More Related Content
PPTX
Digestive System of Non-Ruminant animals.pptx DOCX
DIGESTION & ABSORPTION OF BIOMOLECULES by Dr. Santhosh Kumar N.docx PPTX
5 digestion absorption of carbs,proteins,lipids.pptx DOCX
L3 - CH66 Absorption & Digestion.docx PPT
5-Digestion and Absorption (1).ppt PDF
DIGESTION OF MACROMOLECULES lecture notes_60342932_2025_05_19_12_31.pdf PPTX
Digestion and Absorption of biomolecules.pptx PPTX
Similar to Hello Digestions and Absorption in GIT.ppt
PPTX
Digestion and Absorption of Carbohydrates, Proteins and.pptx PPTX
DIGESTION ,ABSORTION AND ASSIMILATION OF NUTRIENTS PPTX
Carbohydrate metabolism i PPTX
PPTX
Digestion and absorption.pptx PDF
Digestion, absorption and transport of food PPTX
CN UNIT MACRONUTRIENTS AND DIGESTION 1.pptx PPT
PPTX
4_6051023997057895317.pptx PDF
Digestion and absorption of carbohydrates.pdf PPTX
Digestion and absorption of Carbohydrates proteins and lipstick PDF
Protein_Digestion_NASPGHAN.pdf PPTX
Metabolism new with complete explanation.pptx PDF
2 Carbohydrate metabolism all topics.pdf PPTX
DIGESTION AND ABSORPTION.powerpoint presentation PPTX
PDF
Gastrointestinal Physiology PPTX
Digestion and absorption of food PPT
Physio git 9,10 plus mc qs. PDF
Carbohydrates digestion_compressed.pdf and absorption Recently uploaded
PPTX
LESSON-6.pptx ooppppsjspppappppapppppapppp PDF
How to Prepare for AWS Certified Solutions Architect Associate Certification ... PDF
This digital marketing infographic shows how the right online strategies turn... PPTX
presentationonformalletter-150118050817-conversion-gate01.pptx PPTX
Black and White Modern Industrial Revolution Presentation.pptx PPTX
Principles of Exercise Prescription.pptx PPTX
20220315-Core_Education_Op_Law_F2F_Presentation_Final_v2 (1).pptx PDF
Worksheet for Math class unit Area grade 5-6 DOCX
Buy Verified Cash App Accounts – 100% Safe, 4k BTC and Non-BTC PDF
CLSSBB - (Refresher SSAA - Six Sigma Academy Amsterdam) PDF
Randy Siwiec Office of the Dir of National Intelligence PPTX
Career and Business Opportunities in Industrial Arts PDF
Modern Project Management with AI, Agile & Hybrid by APMIC PDF
Crime Prevention Isn’t Just for Cops: How Everyday Actions Make a Safer World PDF
Pupil's book for year 6pgf or doloand at this page PDF
Customer Success 101: CSM Phone Playbook | csmis.org PPTX
Types of microbes in Microbiology ppptx none PPTX
Tycho_Brahe_and_Johannes_Kepler_Editable_PPT.pptx PPTX
Web Designing Course in Chennai – Career Guide, Skills & Placement Support | ... PDF
CI or FS Poly Cleared Job Fair Handbook | February 5, 2026 Hello Digestions and Absorption in GIT.ppt
- 1.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
DIGESTION AND ABSORPTION of
CARBOHYDRATES & PROTEINS
Dr. Shahnawaz Alam
Associate Professor (Physiology)
NMCRC, Kanpur
- 2.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Basis for Digestion - Hydrolysis
• Digestion involves the breakdown or
hydrolysis (addition of water) of nutrients to
smaller molecules that can be absorbed in
small intestine
• Carbohydrates - monosaccharides
• Proteins - small peptides and amino acids
• Fats - 2-monoglycerides and fatty acids
- 3.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Types of Digestion
• Luminal or cavital digestion -
- occurs in lumen of GI tract
- enzymes from salivary glands, stomach, pancreas
- pancreatic enzymes can do all
• Membrane or contact digestion -
- enzymes on brush border of enterocytes
Intracellular digestion: di and tri-peptides
- 4.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
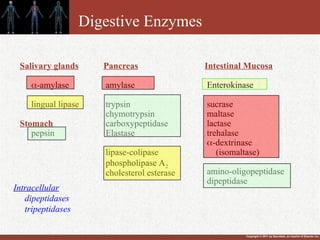
Digestive Enzymes
Salivary glands
-amylase
lingual lipase
Stomach
pepsin
Intestinal Mucosa
Enterokinase
sucrase
maltase
lactase
trehalase
-dextrinase
(isomaltase)
amino-oligopeptidase
dipeptidase
Pancreas
amylase
trypsin
chymotrypsin
carboxypeptidase
Elastase
lipase-colipase
phospholipase A2
cholesterol esterase
Intracellular
dipeptidases
tripeptidases
- 5.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
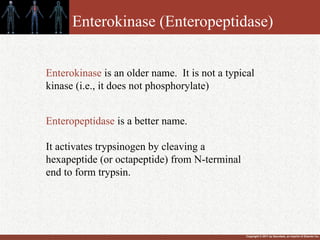
Enterokinase (Enteropeptidase)
Enteropeptidase is a better name.
