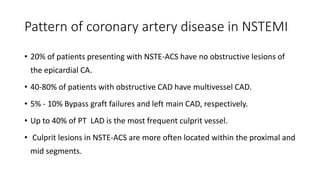
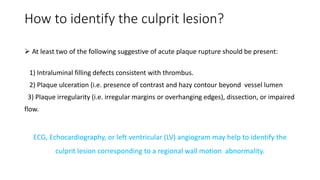
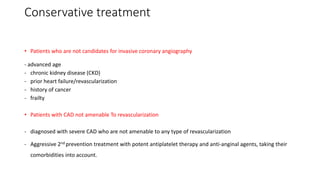
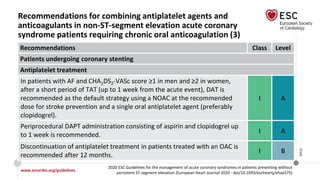
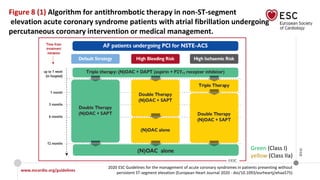
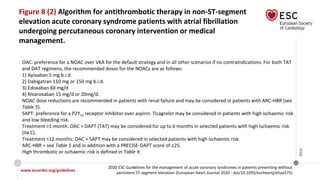
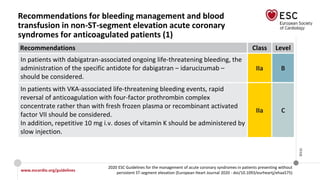
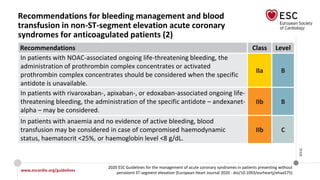
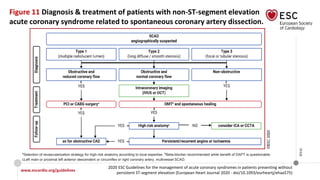
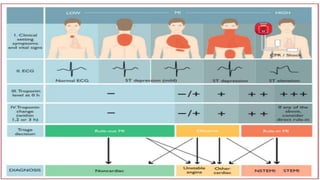
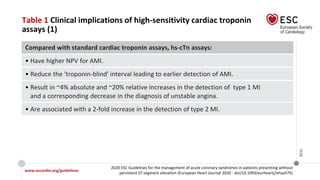
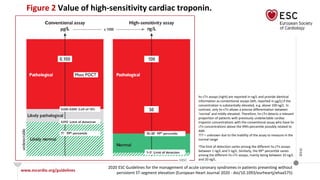
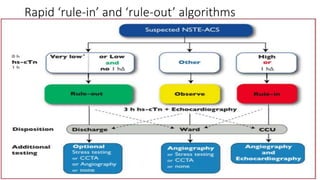
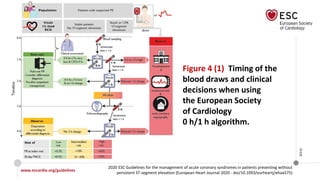
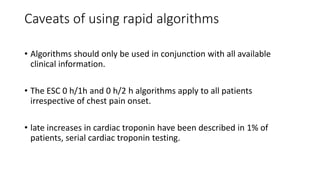
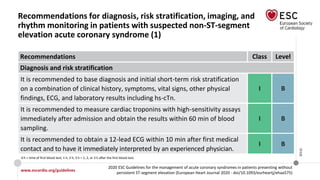
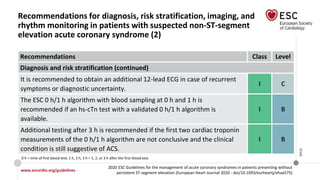
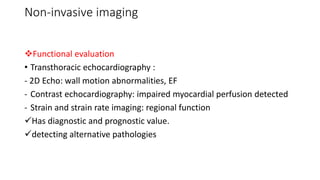
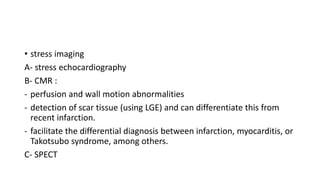
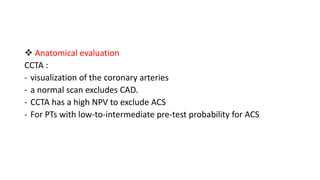
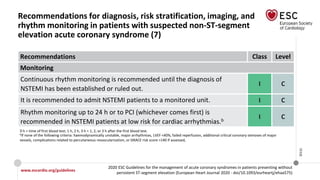
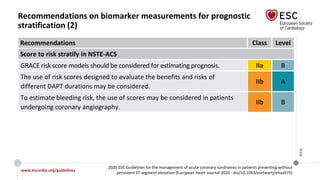
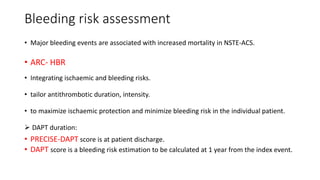
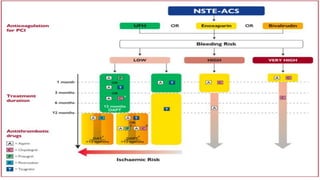
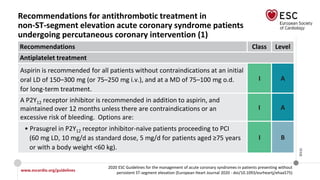
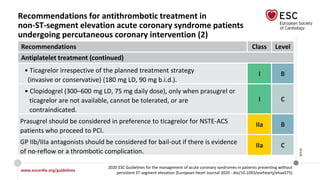
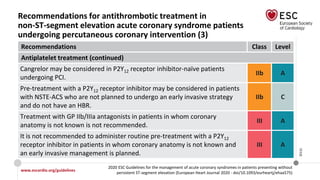
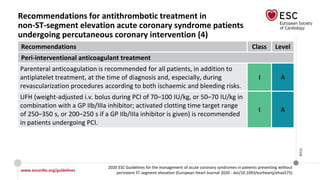
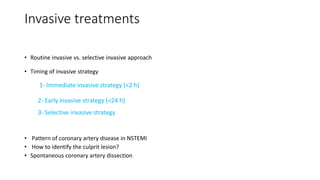
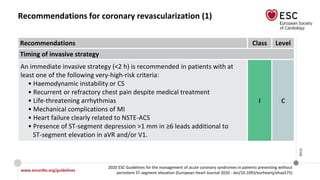
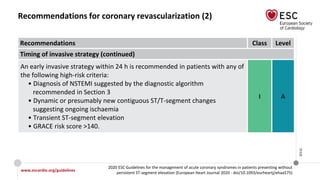
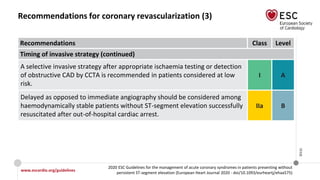
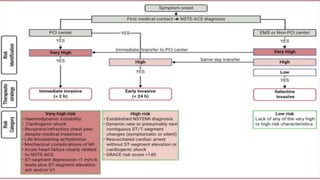
The document provides guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. It discusses the definition, types, epidemiology, diagnosis, risk assessment, and treatment of these conditions. For diagnosis, it recommends an assessment based on history, symptoms, vital signs, ECG, and cardiac troponin tests. It provides algorithms for rapid rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin tests. It also discusses the role of imaging modalities like echocardiography and CCTA in diagnosis and risk stratification. Treatment options include pharmacological, invasive, and conservative therapies based on risk assessment.
