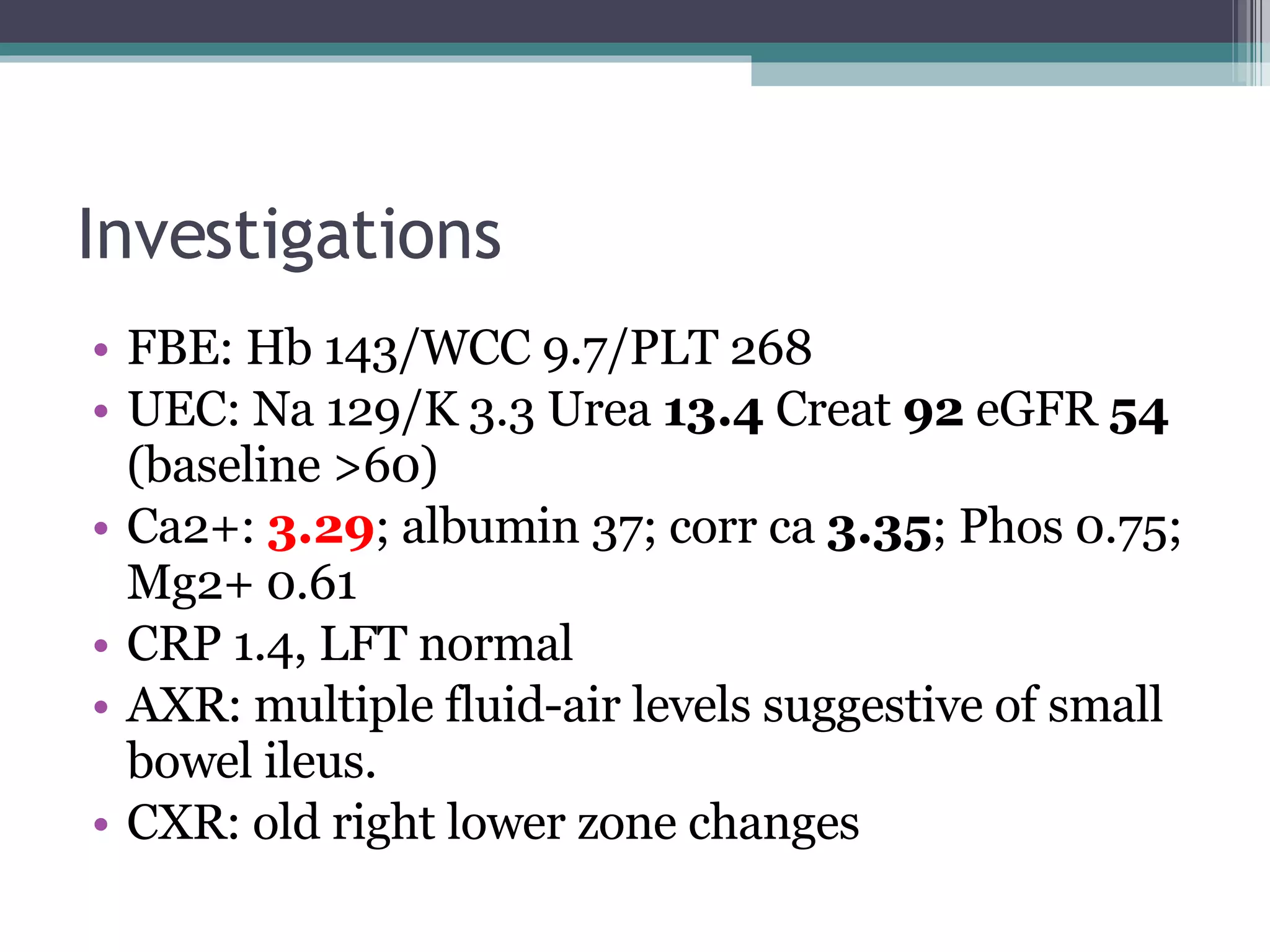
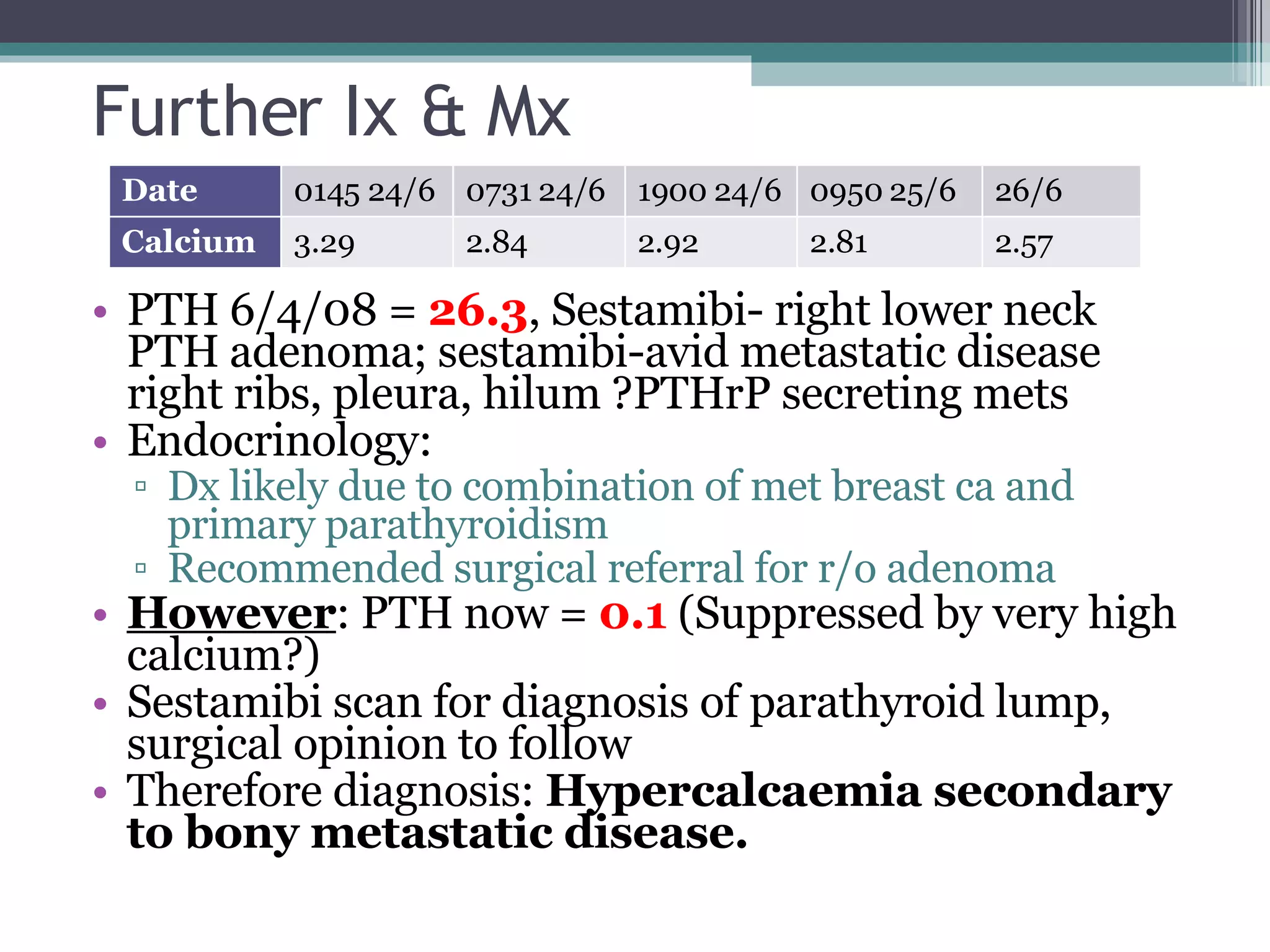
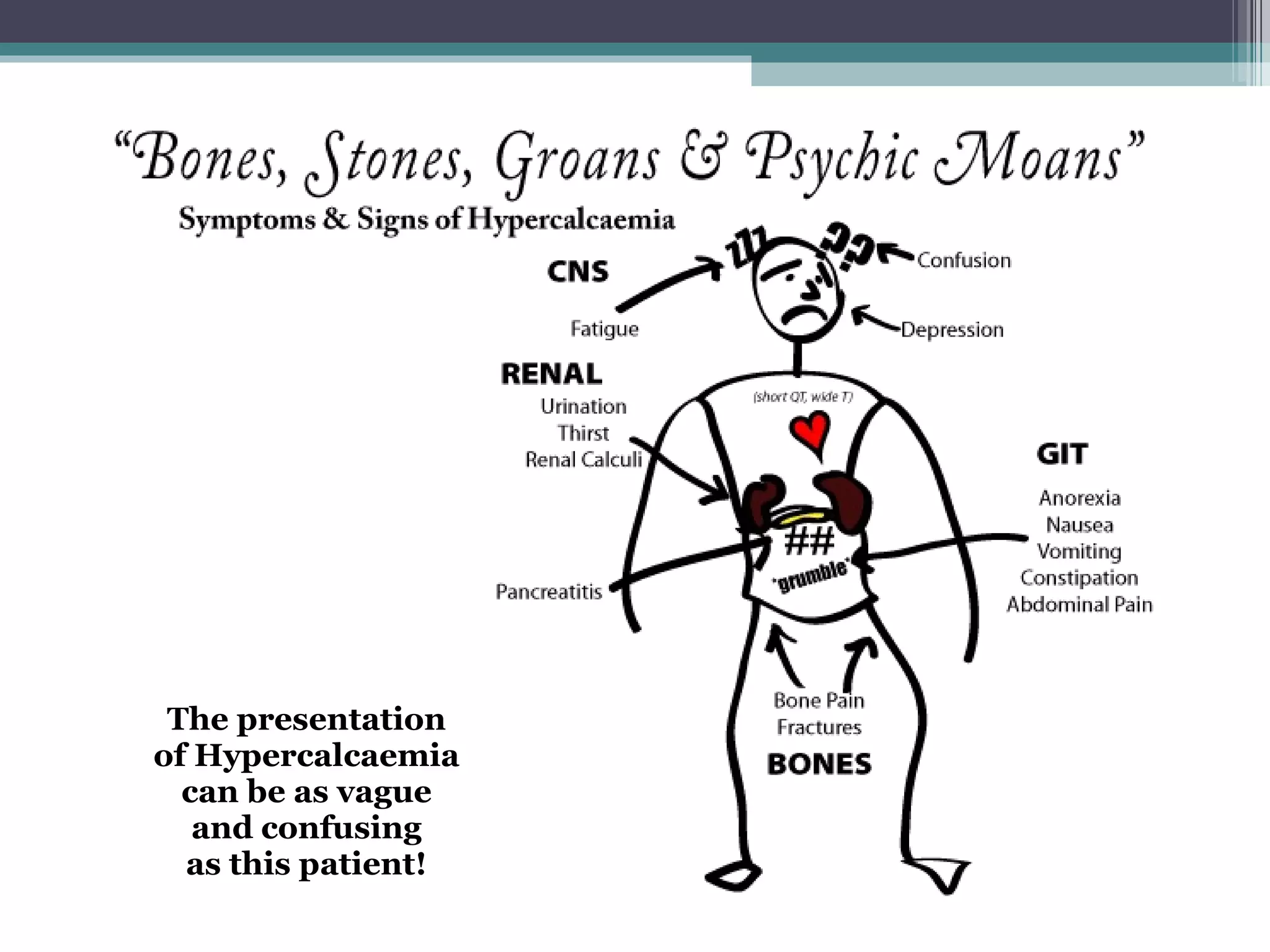
