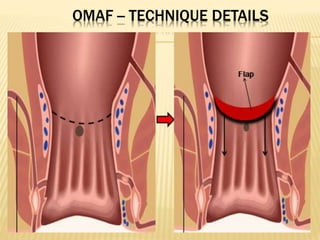
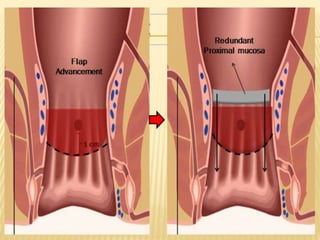
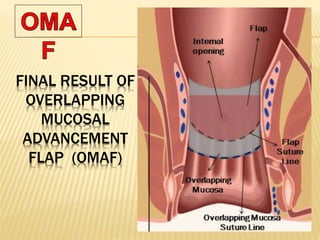
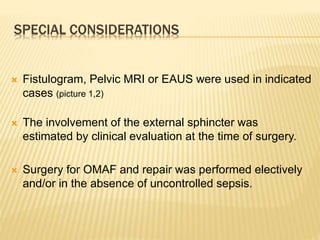
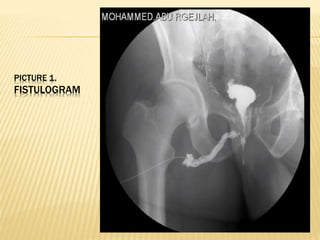
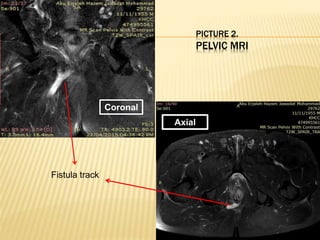
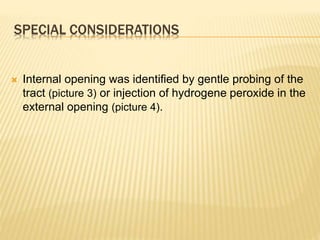
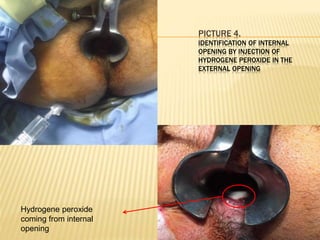
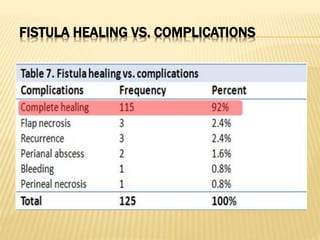
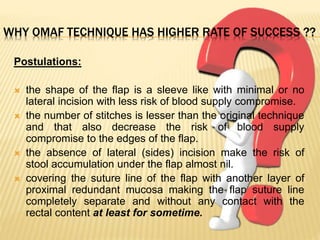
The document discusses the effectiveness of an overlapping mucosal advancement flap (OMAF) technique for repairing high trans-sphincteric fistulas, which presents significant surgical challenges with notable recurrence rates. A retrospective review over six years suggests that the OMAF technique, which utilizes redundant proximal mucosa to overlap the flap and suture line, may improve healing outcomes compared to traditional mucosal advancement flap methods. The findings indicate potential advantages in surgical risk and postoperative recovery associated with the OMAF approach.