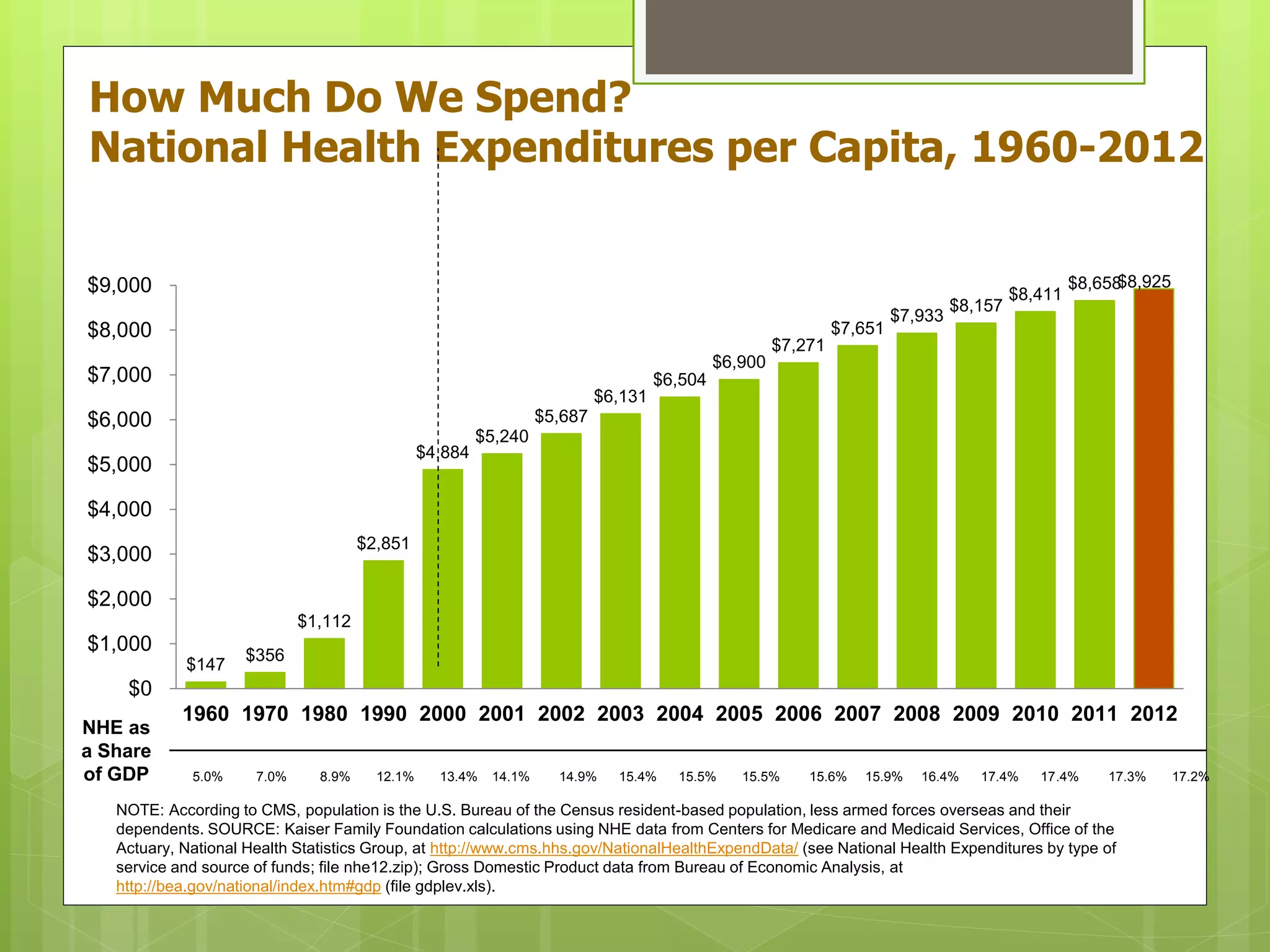
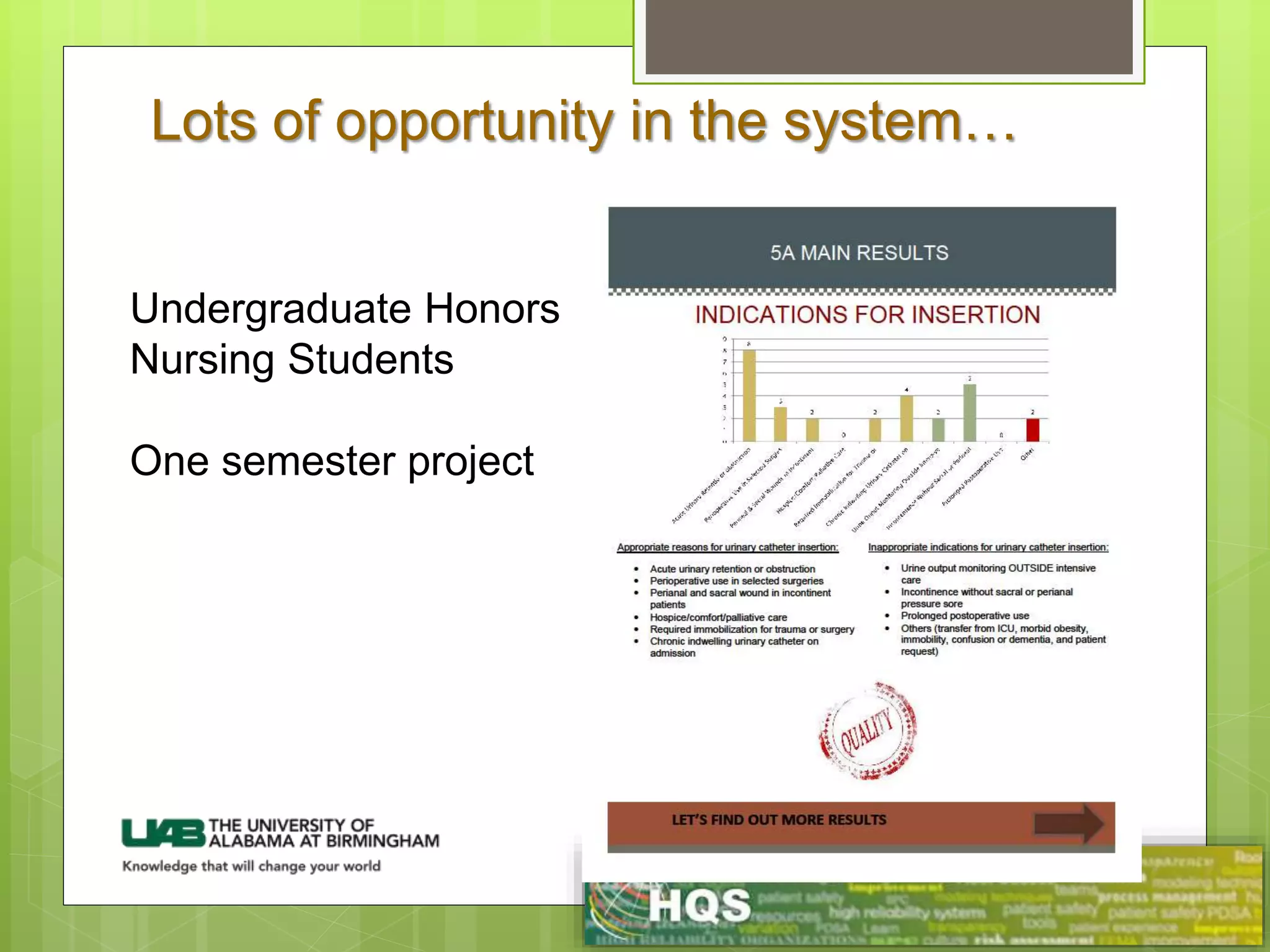
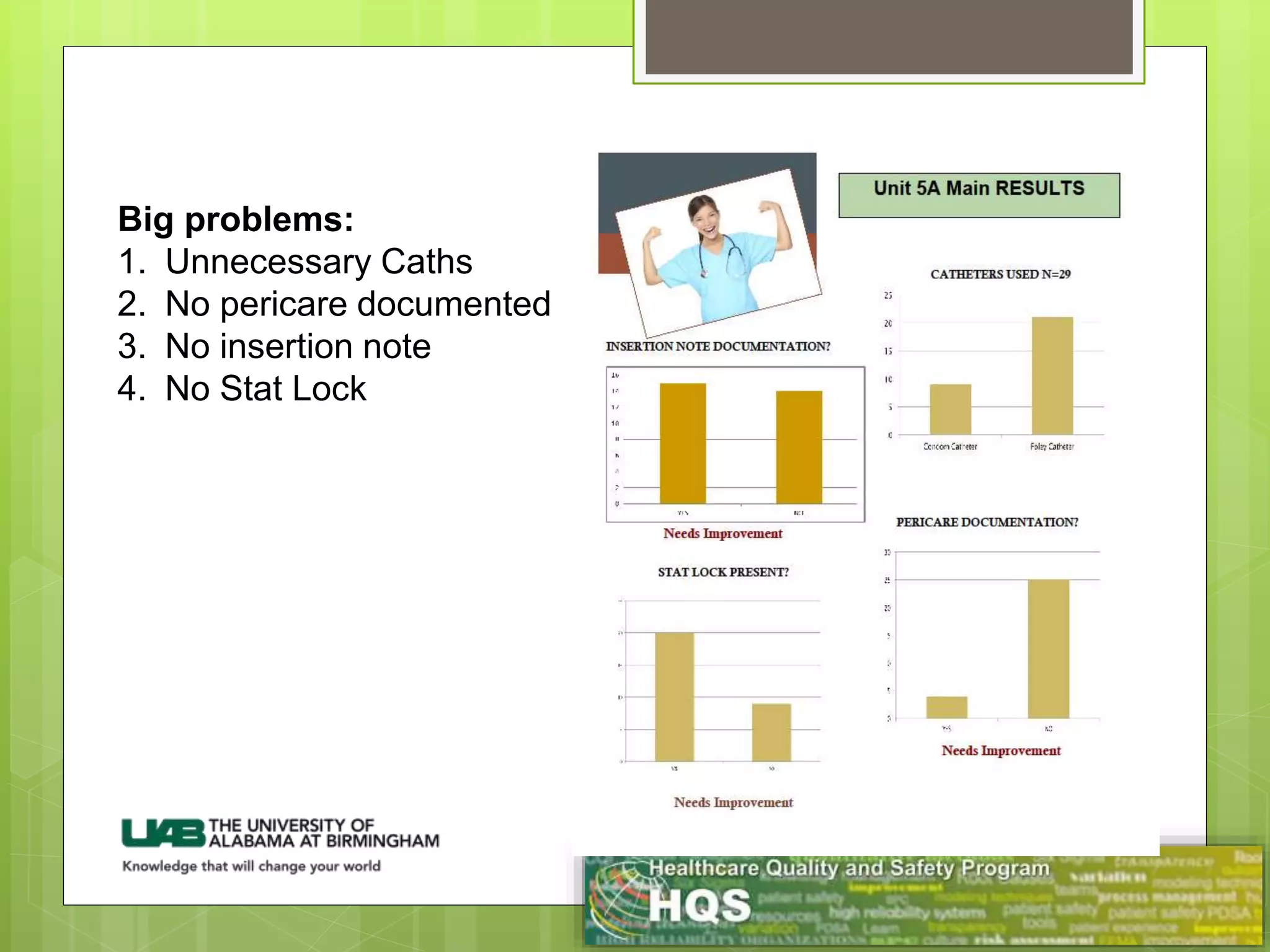
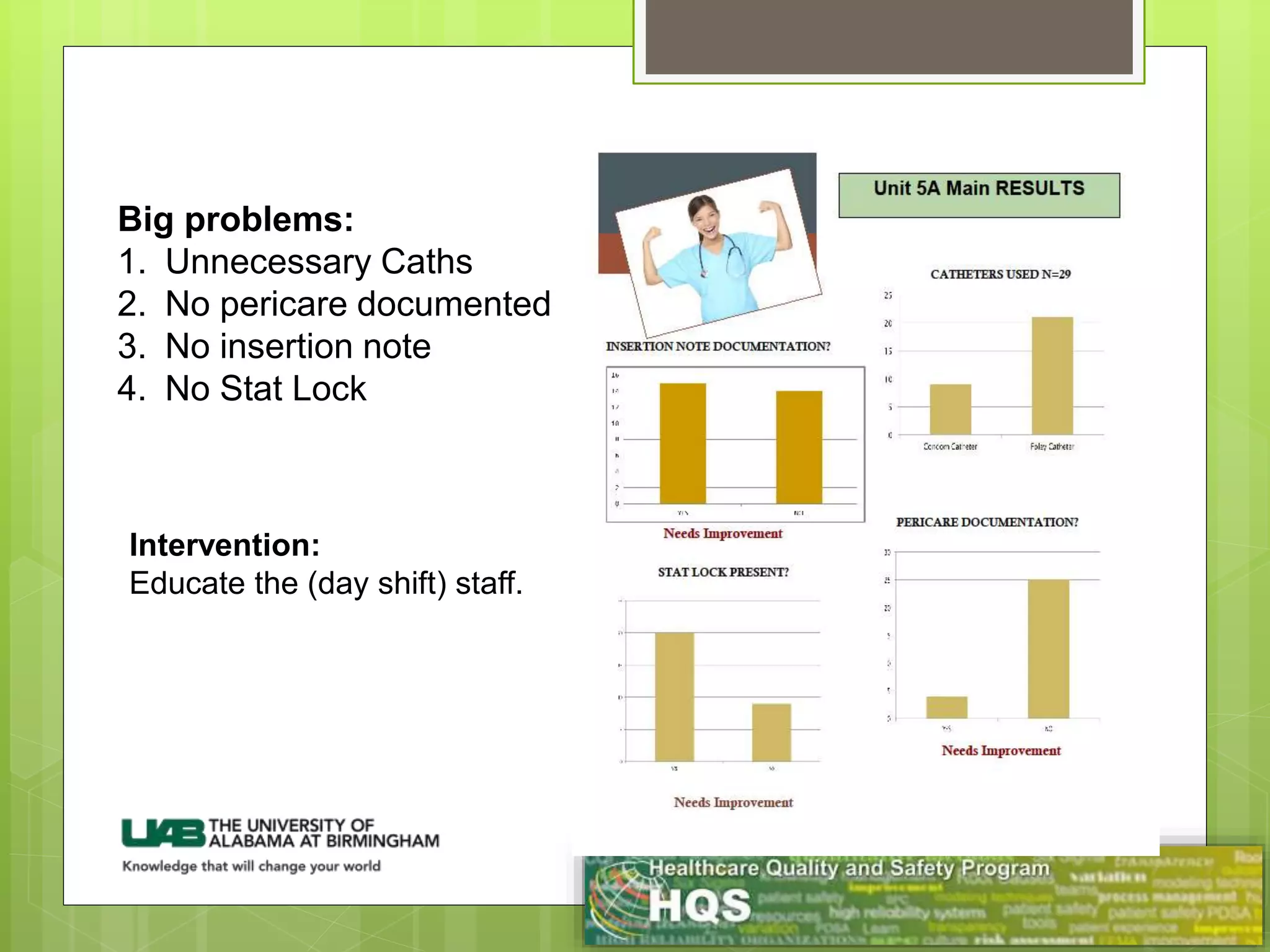
The document discusses identifying problems in healthcare quality and reducing waste. It begins by outlining the six aims of quality healthcare: safe, timely, effective, efficient, equitable, and patient-centered. It then discusses various sources of waste in the healthcare system, including overtreatment, failures of care coordination, failures to execute best practices, excessive administrative complexity, pricing failures, and fraud/abuse. Specific estimates are given for the amount of waste from each category, totaling hundreds of billions of dollars annually. The document emphasizes the opportunity for improvement that exists and stresses the importance of focusing on problems we can directly address and fix.