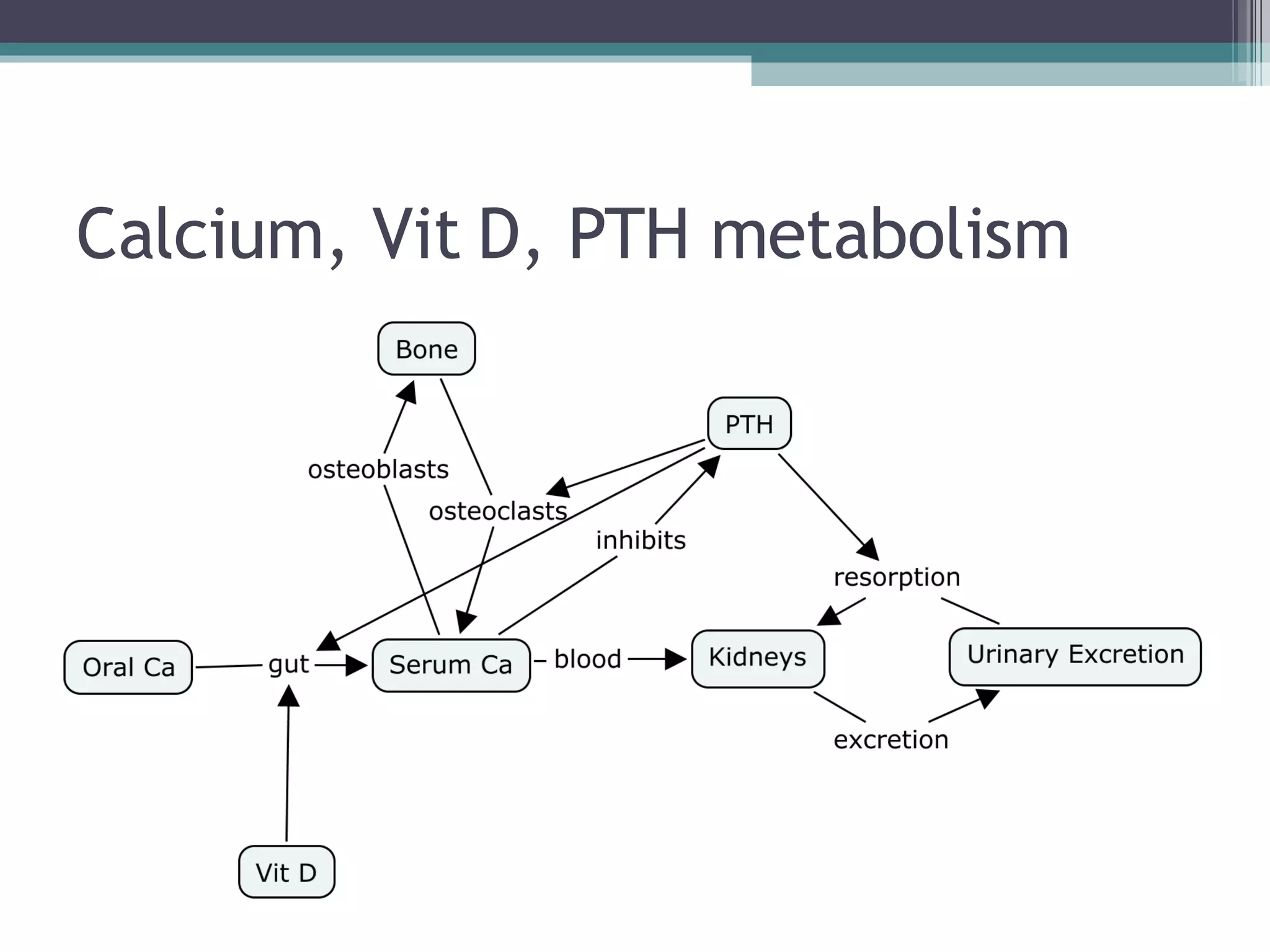
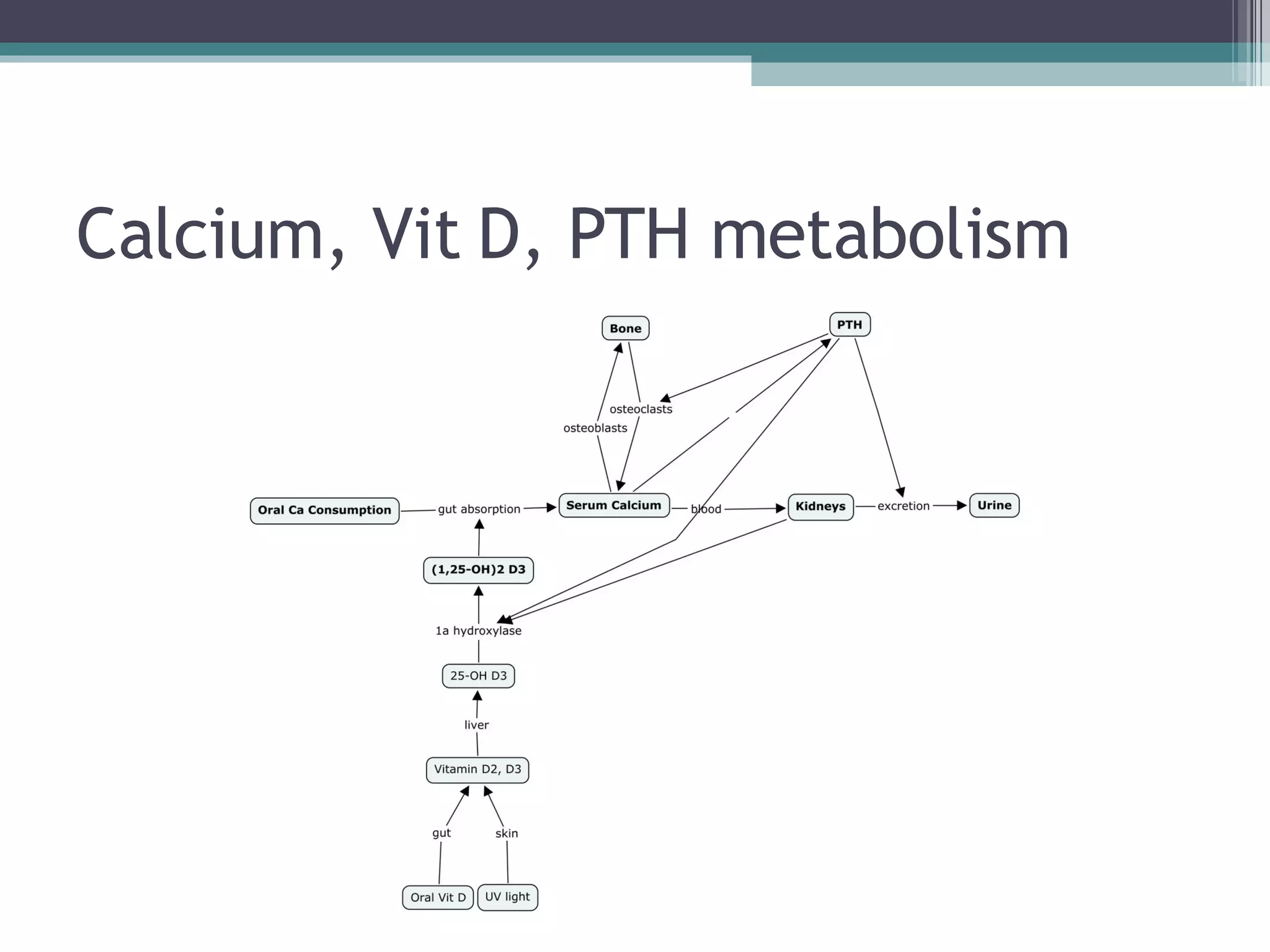
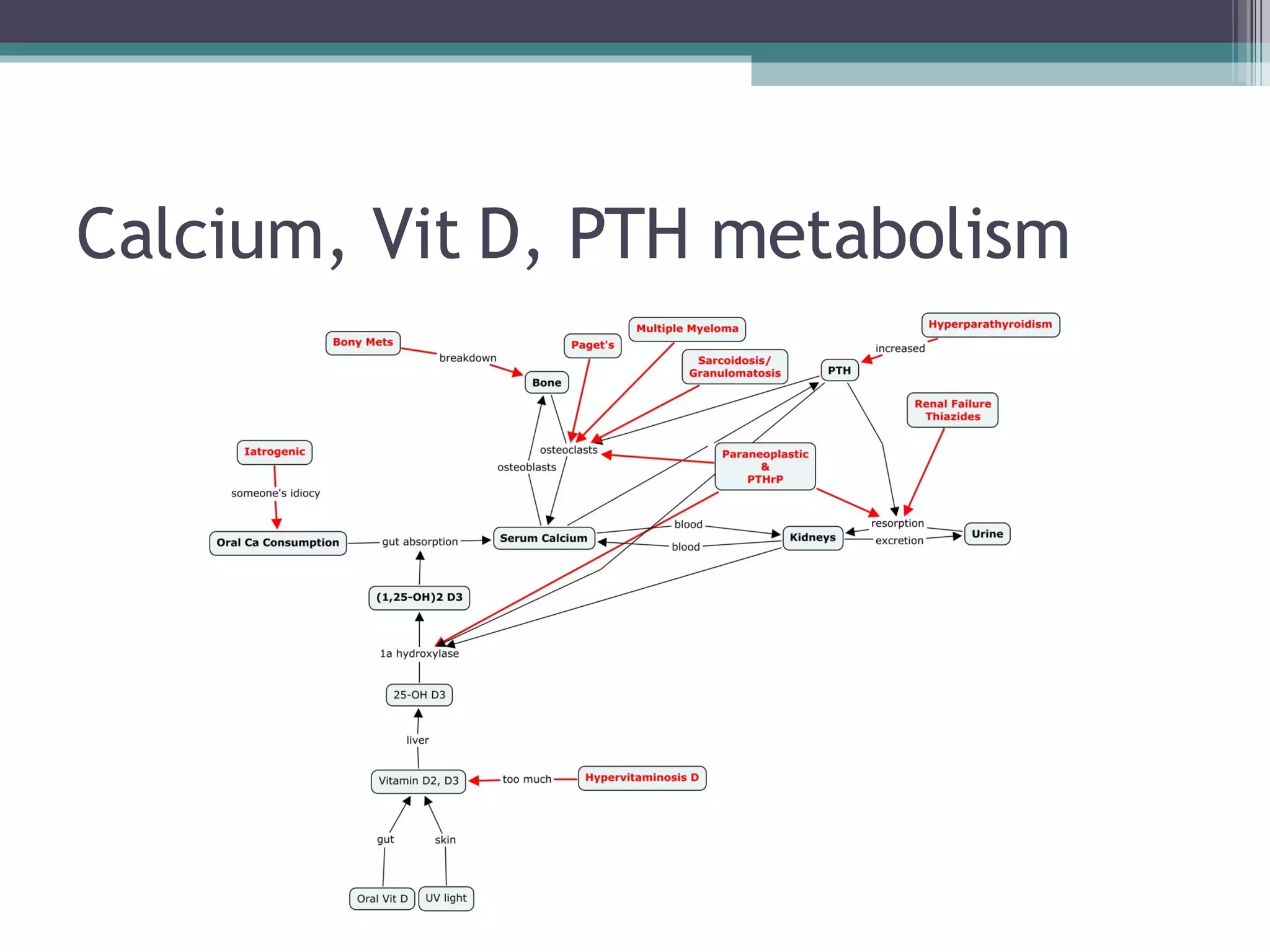
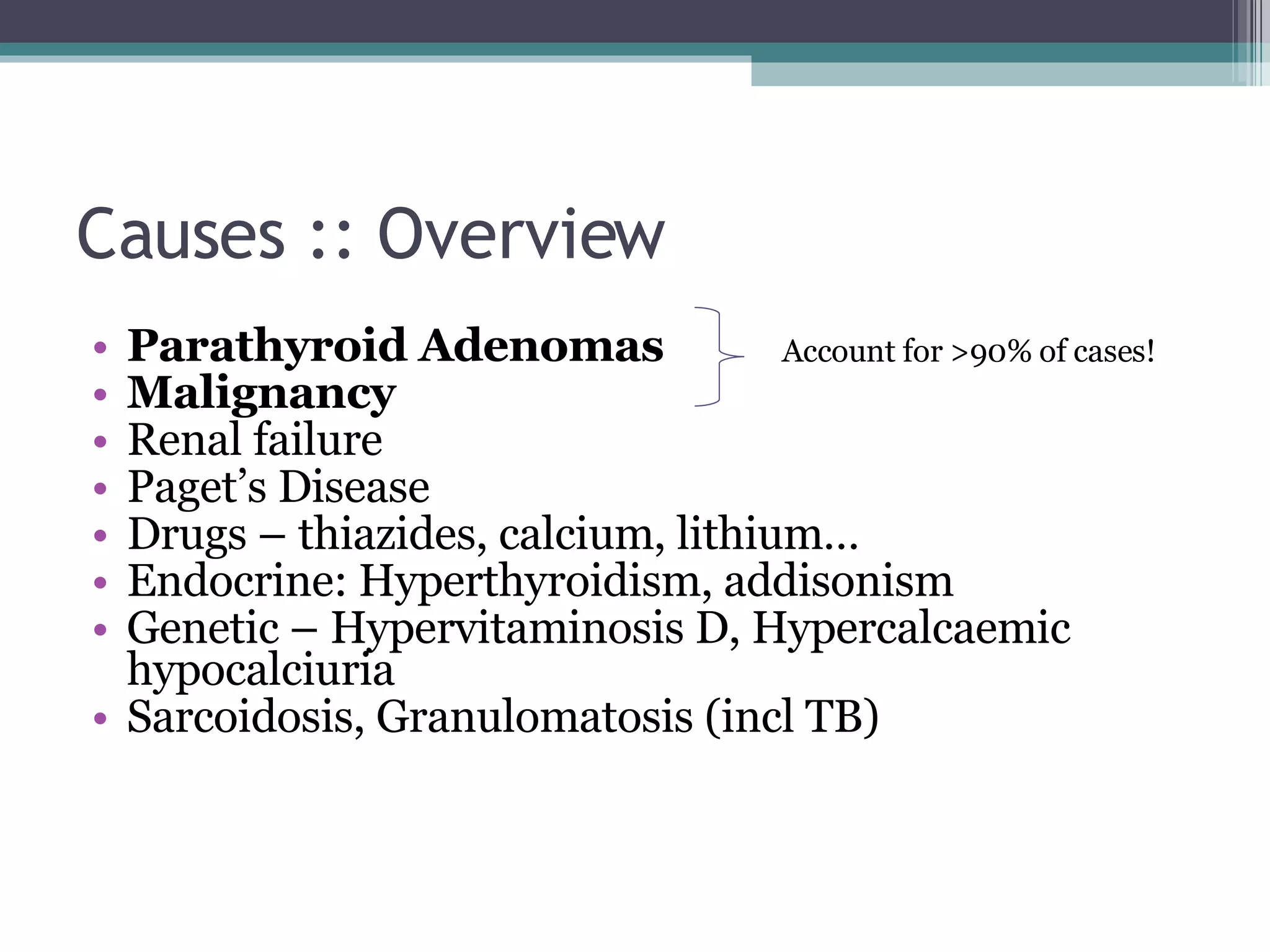
