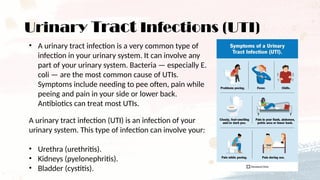
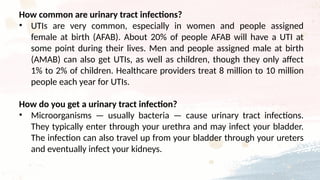
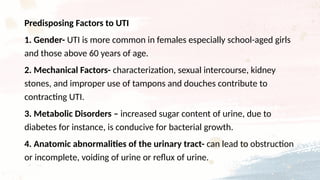
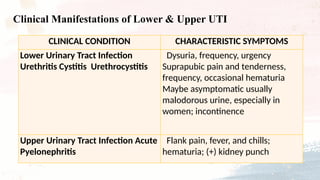
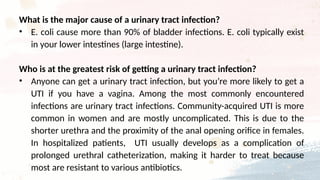
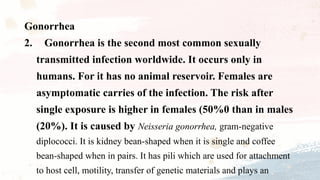
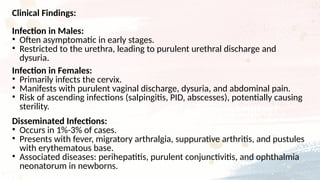
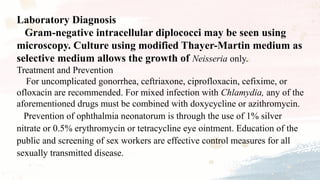
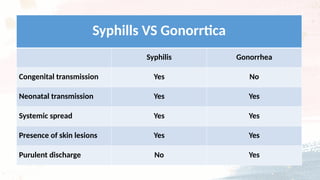
The document provides an overview of urinary tract infections (UTIs) and sexually transmitted infections (STIs), detailing the anatomy of the urinary tract and common causes, symptoms, and treatments of UTIs, primarily caused by E. coli. It also covers various STIs such as chlamydia, gonorrhea, syphilis, and herpes, highlighting their modes of transmission, clinical manifestations, and laboratory diagnosis, emphasizing the importance of prevention and prompt treatment. Overall, it underscores the significance of proper diagnostics and management to ensure effective healthcare outcomes.