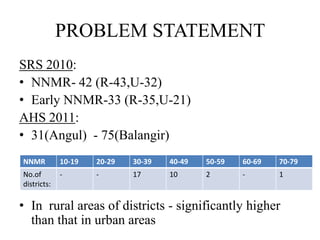
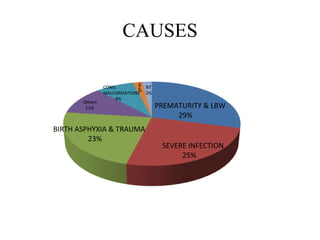
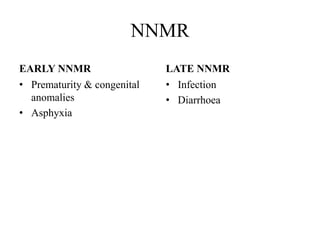
Neonatal deaths in Odisha remain a significant public health problem, accounting for over half of infant and under-5 mortality. The neonatal mortality rate in Odisha is 42 per 1000 live births, with 33 occurring in the early neonatal period. Prematurity, low birth weight, birth asphyxia, and infections are the leading causes. Coverage of antenatal care, institutional deliveries, and postnatal practices like early and exclusive breastfeeding remain areas for improvement. Expanding programs like the Janani Surakshya Yojana and improving access to skilled birth attendance and emergency obstetric and newborn care can help reduce neonatal mortality in Odisha.

![IMR & NNMR
70
60
50
40
9 (14.8% 0f IMR)
30 61
20
33 (54% of IMR: R-55%,
10 U-50%)
0
IMR NNMR
[SRS 2010]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-5-320.jpg)
![U5MR & NNMR
90
80
70
60
50
78
40
30
42 ( 54% of U5MR )
20
10
0
U5MR NNMR
[SRS 2010]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-6-320.jpg)
![ANC
120%
98
100%
80% 77
58.4
60%
40% 37.5
20%
0%
at least 1 2+ 3+ full
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-10-320.jpg)
![CONSUMPTION OF IFA DURING
PREGNANCY
%
None
10%
30 days 100 days
16%
47%
31-90 days
27%
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-11-320.jpg)
![PLACE OF DELIVERY
%
At home
24.5%
Institutional
75.5%
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-12-320.jpg)
![Duration of stay at health facility
4+ days
8%
3 days
8%
2 days
1 day
12%
44%
1 day
28%
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-13-320.jpg)
![DELIVERY ATTENDED BY SBA
90
79%
80
70
60
50
40
30 21%
20
10
0
SBA none
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-14-320.jpg)
![INSTITUTIONAL DELIVERIES & JSY
JSY 60.7 %
Institutional deliveries
75.5 %
0.00% 20.00% 40.00% 60.00% 80.00%
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-15-320.jpg)
![BF AFTER CHILD BIRTH
70.00%
63.7
60.00%
50.00%
40.00%
30.00% 27.2
20.00%
8.8
10.00%
0.3
0.00%
< 1 hr 1-23 hr ³ 24 hr No BF
[COVERAGE EVALUATION SURVEY 2009]](https://image.slidesharecdn.com/neonataldeathsinodisha-120613095804-phpapp02/85/Neonatal-deaths-in-odisha-16-320.jpg)