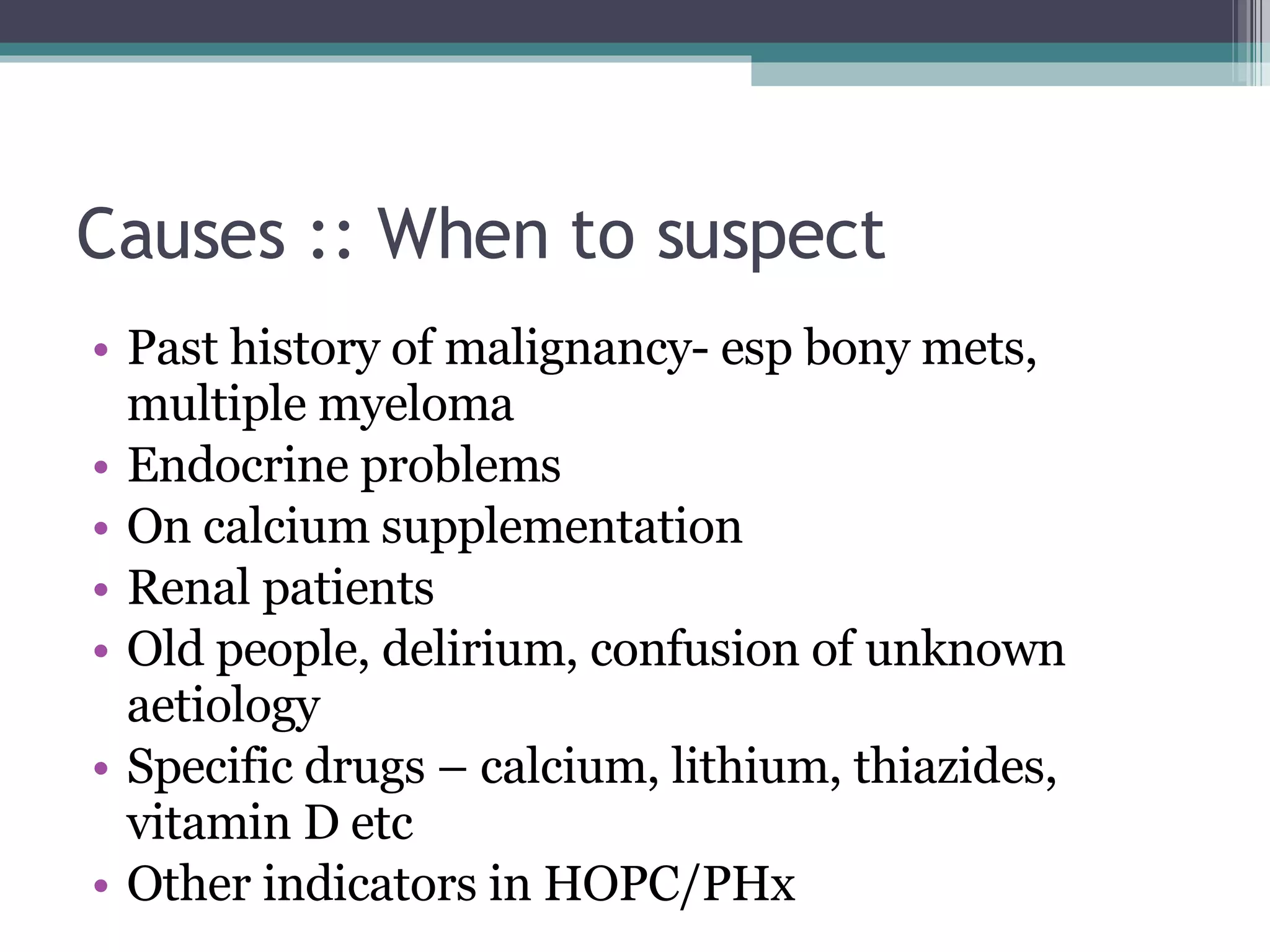
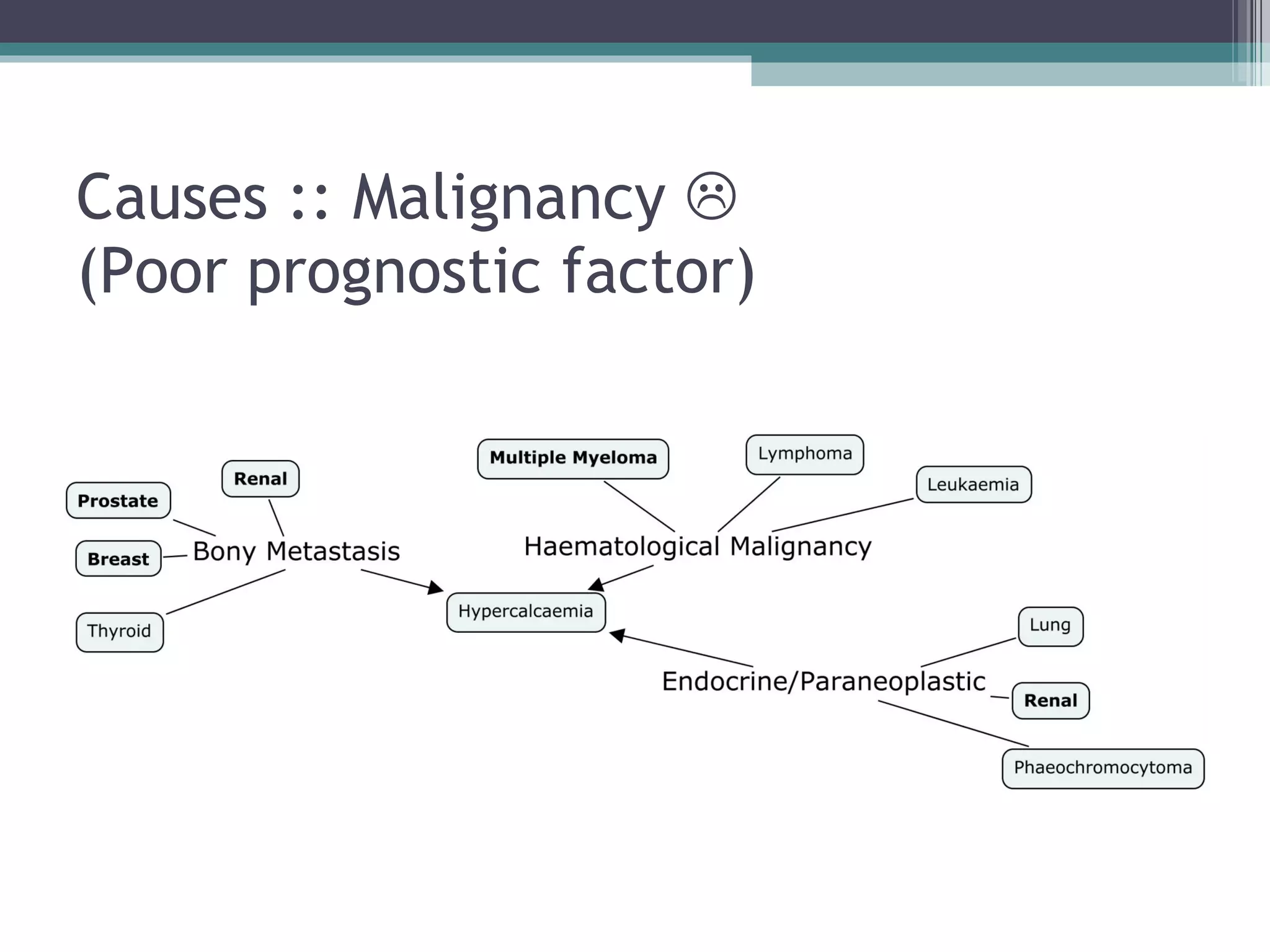
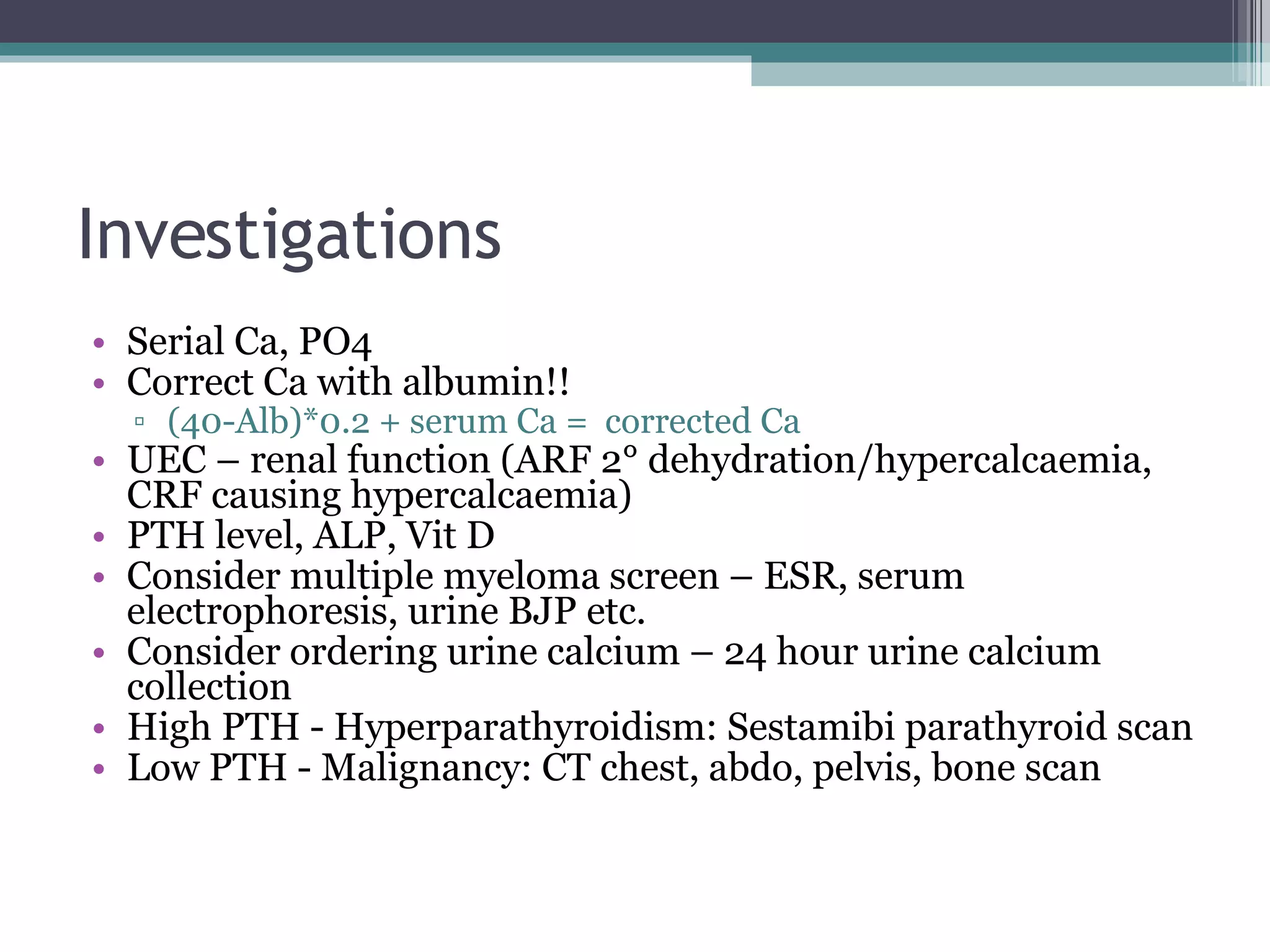
