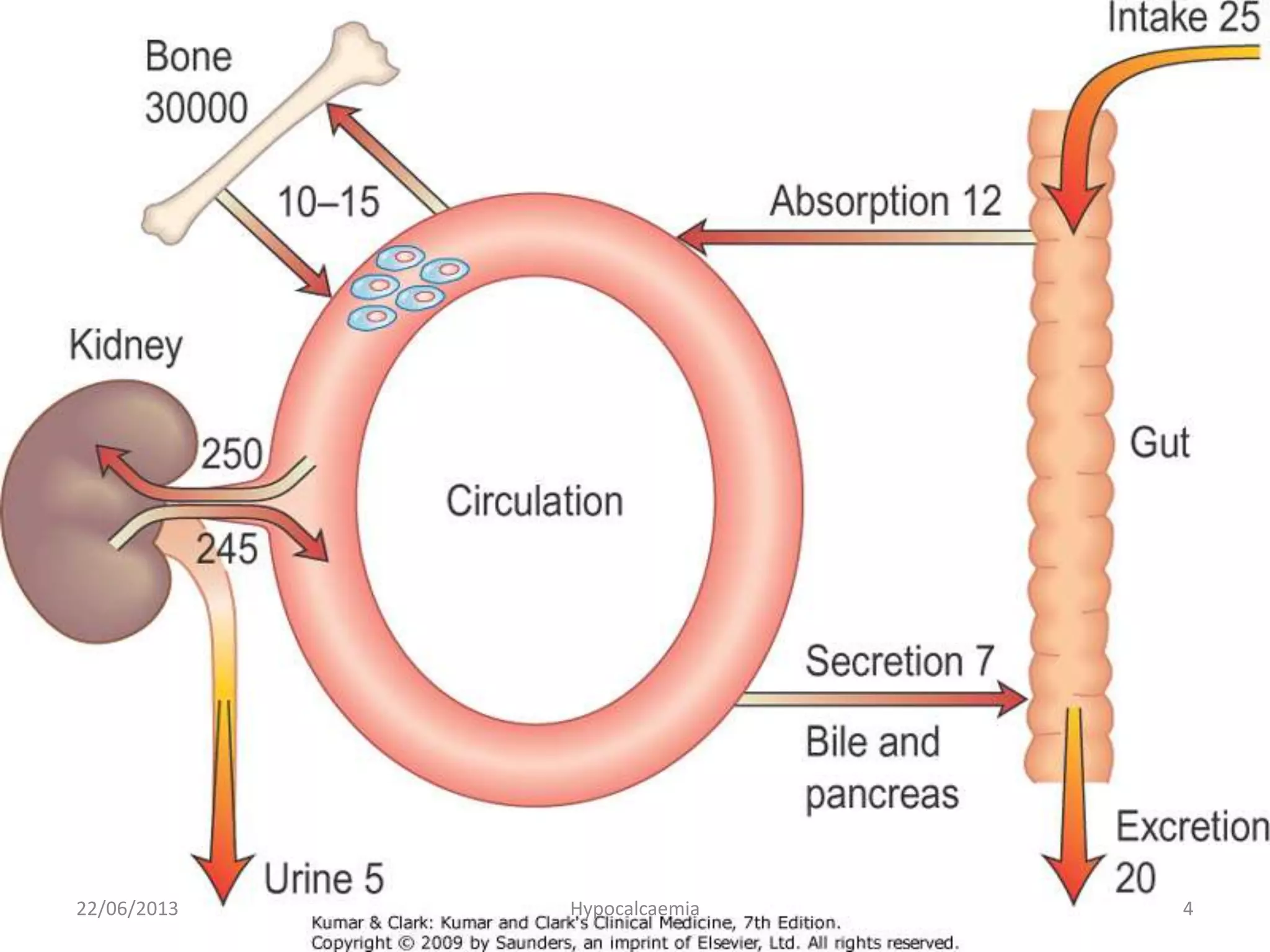
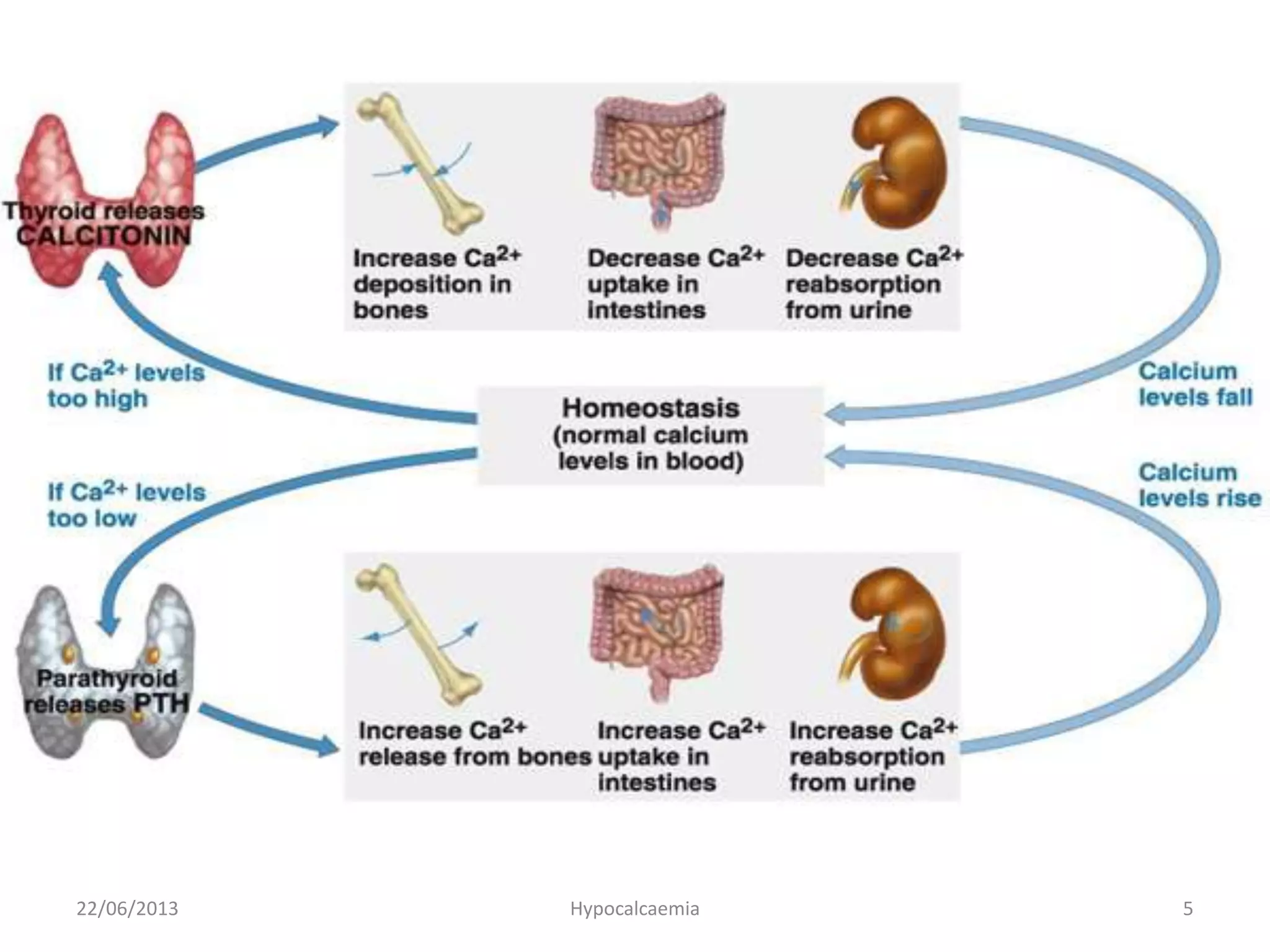
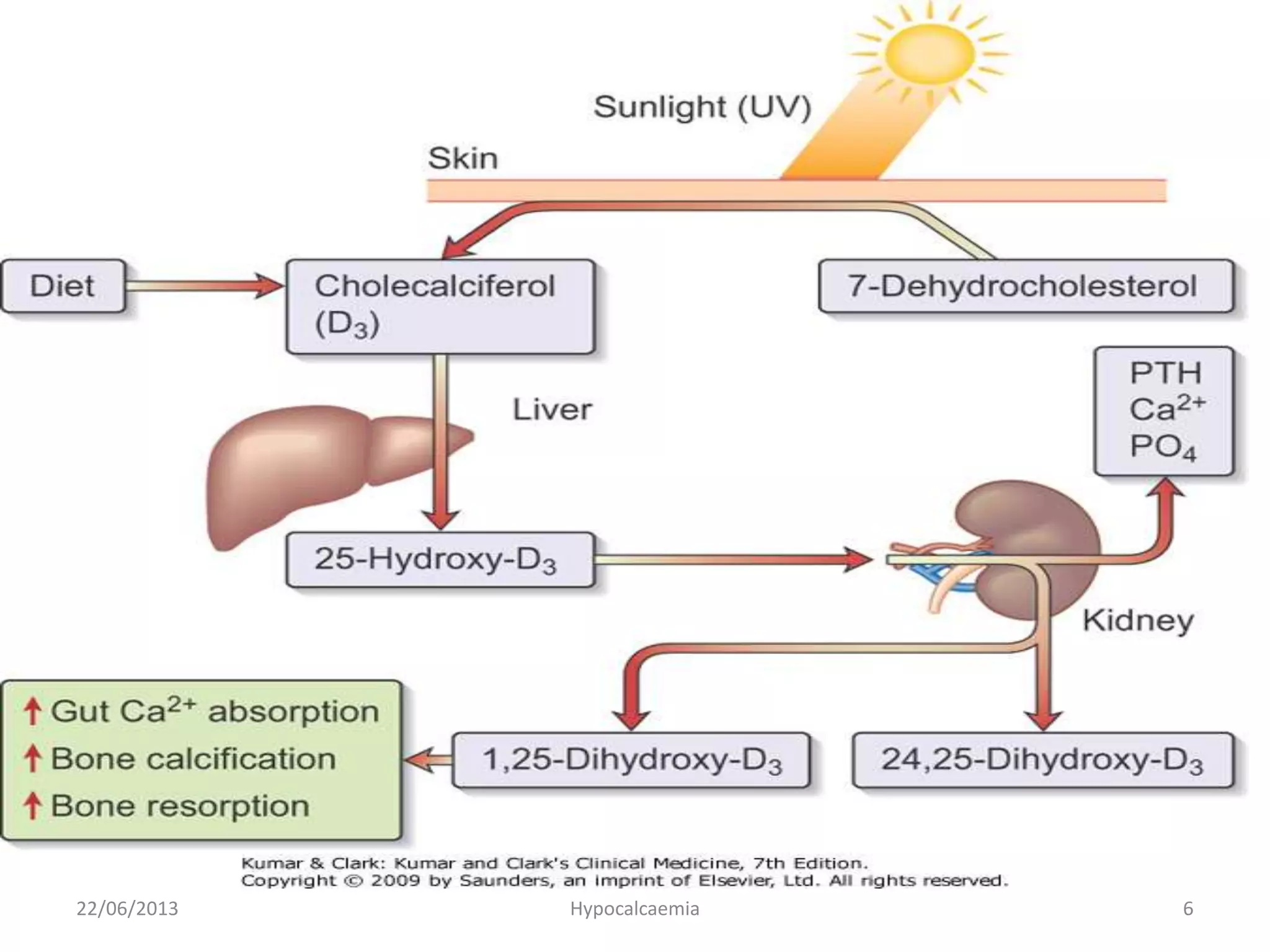
