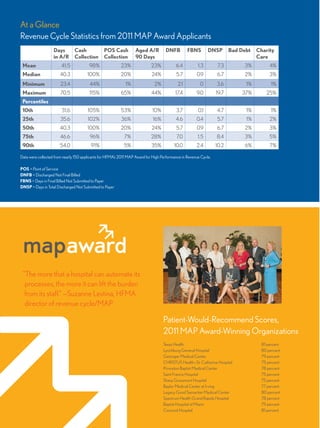
The document discusses strategies for improving revenue cycle performance that were employed by hospitals that won HFMA's MAP Award for High Performance in Revenue Cycle. It outlines seven key strategies used by the award-winning hospitals: 1) Create dedicated teams for revenue cycle improvement 2) Use metrics to conduct root cause analysis 3) Create shared accountability for performance 4) Collaborate across departments 5) Develop comprehensive uncompensated care approaches 6) Enhance customer service 7) Focus on improving the total patient experience. The strategies helped increase cash collections, reduce days in accounts receivable, lower bad debt, and improve patient satisfaction scores.

![Legacy Good Samaritan
Medical Center in Portland,
Ore., developed a revenue
cycle project team four years
ago that provides support
and project management
for revenue cycle initiatives.
“The project team allows our
managers to concentrate on
their day-to-day work while
enabling our system to be innovative in our approach to revenue
cycle improvement,” says Mary Kjemperud, vice president, revenue
cycle, Legacy Health. Team members include a project coordinator
and a project analyst.
Within the revenue cycle at St. Catherine Hospital in Houston—
part of CHRISTUS Health—high-performance work teams have
redesigned revenue cycle workflows to increase efficiency. When
CHRISTUS Health’s revenue cycle departments converted to a
new IT platform—a move that affected several facilities—these high-
performance work teams facilitated the switch to the new system
and ensured rapid stabilization. “When we converted our systems,
although we experienced a slight blip in A/R [accounts receivable]
days, we recovered in less than 60 days. That’s an outstanding
achievement, especially considering there were some chargemaster
issues that held up billing for the first 30 days after the platform went
live,” says Cassandra Hogans, systems director, patient financial
services, CHRISTUS Health.
The use of metrics to conduct
root cause analysis was a key
to success for all MAP Award
winners. For example, in addition
to reviewing traditional metrics
for revenue cycle performance,
Legacy Health also reviews top
10 claim edits and top 10 charge
work edits, “So we’re actually
looking at the front end as well as the billing—what’s going out the
door,” says Terrie Handy, director of patient business services for the
health system. Through a careful, continuous review of key metrics
and root cause analysis, Legacy Health’s percentage of secured
accounts has increased to 99 percent at time of service, and the
system has achieved a net cash increase of nearly $20 million,
Handy says.
At St. Catherine Hospital, metrics are all web-based. “This pro-
vides us with an apples-to-apples-like comparison, plus it allows our
organization to have easy access to the data,” Hogans says. “We also
provide all of our managers, team leads, and supervisors with our
revenue cycle academy training, which includes root-cause analysis
as well as training in outcome action planning that relates to the root
cause analyses.”
St. Catherine Hospital uses “kaizen events”—five-day intensive
events “that allow us to redefine the process, implement metrics, and
implement team shift briefings as well as work management tools”—
to eliminate errors and enhance work flow within the revenue cycle,
Hogans says. “Our root-cause analysis is a significant part of that
process,” she says. Using root-cause analysis, St. Catherine Hospi-
tal’s net-to-cash conversion has increased from 88 percent to
95 percent, and many other CHRISTUS Health facilities have
achieved the same level of excellence. “Our success comes from
having well-designed, standard processes and tools,” Hogans
says. “That 7 percent difference can be multiplied by hospital net
revenues to determine our true cash benefit.”
At Concord Hospital, Concord, N.H, where the emergency
department (ED) is the busiest in the state, a process improvement
workgroup was initiated to assess the coding and charging process
for ED accounts. The workgroup was composed of ED physicians
Strategy No.2Use metrics to conduct root
cause analysis to facilitate
systemic change.
Strategy No.1Create teams dedicated
to revenue cycle
improvement.
At St. Catherine Hospital, high-per-
formance work teams enable each
cell to function as a mini-business
unit. Among the improvements
St. Catherine has experienced is an
increase in net-to-cash conversion
from 88 percent to 95 percent.
MAP Award-Winning
Strategies for Success
Seven specific strategies for revenue cycle
success came to light during interviews
with recipients of this year’s MAP Award.
hfm_SpecialInsert_081611.indd 3 8/16/11 8:56 AM](https://image.slidesharecdn.com/f1eed477-3454-4d79-923f-ea1768b92cc2-161021163502/85/MAP-3-320.jpg)