It activates trypsinogen by cleaving a
hexapeptide (or octapeptide) from N-terminal
end to form trypsin.
Enterokinase is an older name. It is not a typical
kinase (i.e., it does not phosphorylate)
- 6.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
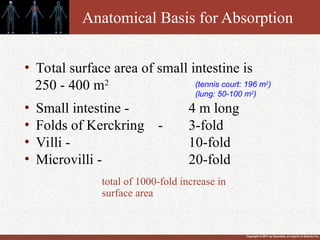
Anatomical Basis for Absorption
• Total surface area of small intestine is
250 - 400 m2
• Small intestine - 4 m long
• Folds of Kerckring - 3-fold
• Villi - 10-fold
• Microvilli - 20-fold
(tennis court: 196 m2
)
(lung: 50-100 m2
)
total of 1000-fold increase in
surface area
- 7.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
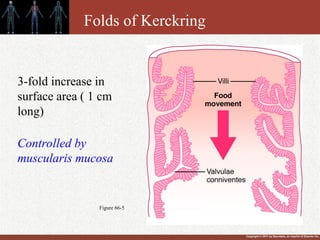
Figure 66-5
Folds of Kerckring
3-fold increase in
surface area ( 1 cm
long)
Controlled by
muscularis mucosa
- 8.
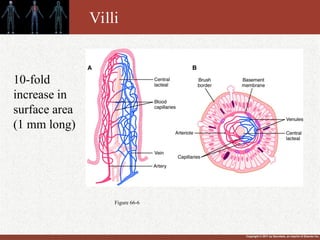
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Figure 66-6
10-fold
increase in
surface area
(1 mm long)
Villi
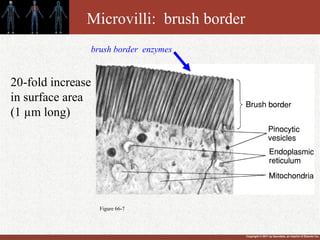
- 9.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Figure 66-7
20-fold increase
in surface area
(1 µm long)
Microvilli: brush border
brush border enzymes
- 10.
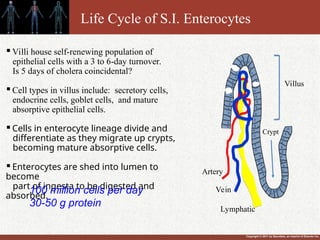
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Villi house self-renewing population of
epithelial cells with a 3 to 6-day turnover.
Is 5 days of cholera coincidental?
Cell types in villus include: secretory cells,
endocrine cells, goblet cells, and mature
absorptive epithelial cells.
Cells in enterocyte lineage divide and
differentiate as they migrate up crypts,
becoming mature absorptive cells.
Enterocytes are shed into lumen to
become
part of ingesta to be digested and
absorbed.
100 million cells per day
30-50 g protein
Life Cycle of S.I. Enterocytes
Artery
Vein
Lymphatic
Villus
Crypt
- 11.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Mechanisms of Absorption
• Four mechanisms are critical for transport of substances
across intestinal cell membrane
- Active Transport -
- primary
- secondary (co-transport, counter-transport)
- Passive Diffusion
- Facilitated Diffusion - carrier mediated
- Endocytosis – this allows large proteins
(immunoglobulins) to be absorbed in babies.
- Does not occur in adults.
- 12.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Sites of Absorption
• Stomach - ethanol, NSAIDs, aspirin
• Duodenum and Jejunum - nutrients, vitamins, various
ions, water and electrolytes
• Ileum - bile salts and vitamin B12
- major clinical significance
• Colon - water and electrolytes
• Rectum - drugs such as steroids and salicylates
- 13.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
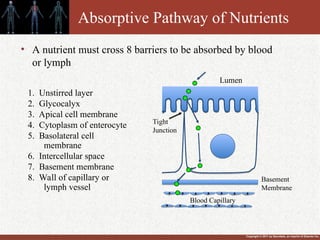
Absorptive Pathway of Nutrients
1. Unstirred layer
2. Glycocalyx
3. Apical cell membrane
4. Cytoplasm of enterocyte
5. Basolateral cell
membrane
6. Intercellular space
7. Basement membrane
8. Wall of capillary or
lymph vessel
• A nutrient must cross 8 barriers to be absorbed by blood
or lymph
Lumen
Tight
Junction
Basement
Membrane
Blood Capillary
- 14.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Digestion
• Carbohydrates
• Proteins
• Fats
- 15.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
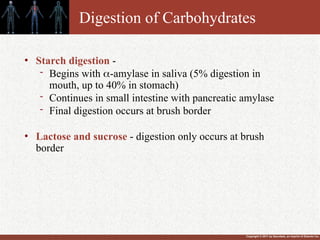
Digestion of Carbohydrates
• Starch digestion -
- Begins with -amylase in saliva (5% digestion in
mouth, up to 40% in stomach)
- Continues in small intestine with pancreatic amylase
- Final digestion occurs at brush border
• Lactose and sucrose - digestion only occurs at brush
border
- 16.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
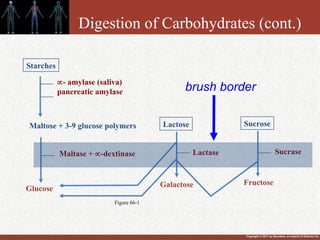
Digestion of Carbohydrates (cont.)