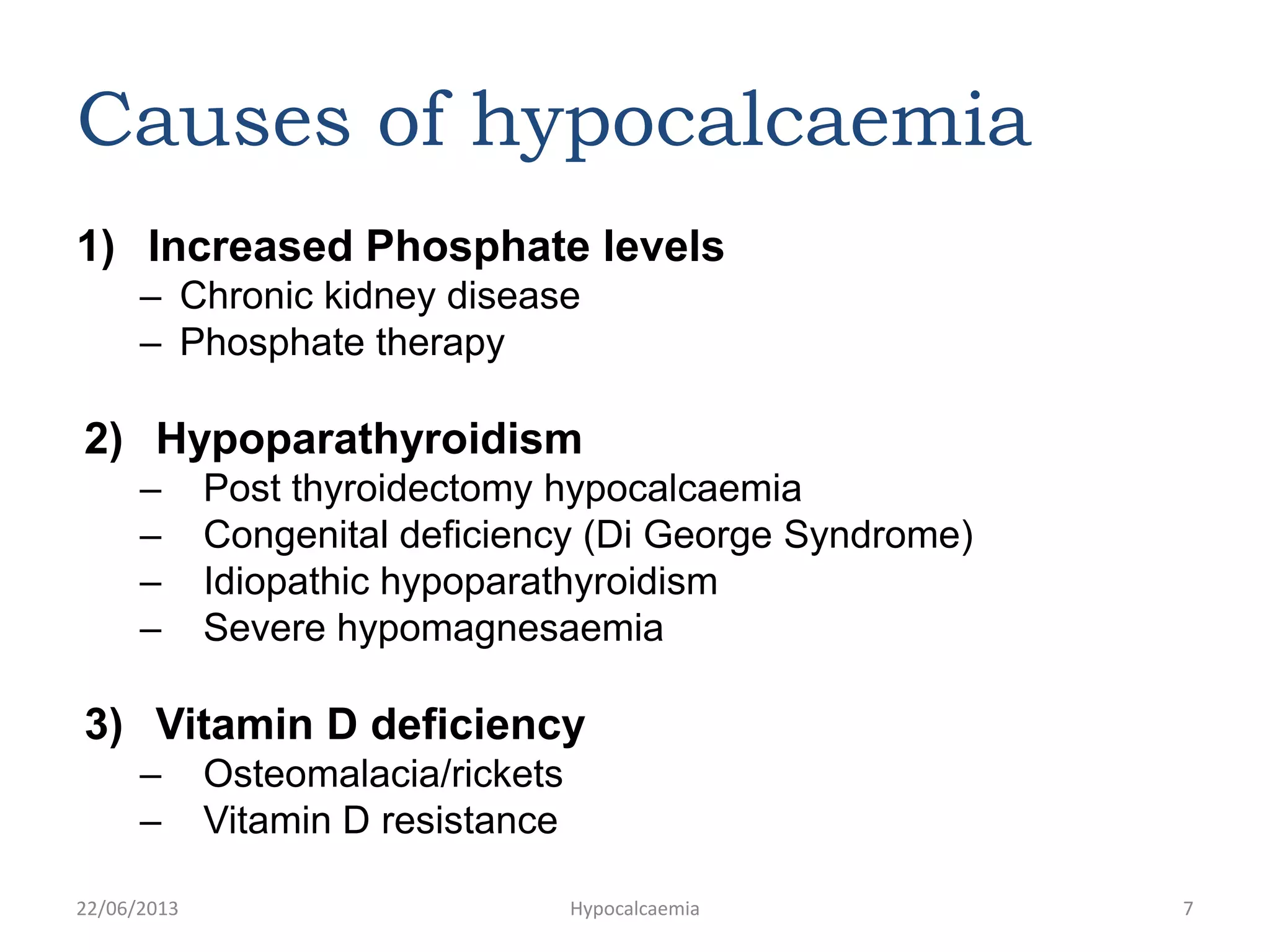
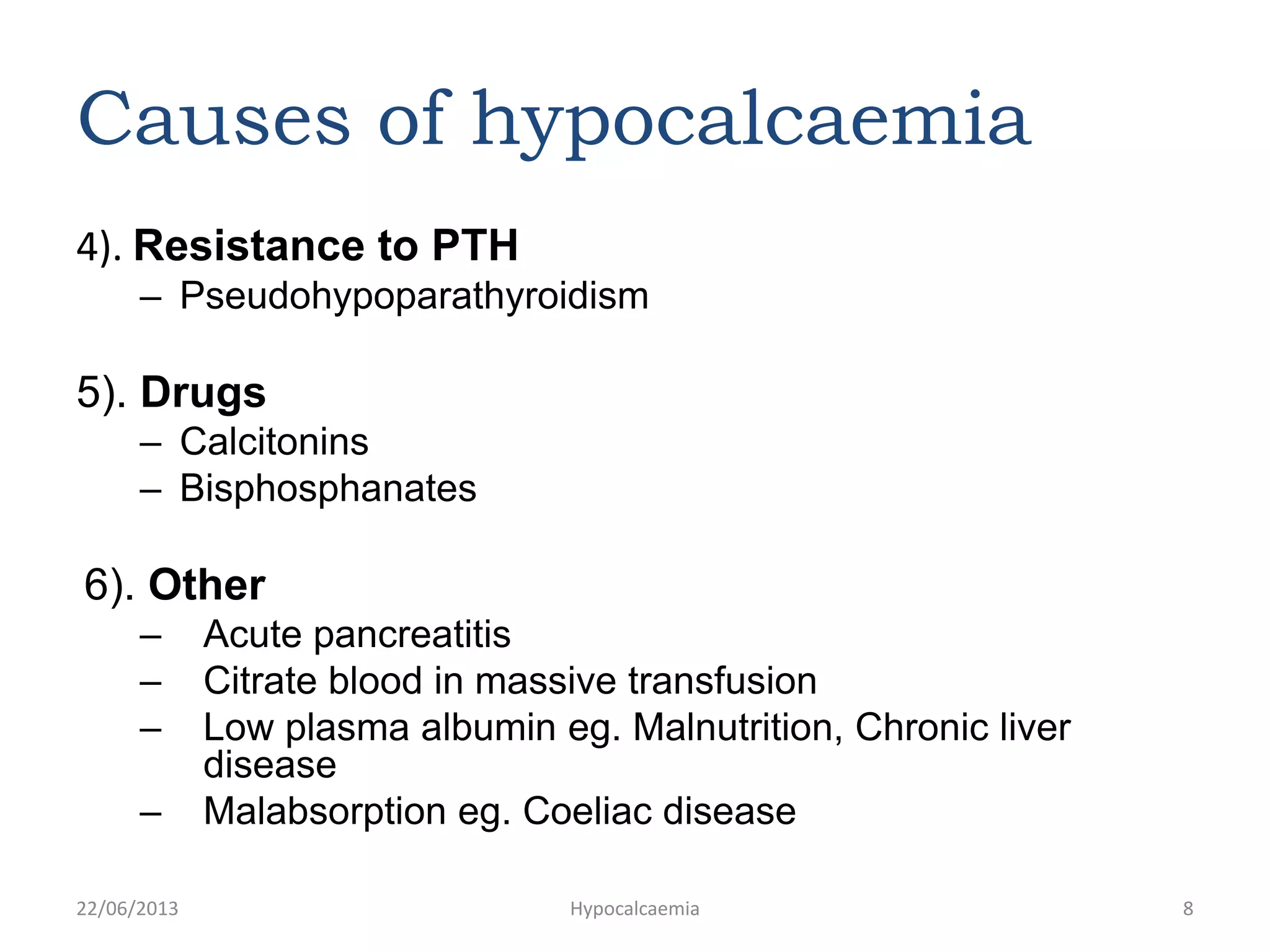
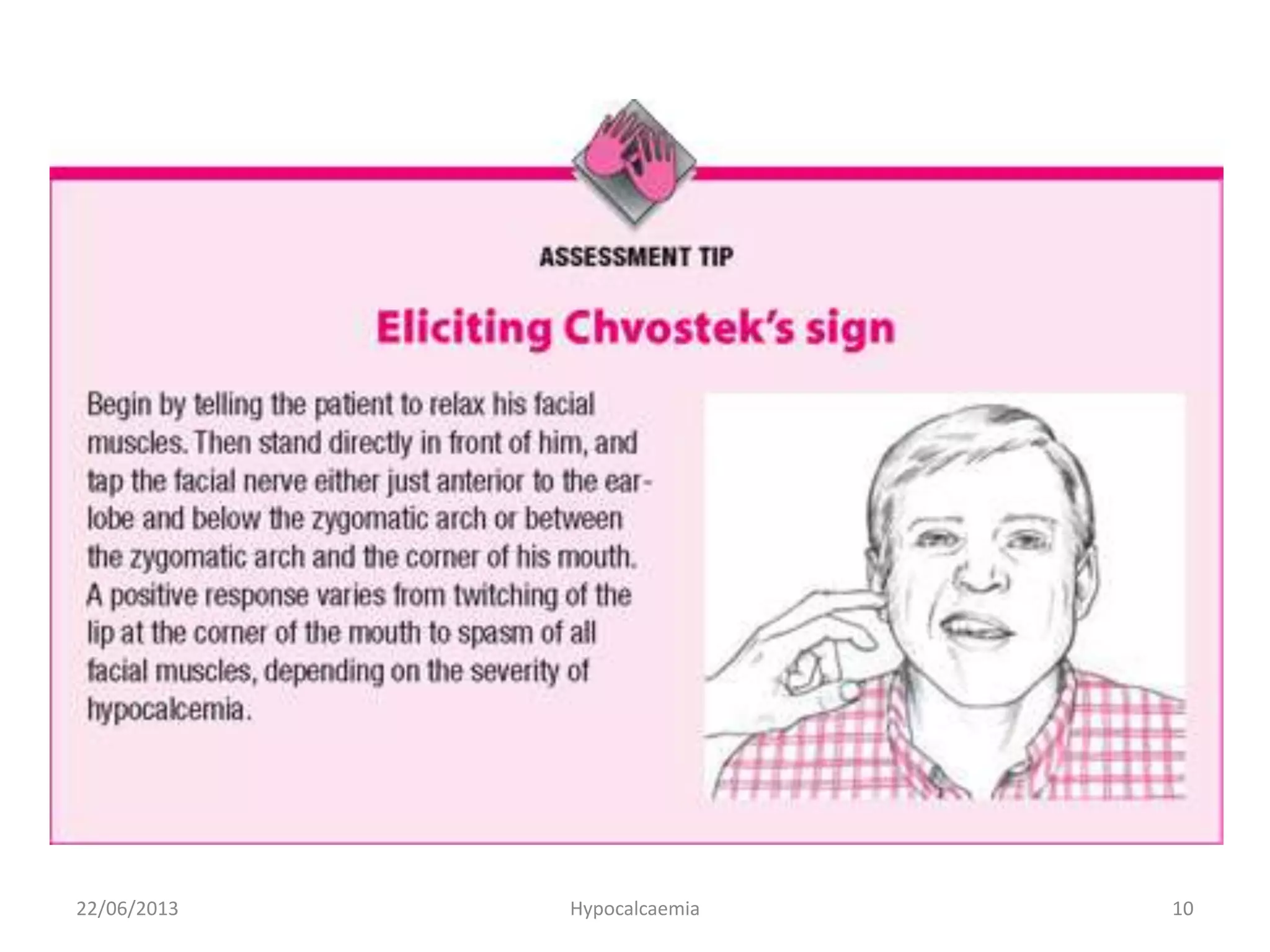
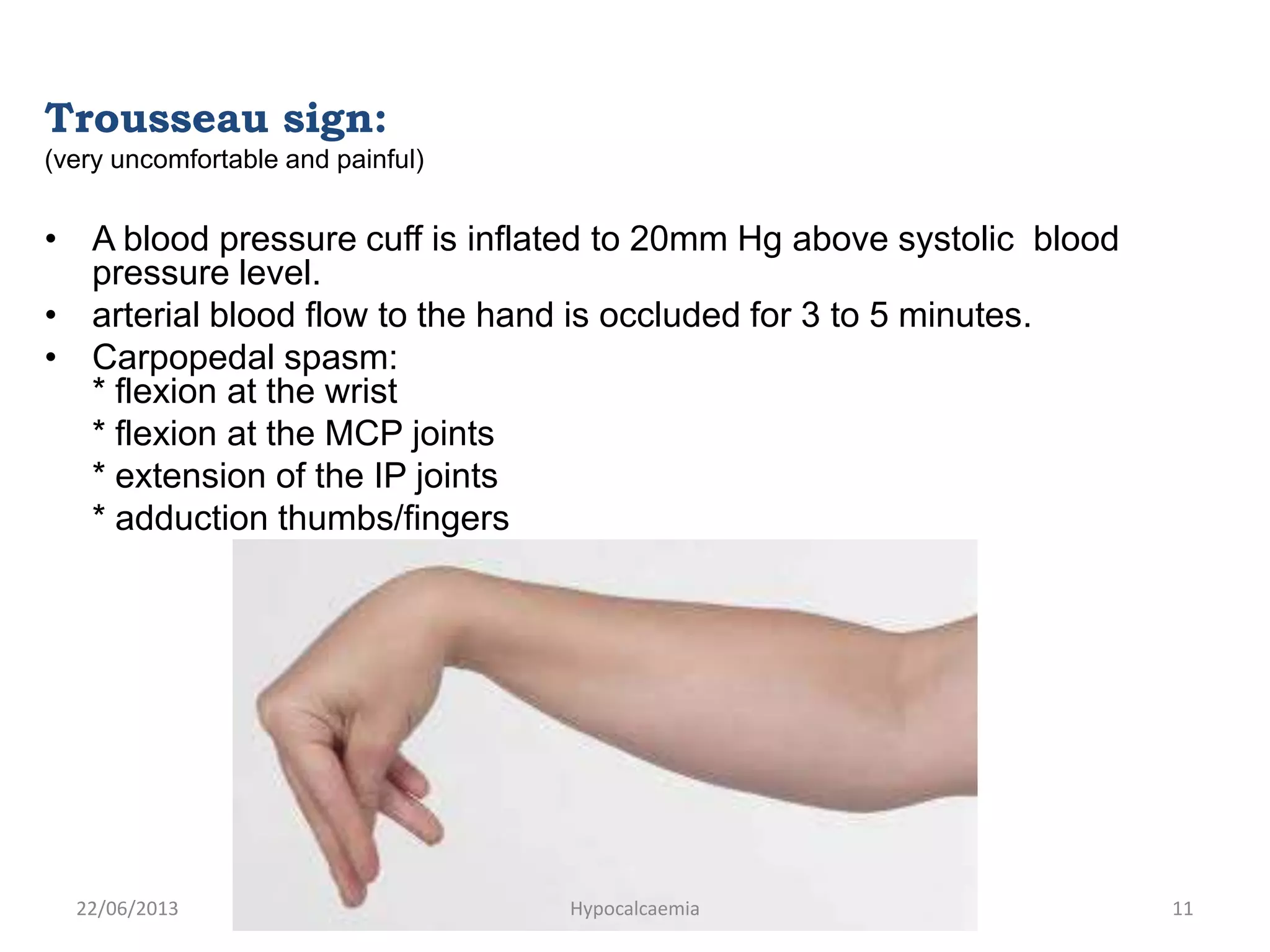
