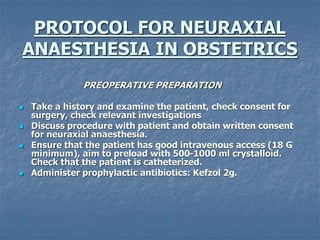
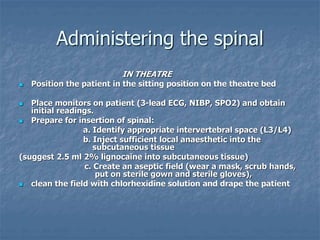
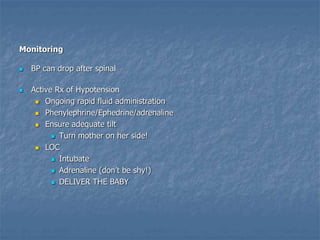
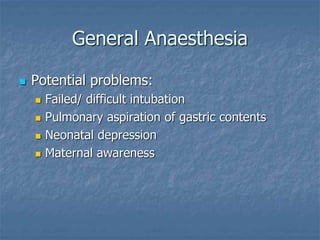
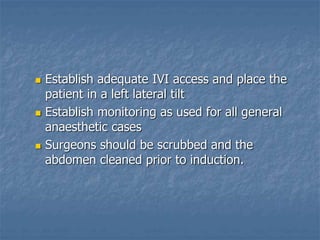
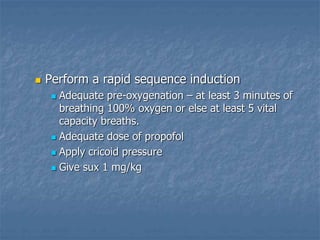
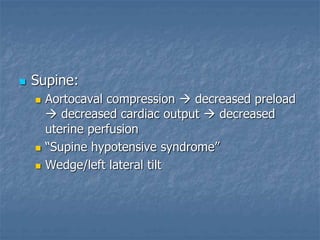
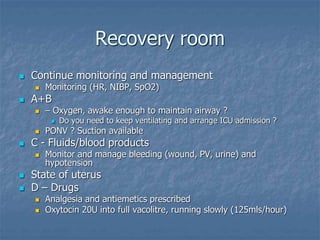
Obstetric anaesthesia involves risks from both general anaesthesia and spinal anaesthesia due to physiological changes in pregnancy and the need to consider both mother and baby. The document outlines protocols for administering spinal anaesthesia including patient assessment, monitoring for complications like hypotension, and management of issues in recovery. It emphasizes vigilant monitoring and proactive treatment of any complications throughout the procedure and recovery.
![4. Insertion of the Spinal Needle:
a. Use a 25 or 27 G pencil point spinal needle.
b. Inject your spinal mixture (prepared in a 5 ml syringe) into
the subarachnoid space.
[1.8 ml 0.5 % heavy bupivacaine and 0.4 ml (20 ug) fentanyl]
C. Apply dressing
5. Position patient in the supine position, ensuring a degree of left
lateral tilt tilt to prevent aortocaval compression. Use of a vaculitre
as a wedge is acceptable.](https://image.slidesharecdn.com/obstetricanaesthesiaupdated2-230807194721-45fc1022/85/Obstetric-Anaesthesia-Updated-2-pptx-10-320.jpg)

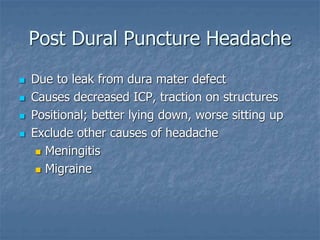
![ Initial treatment is conservative
Strict bed rest
Simple analgesics
[Caffeine]
Epidural blood patch if not resolving within
24hours
Sterile in theatre
Patients’ own blood into EPIDURAL SPACE](https://image.slidesharecdn.com/obstetricanaesthesiaupdated2-230807194721-45fc1022/85/Obstetric-Anaesthesia-Updated-2-pptx-21-320.jpg)