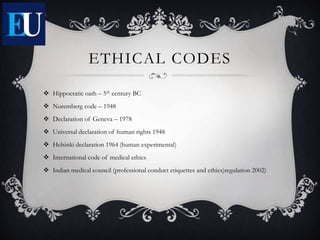
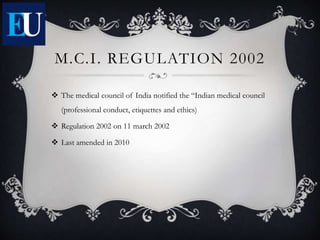
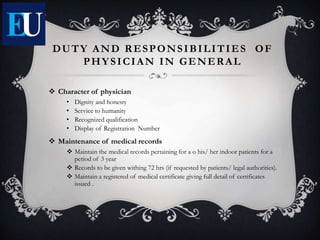
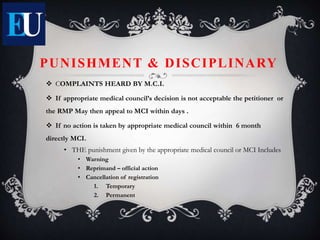
This document provides an introduction to medical ethics. It discusses that medical ethics deals with moral issues that arise in medical practice and research. The main principles of medical ethics discussed are autonomy, beneficence, confidentiality, non-maleficence, and justice. Regulations like the Hippocratic Oath, Declaration of Geneva, and the Indian Medical Council's code of conduct are mentioned. The importance of medical ethics for the patient-physician relationship and conduct of research is highlighted.