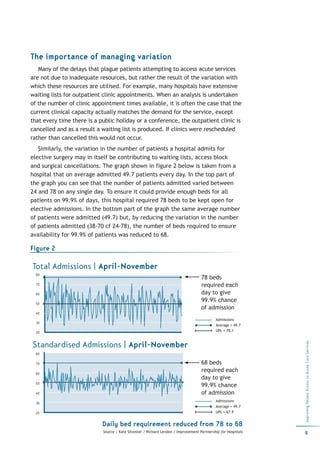
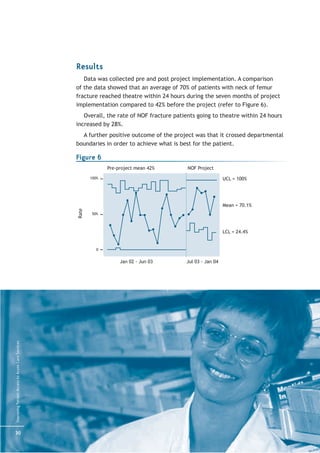
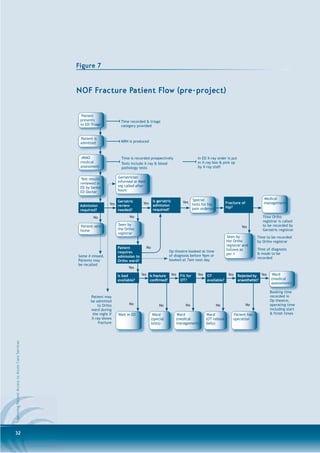
This document provides a toolkit for public hospitals to improve patient access to acute care services. It outlines a process for hospitals to plan improvements, which includes identifying problems, reviewing performance data, engaging clinicians, understanding current systems, determining goals, implementing changes, analyzing results, and communicating changes. The toolkit compiles strategies from various sources that have been shown to improve patient flow, though the evidence level varies. It is intended to help hospitals redesign processes to provide safe, efficient, and timely patient-centered care.