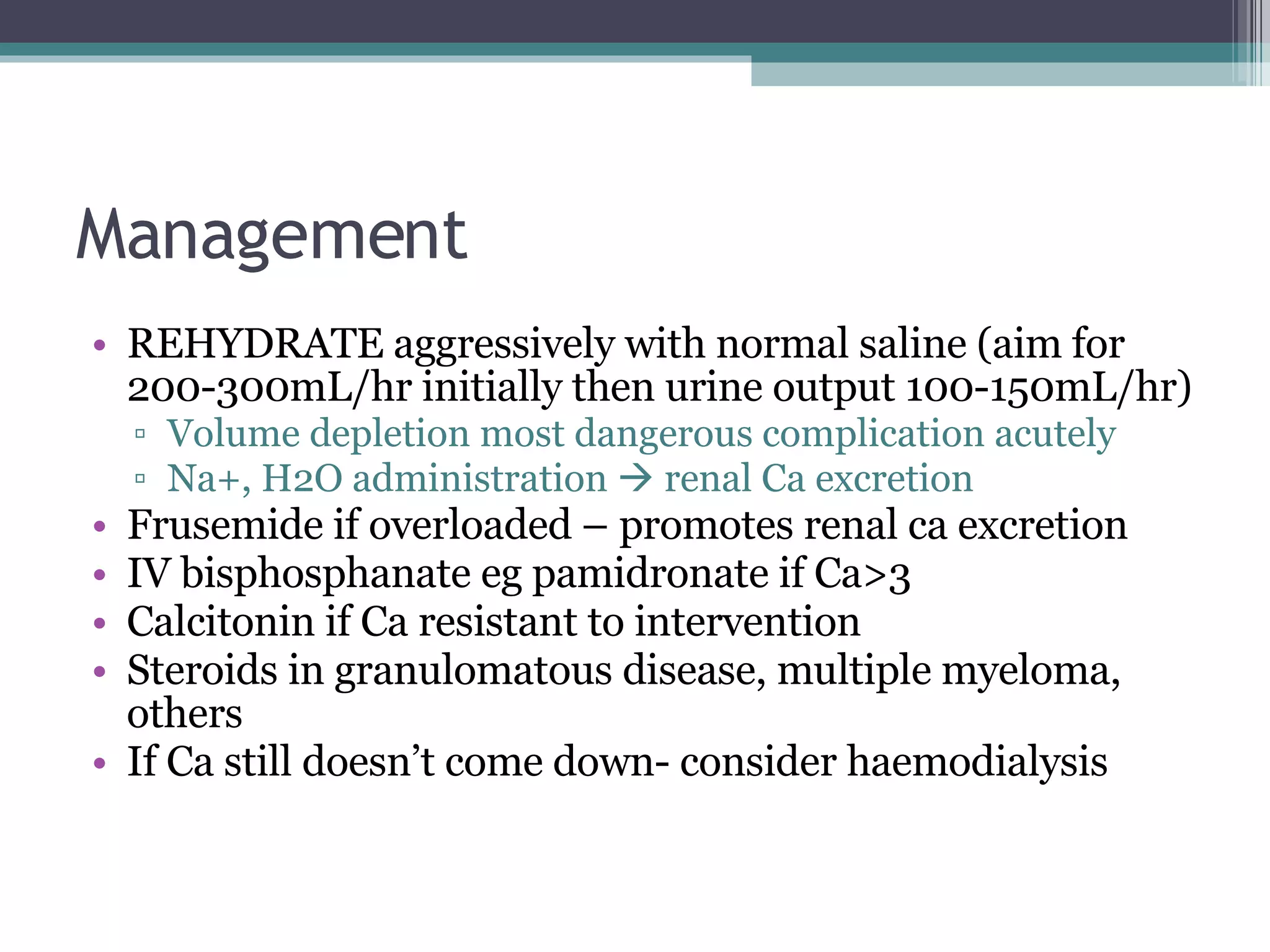
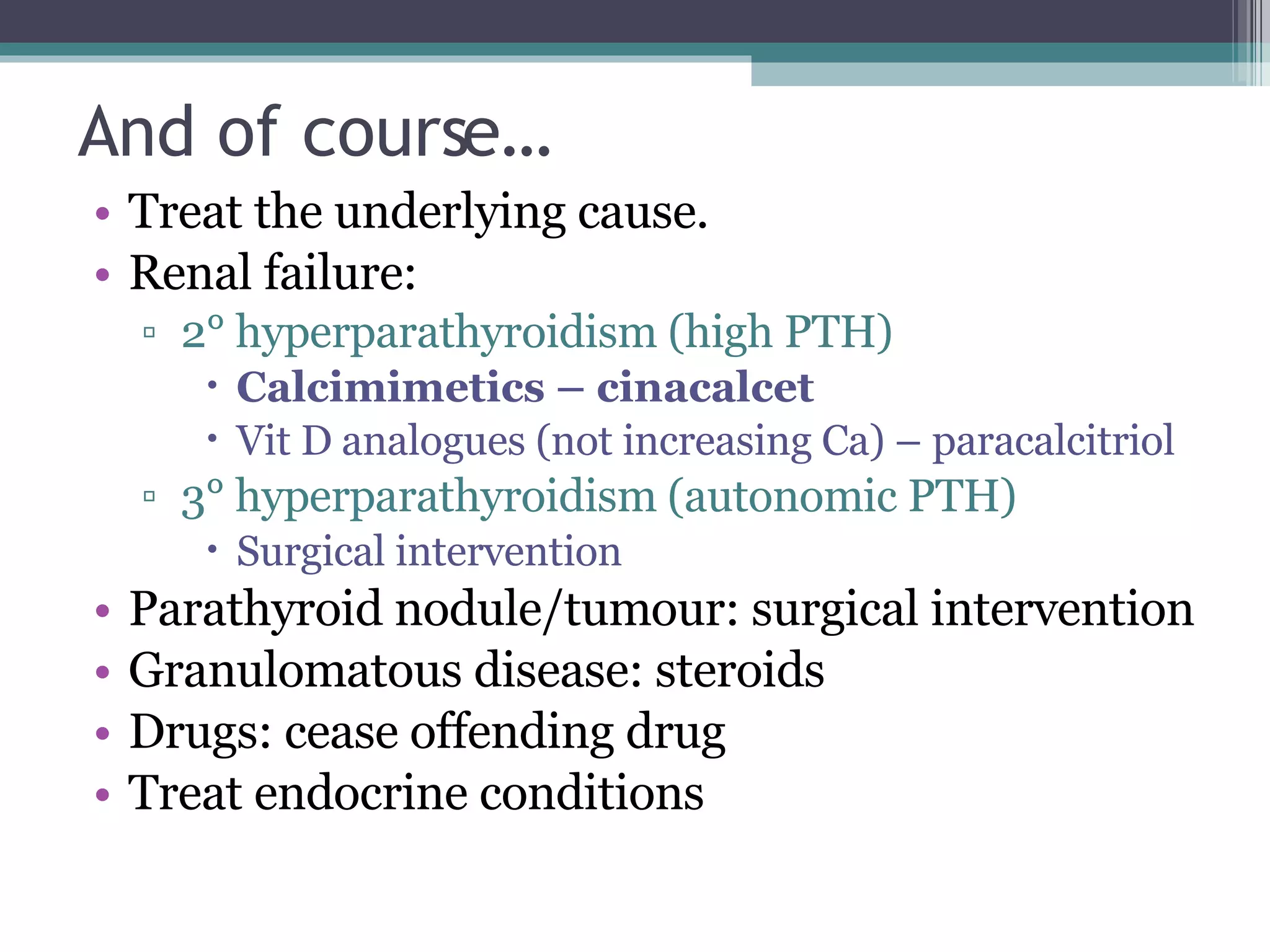
This document presents the case of an 80-year-old woman with metastatic breast cancer and a history of parathyroid adenoma who presented with vomiting, diarrhea, fatigue and severe abdominal pain. Initial workup found hypercalcemia likely due to both bony metastases and primary hyperparathyroidism. She was aggressively rehydrated and further testing found suppressed PTH levels, supporting the diagnosis of hypercalcemia secondary to bony metastatic disease rather than parathyroid adenoma. Her calcium levels responded well to intravenous fluids and she was managed conservatively.