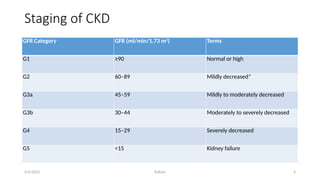
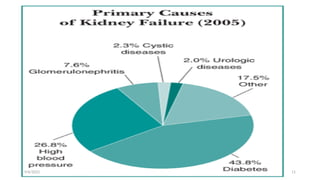
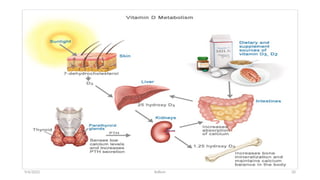
The document provides a comprehensive overview of chronic kidney disease (CKD), including its definition, staging, causes, clinical manifestations, diagnosis, and treatment approaches. CKD is characterized by a progressive loss of kidney function, often presenting with symptoms such as fluid retention, uremia, and anemia. Effective management focuses on reversing the underlying causes, relieving symptoms, and may involve dialysis or transplantation in advanced cases.