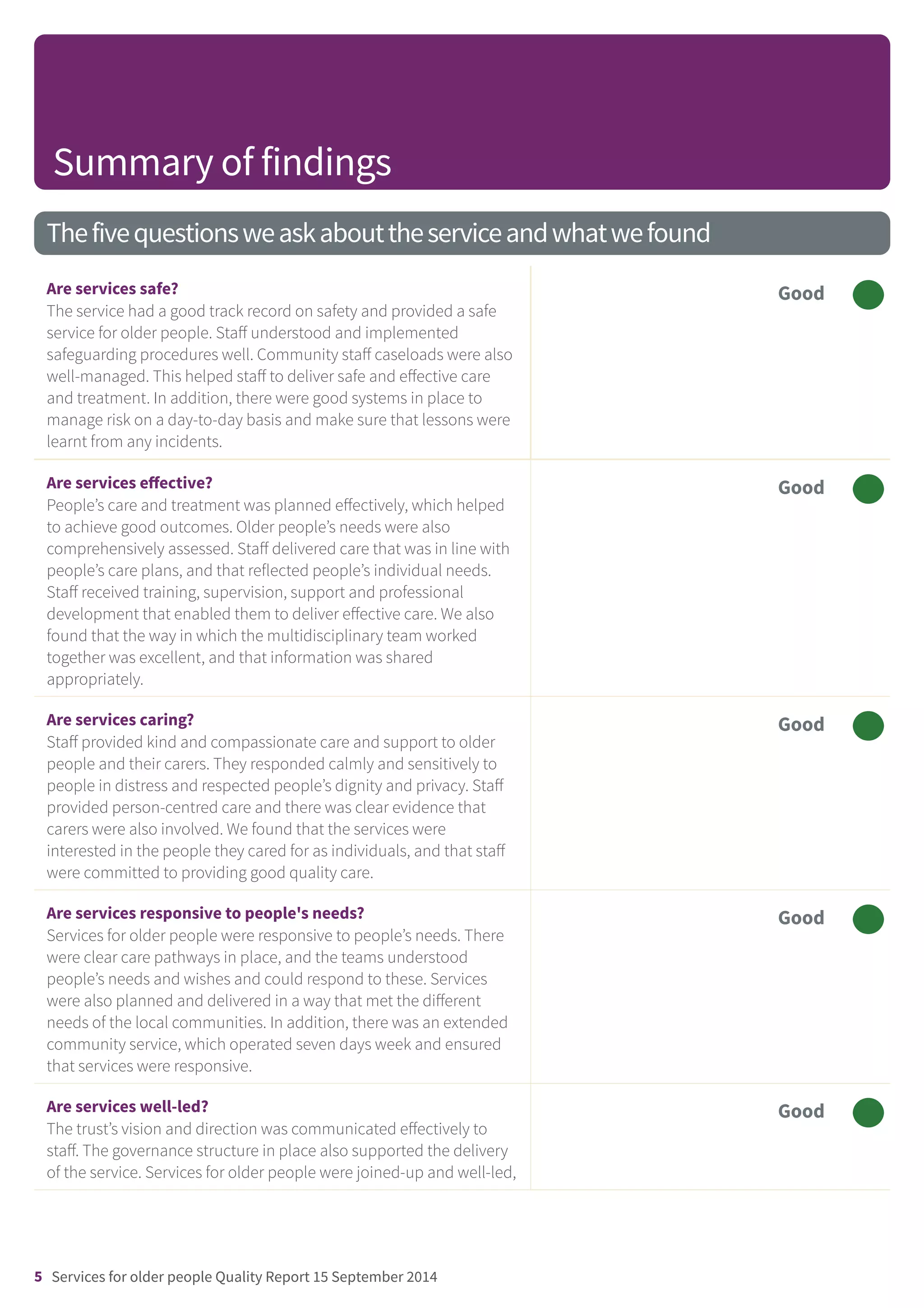
This document provides a summary of the Care Quality Commission's (CQC) inspection of services for older people provided by Bradford District Care Trust. It finds that services were safe, effective, caring, responsive and well-led. Key points include:
- Staff understood safeguarding procedures and managed risks and caseloads well
- Care was planned effectively and delivered according to individual needs
- The multidisciplinary team worked well together
- Staff provided compassionate and person-centred care
- Services were responsive to the community's needs through their provision
- Managers were accessible and the trust involved service users in development