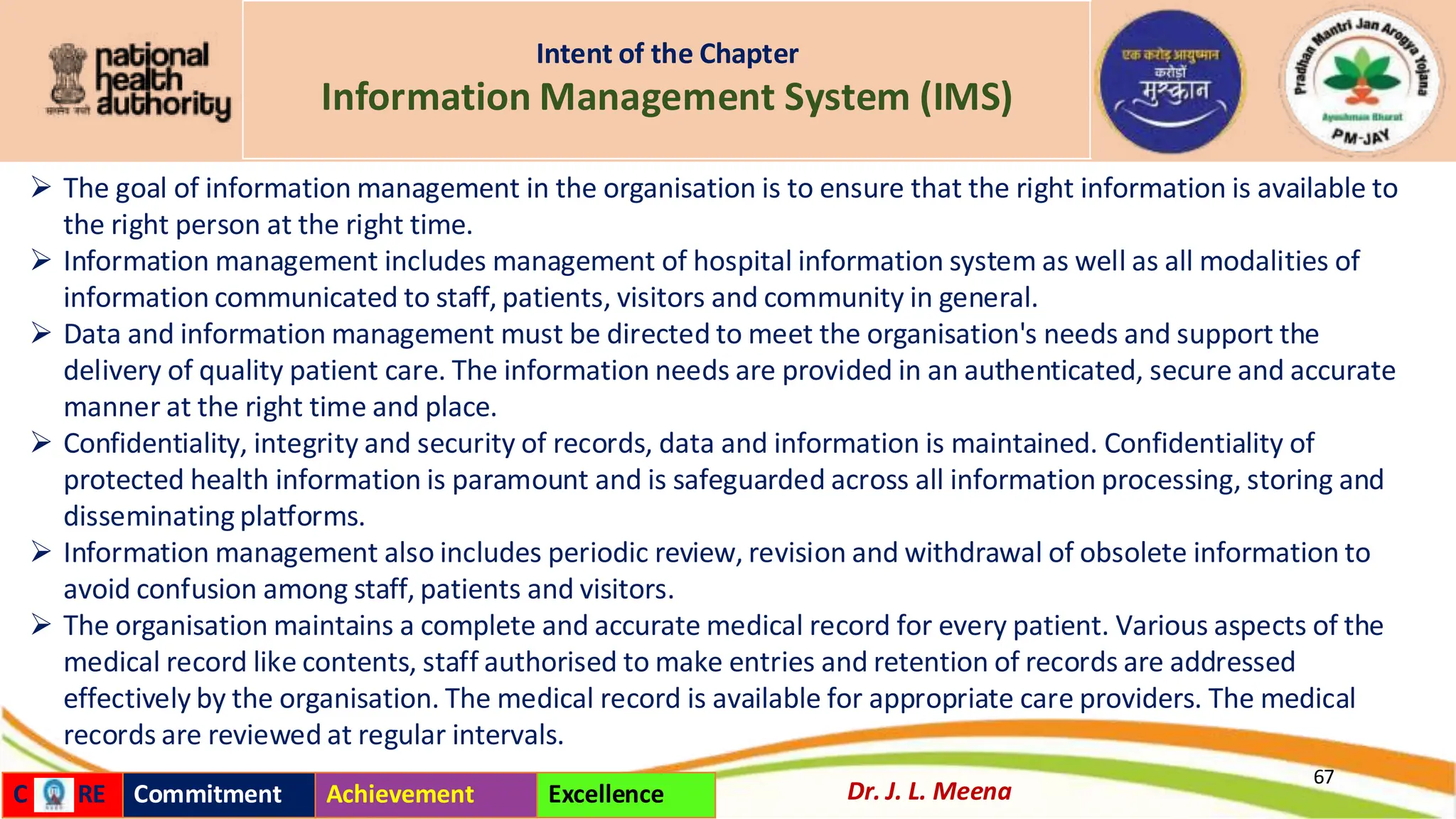
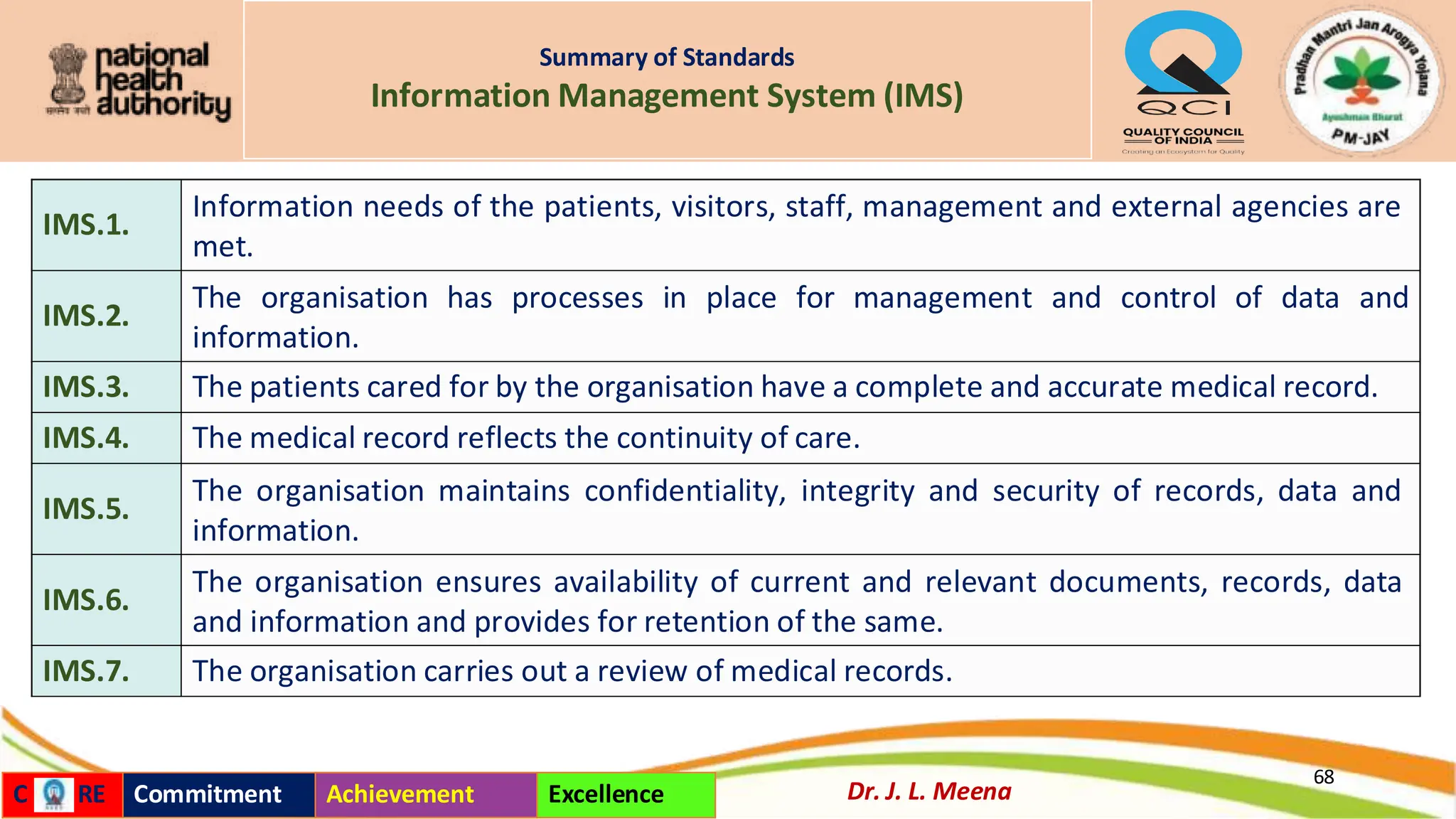
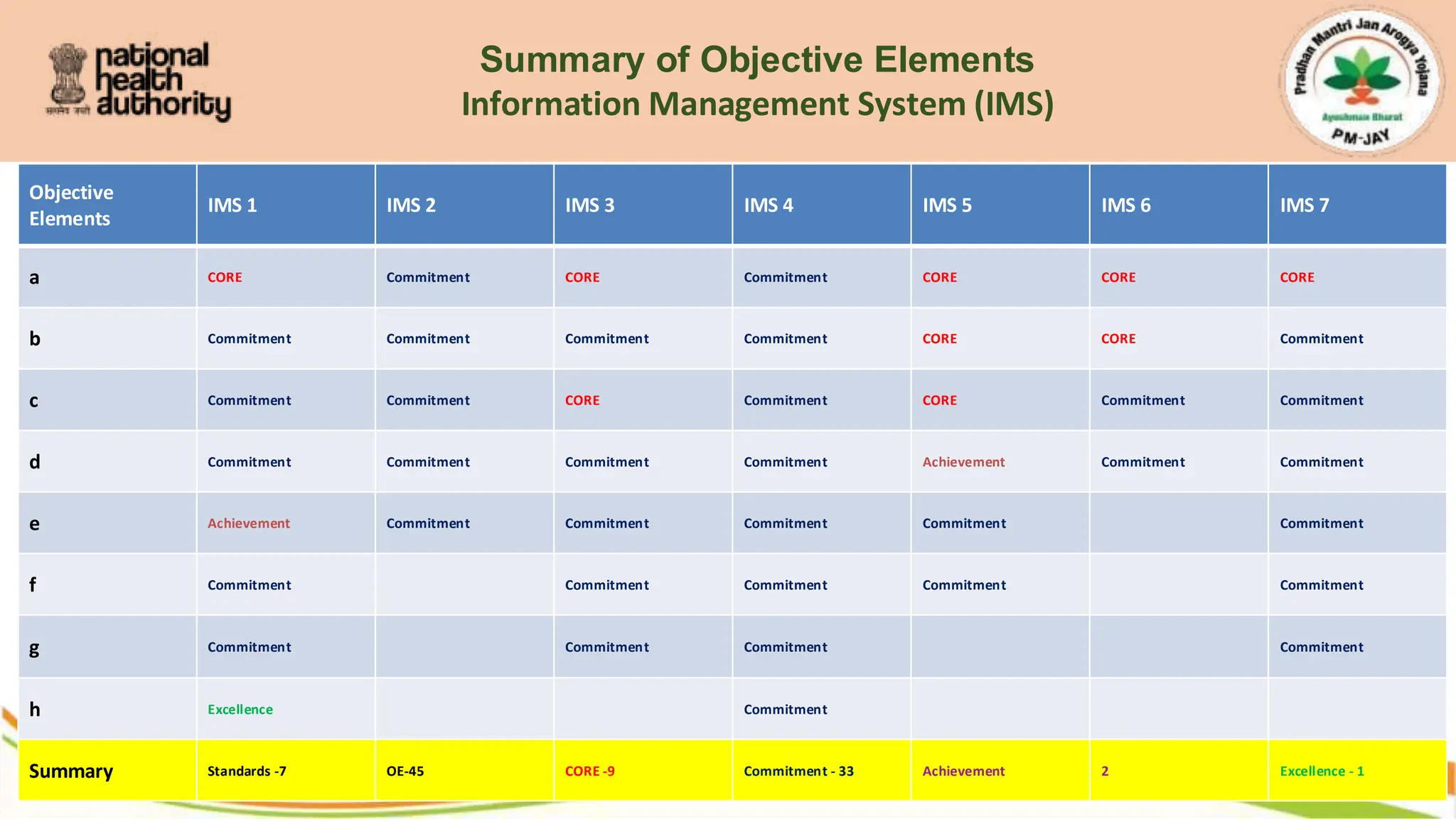
An Information Management System (IMS) promotes patient safety by reducing medical errors, streamlining communication among healthcare providers, and enabling data-driven decisions. Key features include automated alerts for potential risks, compliance tracking, and secure data sharing. By fostering transparency and accountability, IMS improves care quality, minimizes adverse events, and supports regulatory compliance, ultimately safeguarding patient well-being in healthcare settings. IMS for patient safety is a digital framework designed to enhance healthcare delivery by organizing, storing, and analyzing patient data. It integrates electronic health records, incident reporting, and risk management tools to ensure accurate, real-time information access.