![Biomarkers
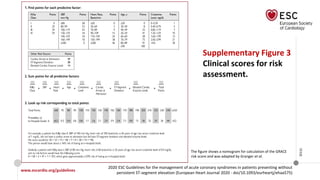
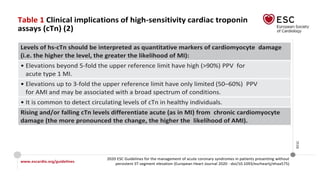
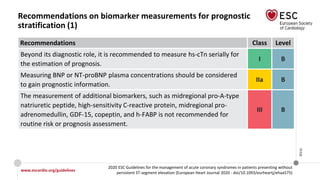
• Toponin: The higher the hs-cTn levels, the greater the risk of death.
• Serum creatinine and eGFR.
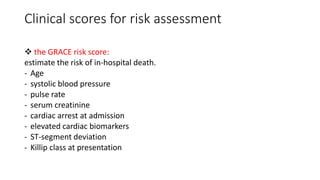
key elements of (GRACE) risk score
• natriuretic peptides [BNP and N-terminal pro-BNP (NT-proBNP)]](https://image.slidesharecdn.com/nstemi-220719014224-c31f8f79/85/NSTEMI-pptx-33-320.jpg)

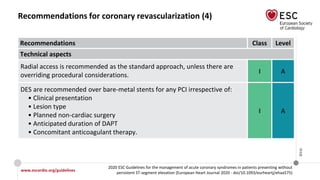
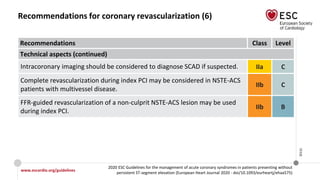
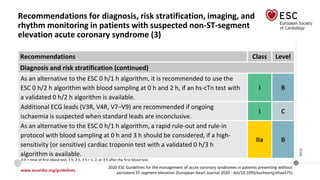
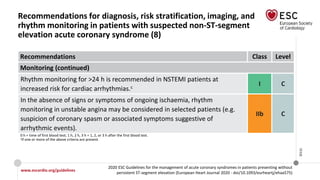
![www.escardio.org/guidelines
2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without
persistent ST-segment elevation (European Heart Journal 2020 - doi/10.1093/eurheartj/ehaa575)
©ESC
Recommendations for coronary revascularization (5)
Recommendations Class Level
Technical aspects (continued)
It is recommended to base the revascularization strategy (ad hoc culprit
lesion PCI/multivessel PCI/CABG) on the patient’s clinical status and
comorbidities, as well as their disease severity [i.e. the distribution and
angiographic lesion characteristics (e.g. SYNTAX score)], according to the
principles for stable CAD. However, the decision on immediate PCI of the
culprit stenosis does not require Heart Team consultation.
I B
Complete revascularization should be considered in NSTE-ACS patients
without CS and with multivessel CAD.
IIa C](https://image.slidesharecdn.com/nstemi-220719014224-c31f8f79/85/NSTEMI-pptx-64-320.jpg)