This document provides guidance on performing a musculoskeletal examination. Key points include:
1) Examine general appearance, observe for asymmetry, compare limbs, and assess active range of motion before passive.
2) Screen for pain or stiffness, ability to dress oneself, and ability to climb stairs.
3) Inspect gait for limps or other abnormalities and describe gait cycle.
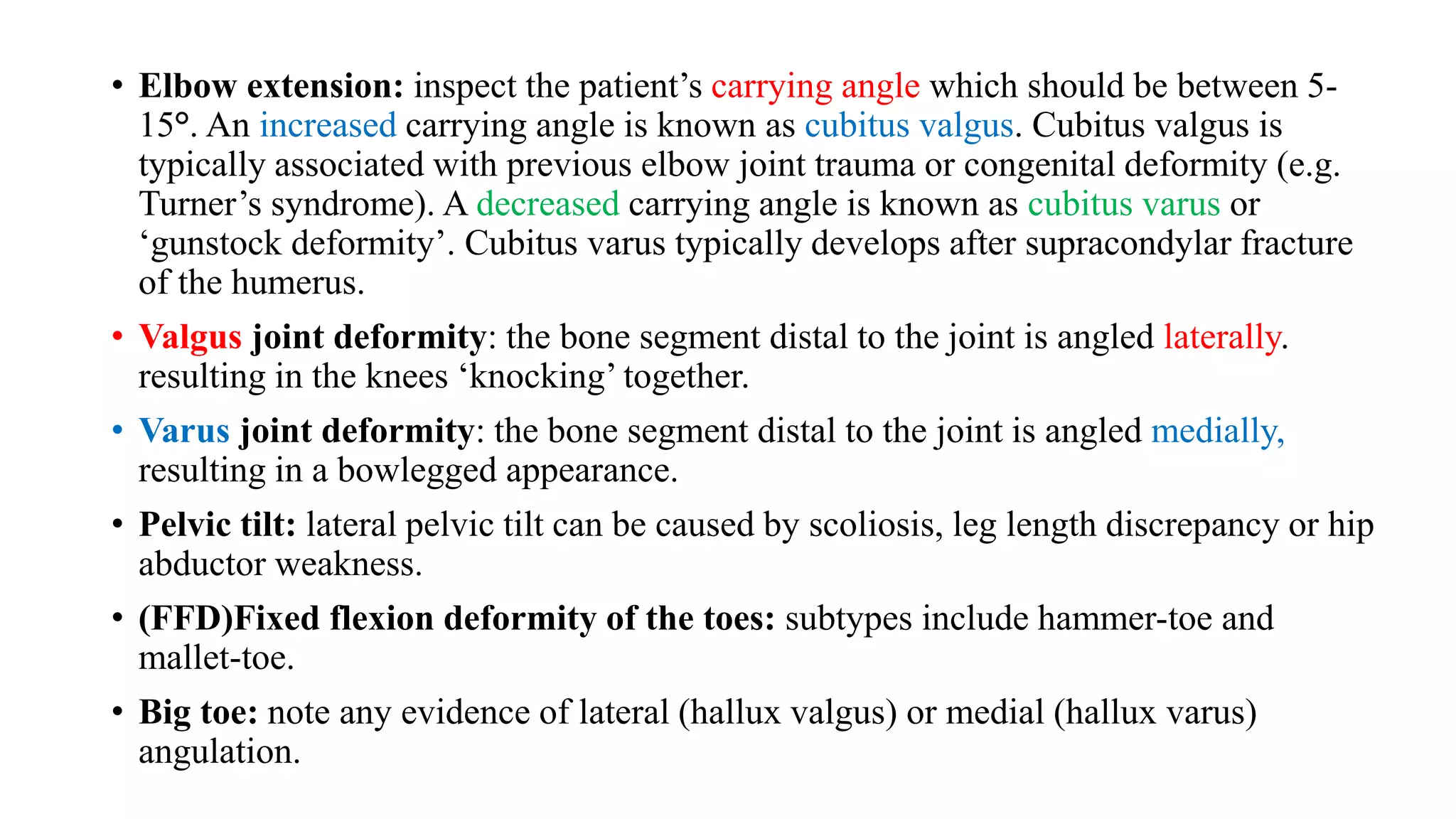
4) Examine joints for swelling, erythema, deformities, and range of motion both anteriorly and posteriorly.