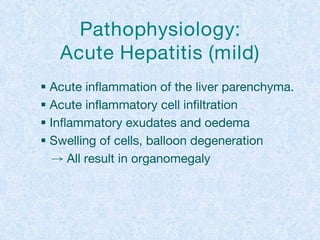
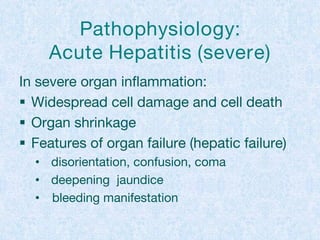
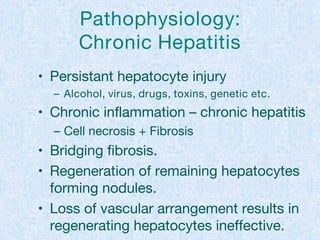
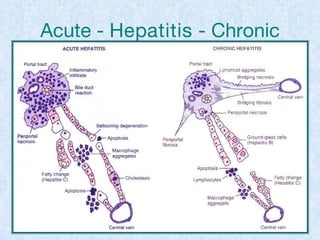
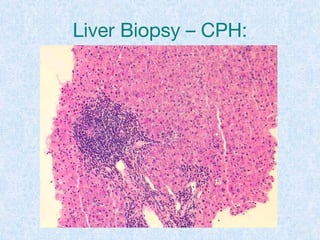
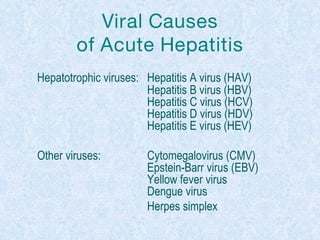
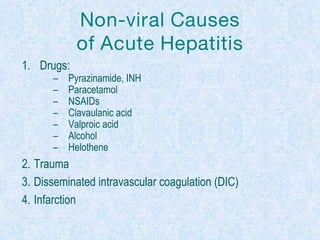
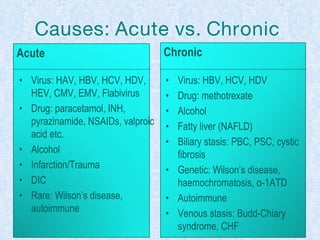
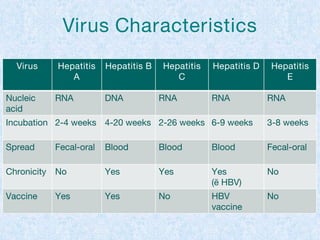
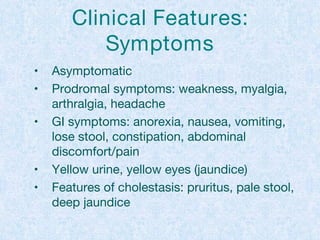
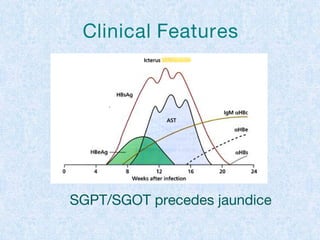
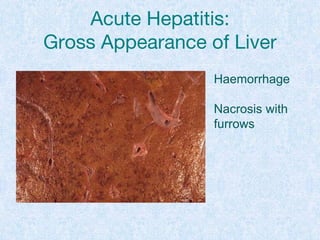
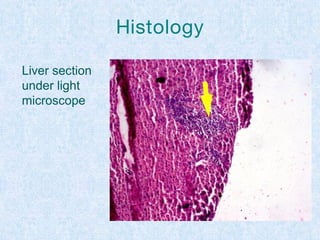
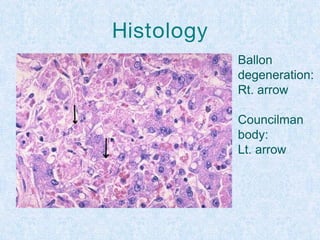
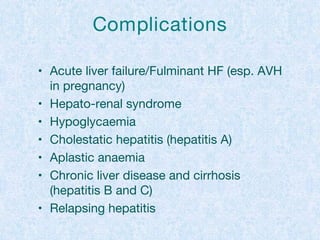
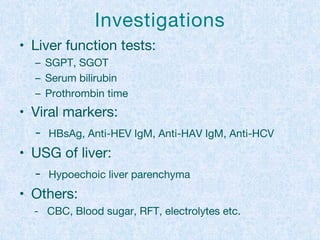
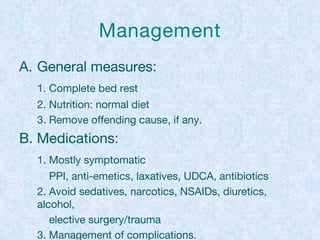
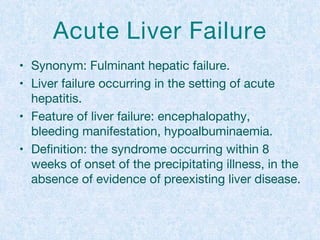
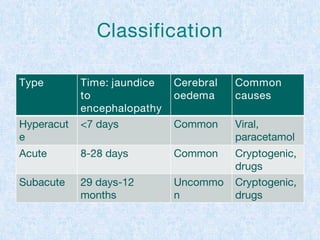
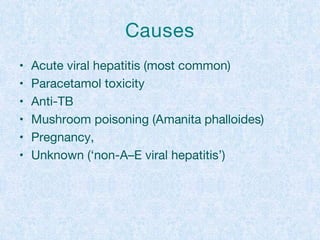
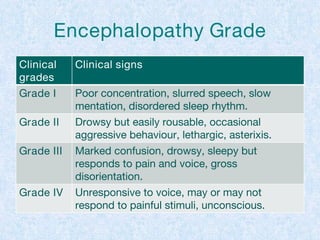
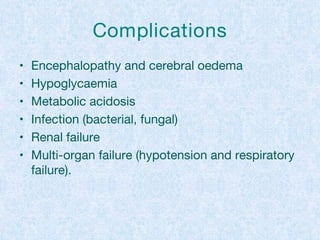
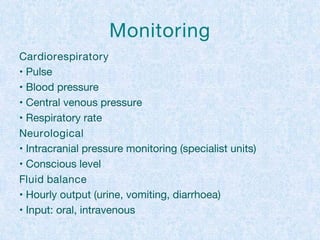
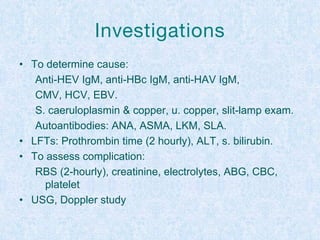
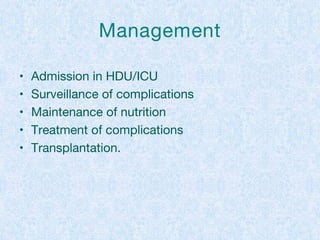
The document discusses acute and chronic hepatitis, including their pathophysiology, causes, clinical features, investigations, and management strategies. It outlines the differences between mild and severe acute hepatitis, explains various viral and non-viral causes, and details complications such as acute liver failure. Management includes general measures like bed rest and dietary adjustments, alongside monitoring and treatment to address complications.