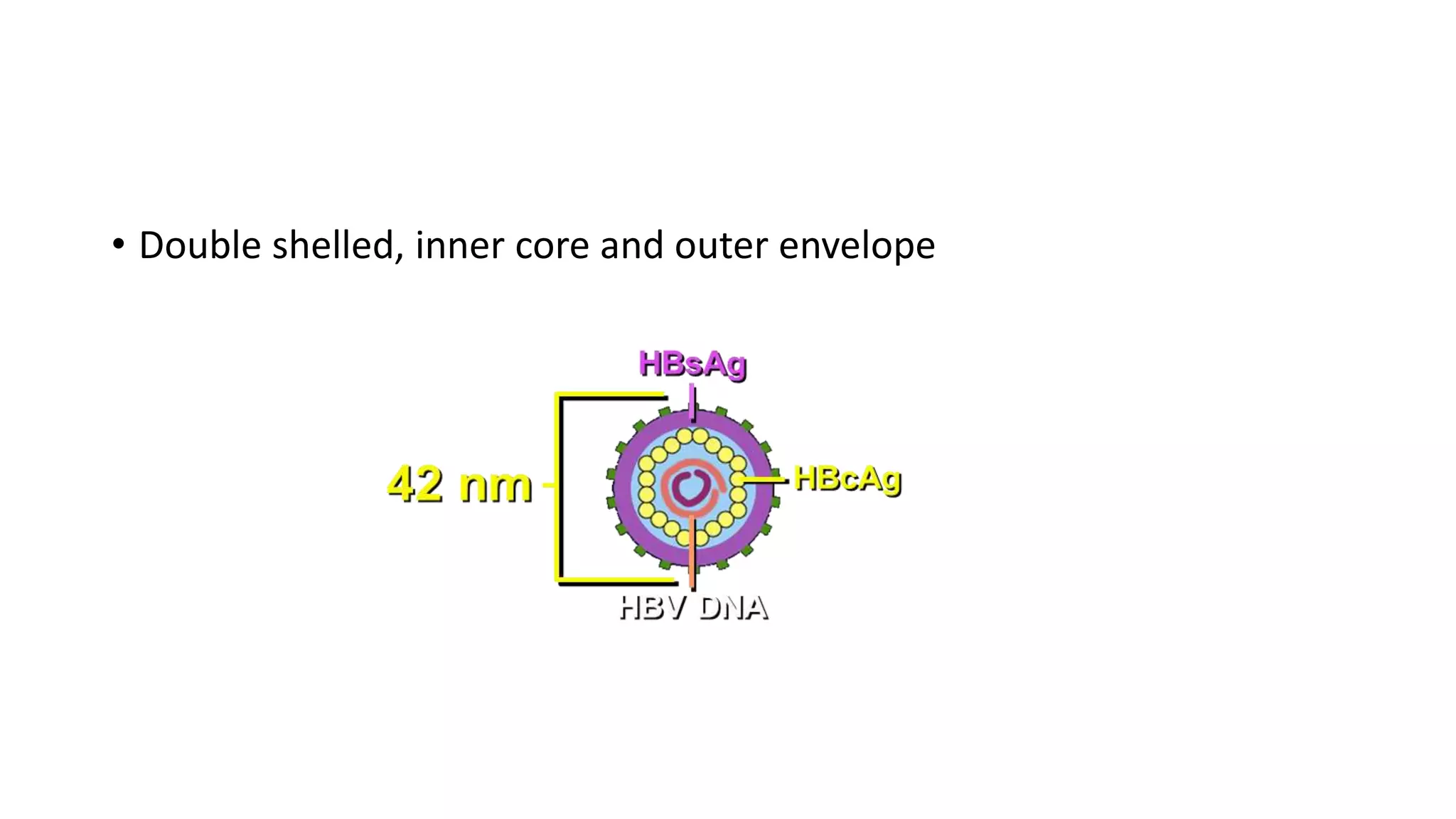
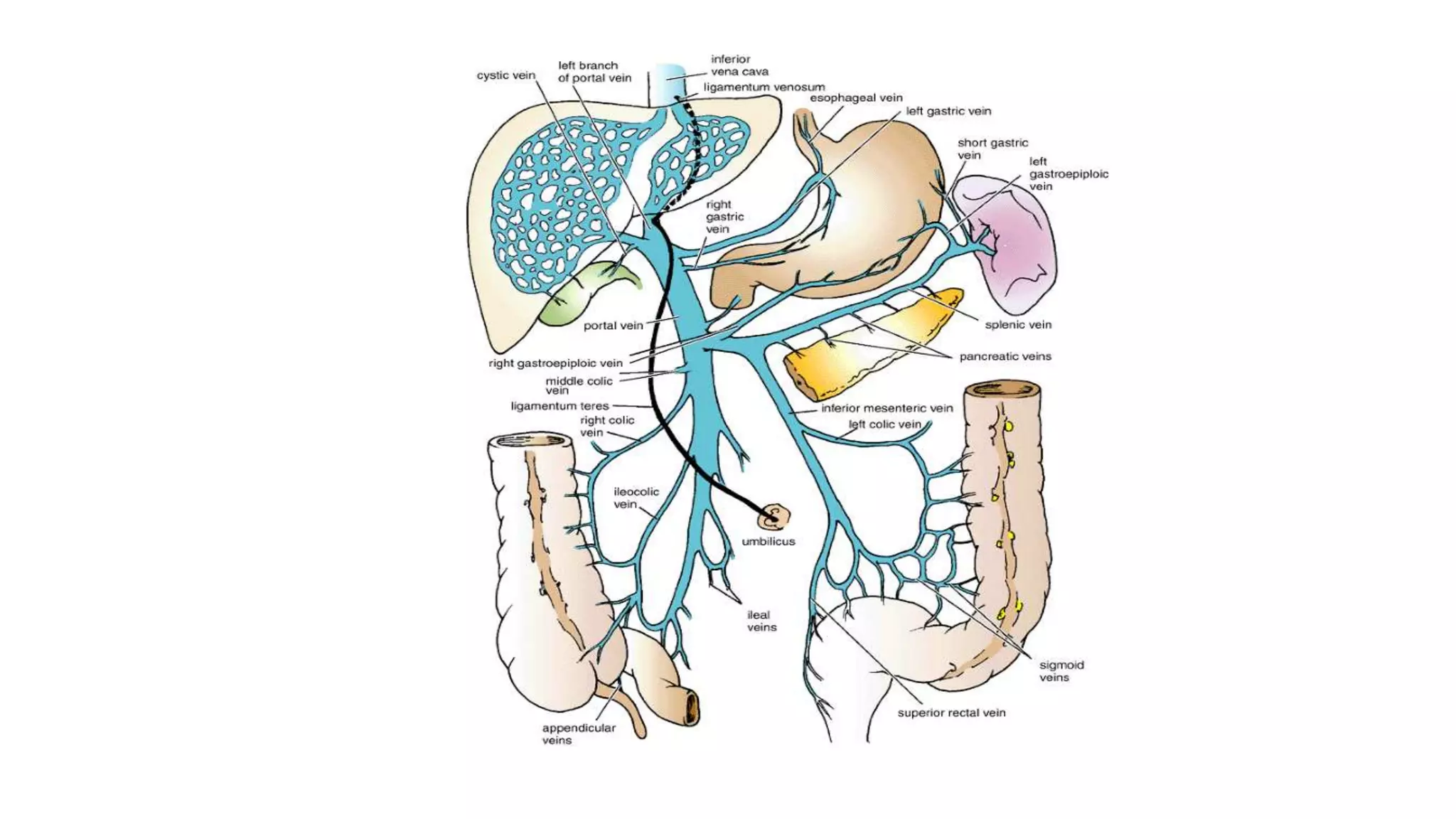
This document discusses hepatitis and its complications. It defines hepatitis as inflammation of the liver and classifies it as either acute or chronic based on duration and viral, drug-induced, autoimmune, or other etiologies. Clinical features of acute and chronic hepatitis are described. Specific viral causes like hepatitis A, B, C, and D are explained in detail including transmission, presentation, diagnosis, and treatment. Other causes of hepatitis like drugs, alcohol, and autoimmune hepatitis are also outlined. Complications of chronic liver disease like cirrhosis and portal hypertension are defined and their clinical features and management described.