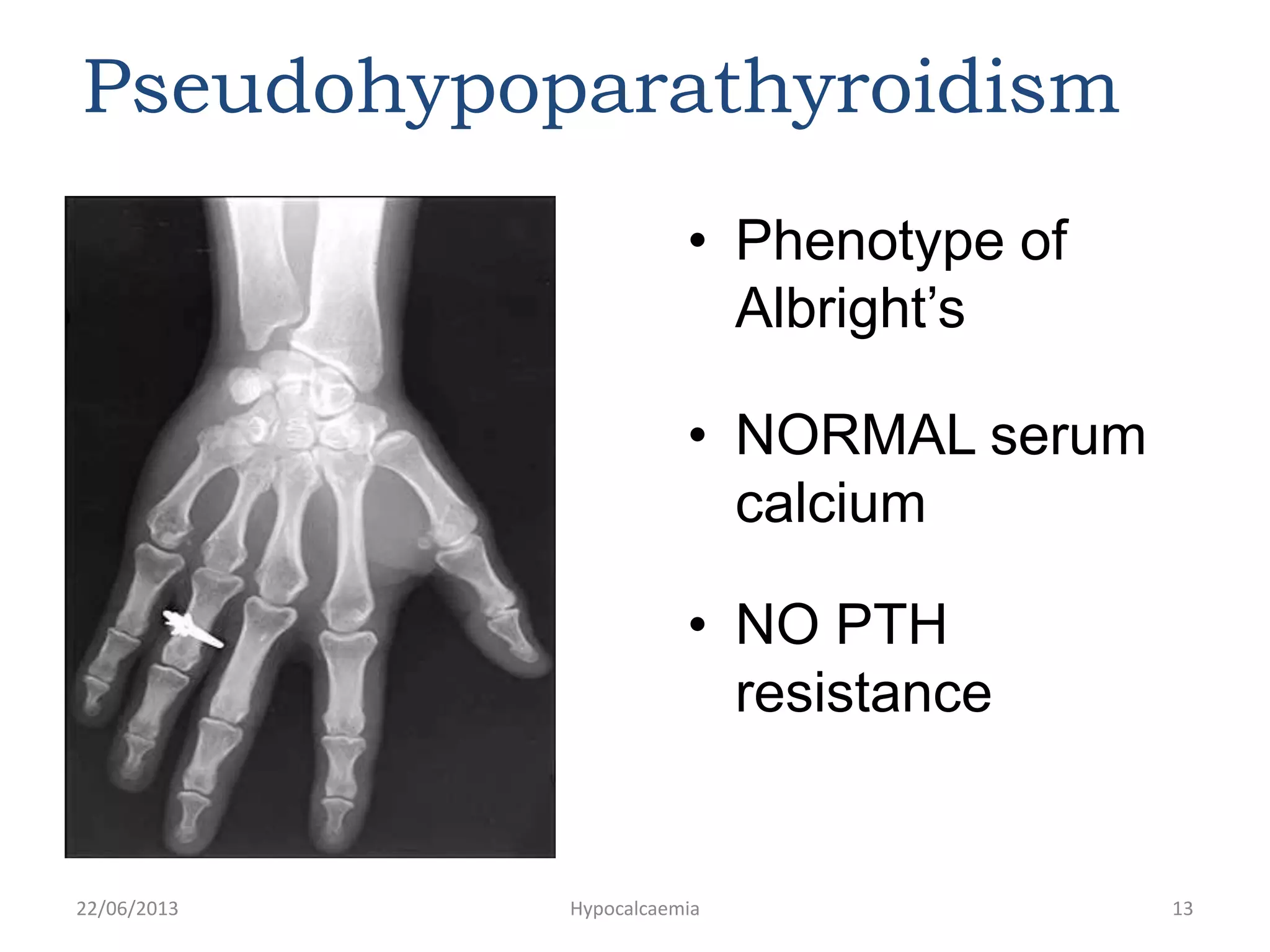
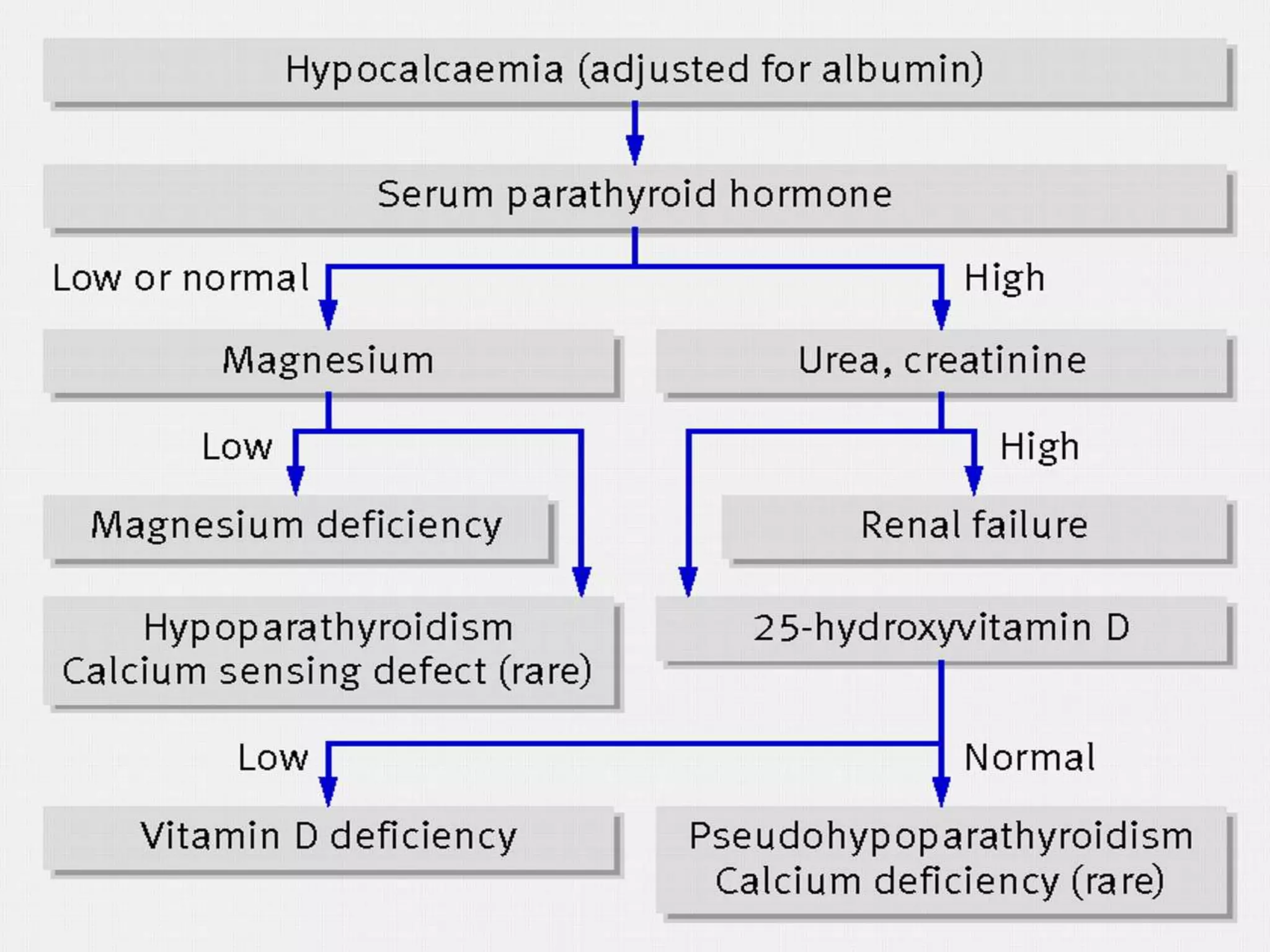
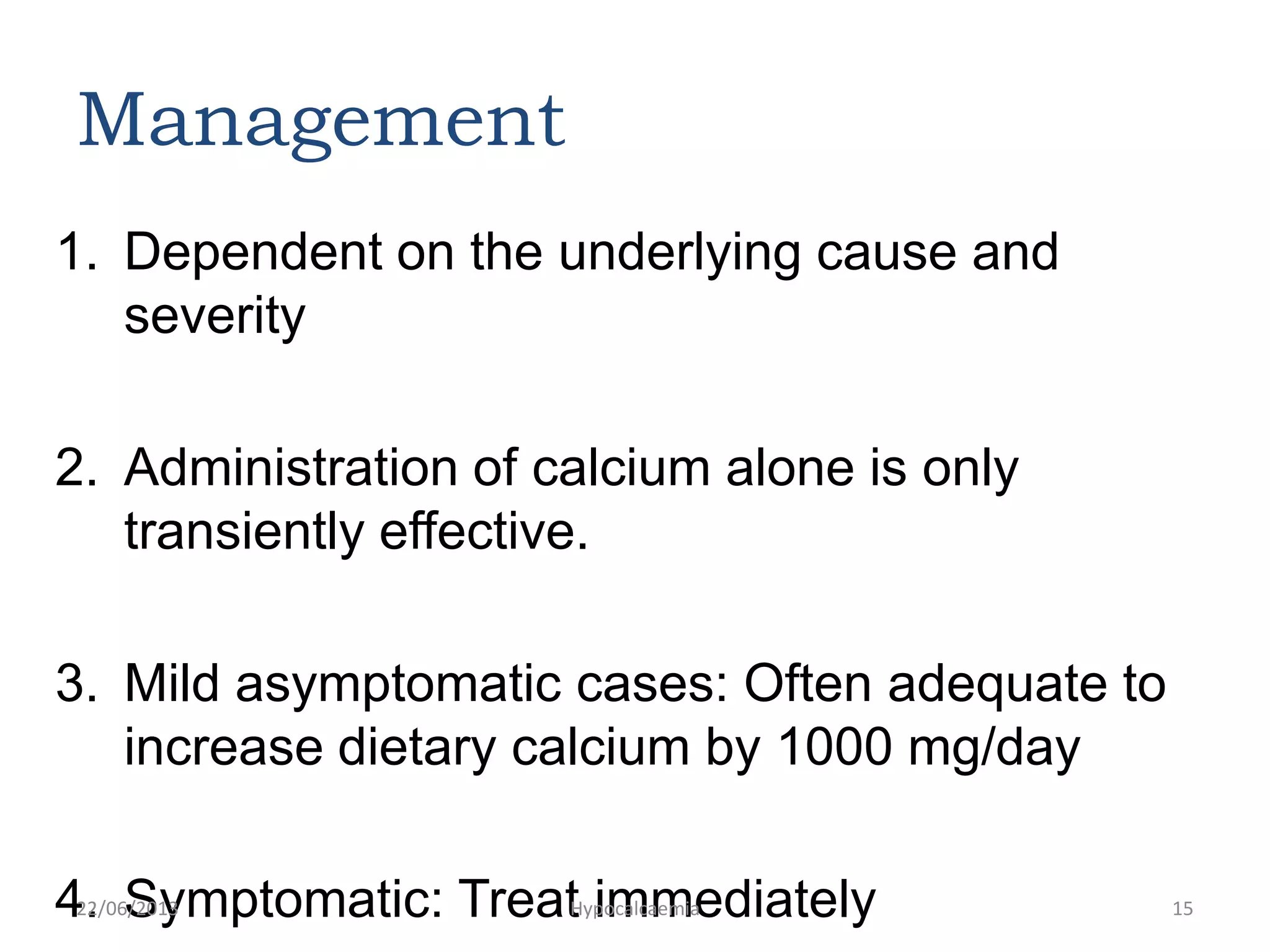
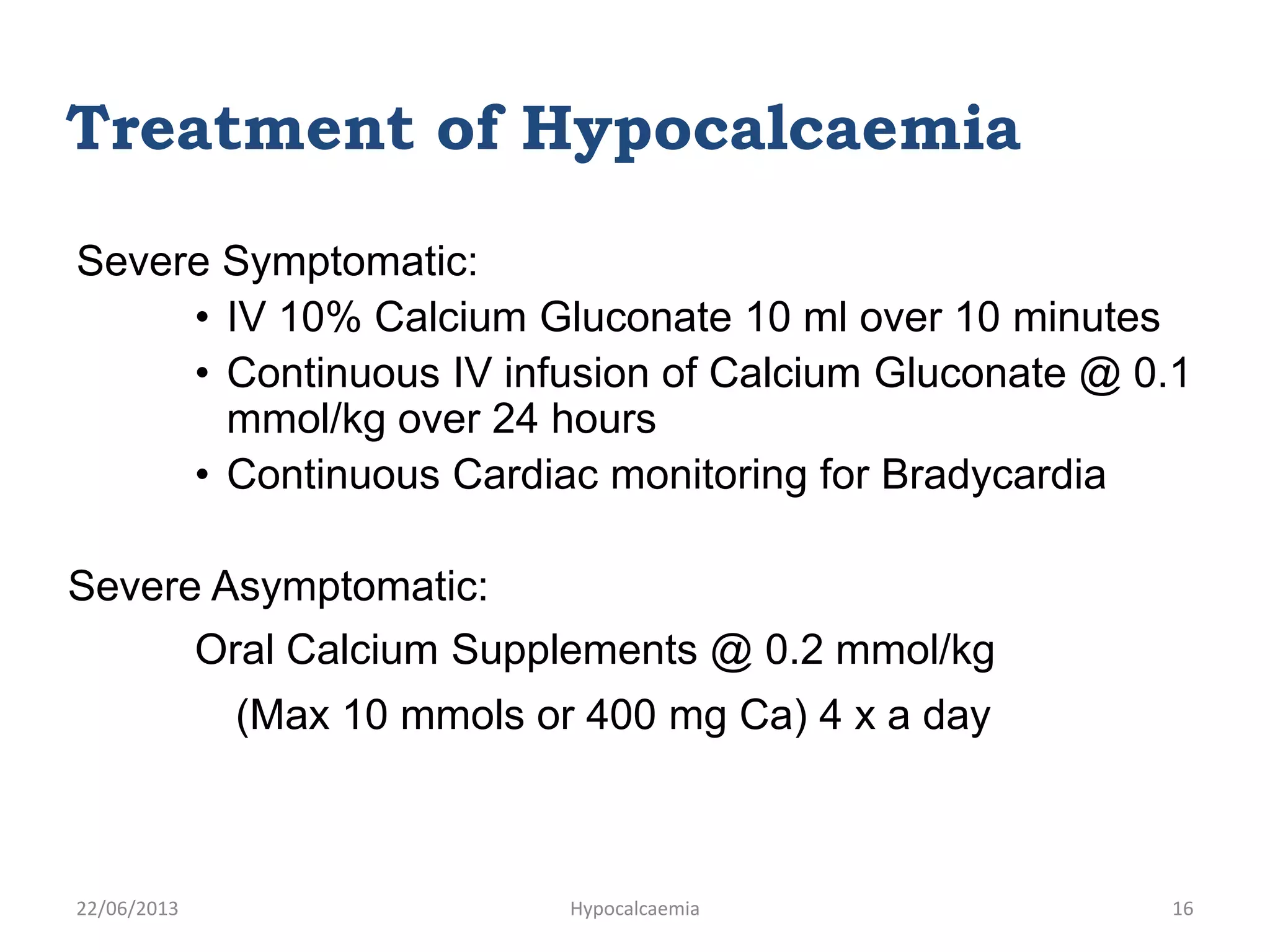
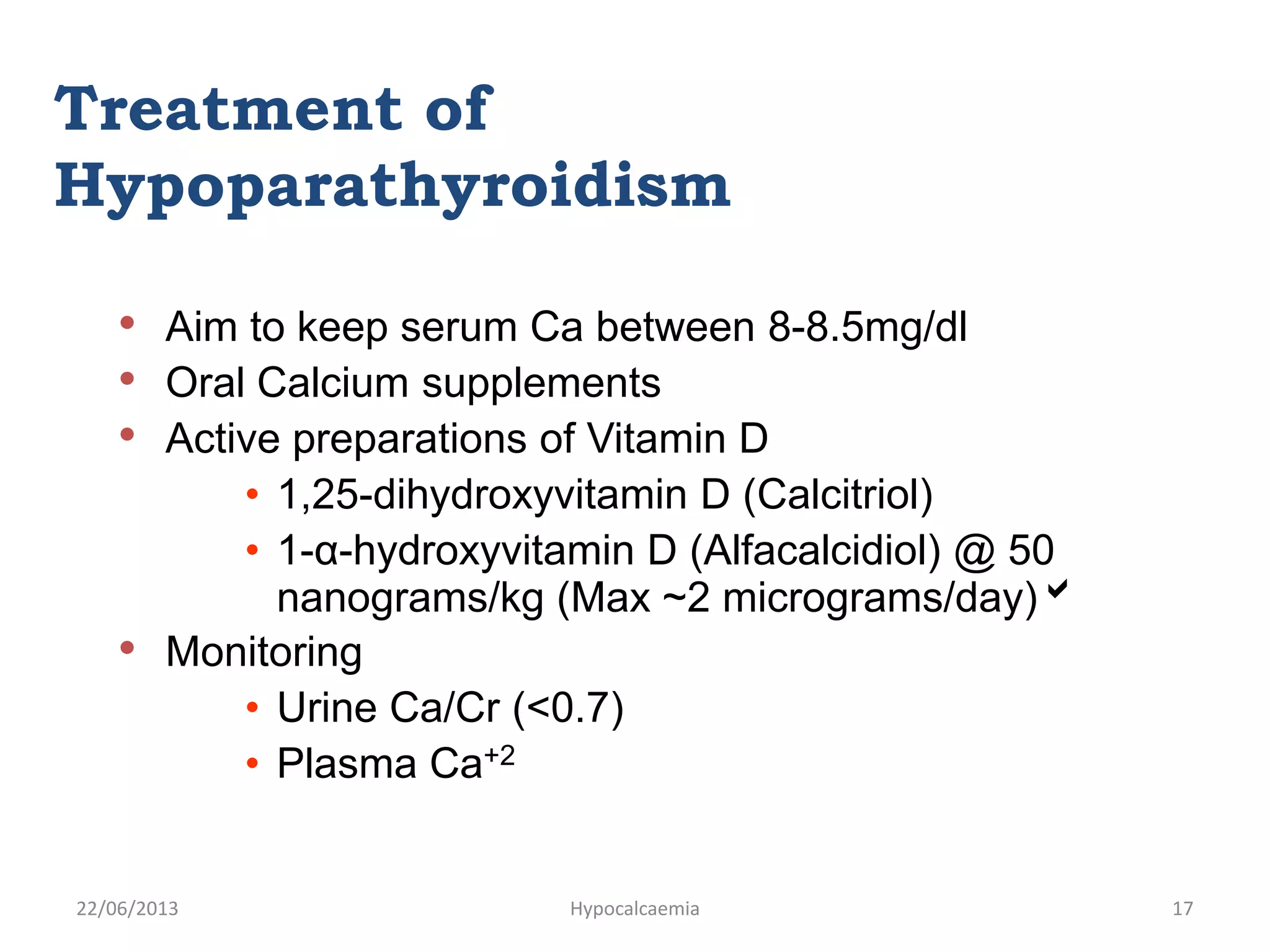
This document discusses hypocalcemia, which occurs when calcium levels in the blood are too low. It defines normal calcium levels and describes the causes of hypocalcemia, including kidney disease, hypoparathyroidism, vitamin D deficiency, certain drugs, and other conditions. Symptoms can include tingling, muscle cramps, seizures, and cardiac issues. Diagnosis involves testing serum calcium, phosphate, albumin, magnesium, parathyroid hormone, and vitamin D levels. Treatment depends on severity but may include oral calcium supplements or intravenous calcium for more severe cases.