Starches
Maltose + 3-9 glucose polymers
Maltase + -dextinase
Glucose
Galactose
Lactose Sucrose
Lactase
Fructose
Sucrase
- amylase (saliva)
pancreatic amylase brush border
Figure 66-1
- 17.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
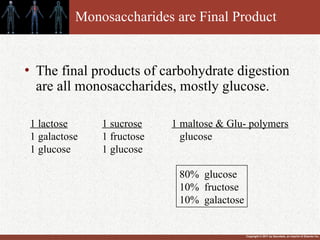
Monosaccharides are Final Product
• The final products of carbohydrate digestion
are all monosaccharides, mostly glucose.
1 lactose
1 galactose
1 glucose
1 sucrose
1 fructose
1 glucose
1 maltose & Glu- polymers
glucose
80% glucose
10% fructose
10% galactose
- 18.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
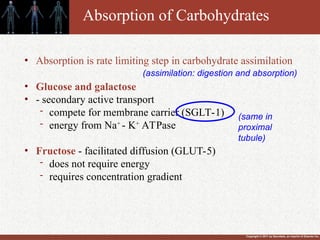
Absorption of Carbohydrates
• Absorption is rate limiting step in carbohydrate assimilation
• Glucose and galactose
• - secondary active transport
- compete for membrane carrier (SGLT-1)
- energy from Na+
- K+
ATPase
• Fructose - facilitated diffusion (GLUT-5)
- does not require energy
- requires concentration gradient
(same in
proximal
tubule)
(assimilation: digestion and absorption)
- 19.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
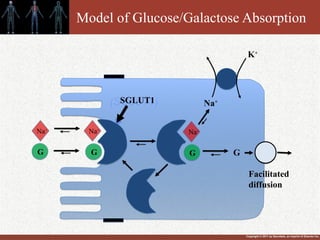
Model of Glucose/Galactose Absorption
(SGLUT1)
Na+
Na+
Na+
G G G
Na+
SGLUT1
K+
G
Facilitated
diffusion
- 20.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
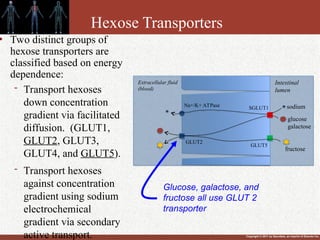
Hexose Transporters
• Two distinct groups of
hexose transporters are
classified based on energy
dependence:
- Transport hexoses
down concentration
gradient via facilitated
diffusion. (GLUT1,
GLUT2, GLUT3,
GLUT4, and GLUT5).
- Transport hexoses
against concentration
gradient using sodium
electrochemical
gradient via secondary
active transport.
Intestinal
lumen
Extracellular fluid
(blood)
SGLUT1
Na+/K+ ATPase
GLUT2
GLUT5
sodium
glucose
galactose
fructose
Glucose, galactose, and
fructose all use GLUT 2
transporter
- 21.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Abnormalities of Carbohydrate
Assimilation
Lactose Intolerance [acquired lactase deficiency or primary adult
hypolactasia] most common
Symptoms - abdominal cramps, bloating, diarrhea, and flatulence
Diagnosis - feed lactose - look for glucose in plasma
- H2 breath test
Cause - absence of brush border lactase
Prevalence: 80% blacks and Hispanics, ~100% Asians, 15-20%
white Europeans
Treatment – avoid milk, drink predigested milk (lactose free milk)
or take calcium supplements
Lack of glucose / galactose carrier - rare
diagnosed at birth
feed fructose
(what if??)
(SGLT-1)
- 22.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
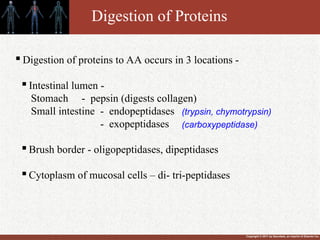
Digestion of Proteins
Digestion of proteins to AA occurs in 3 locations -
Intestinal lumen -
Stomach - pepsin (digests collagen)
Small intestine - endopeptidases
- exopeptidases
Brush border - oligopeptidases, dipeptidases
Cytoplasm of mucosal cells – di- tri-peptidases
(trypsin, chymotrypsin)
(carboxypeptidase)
- 23.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
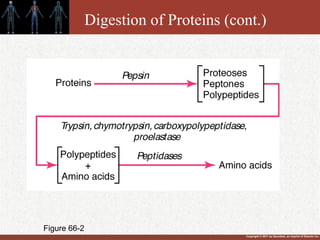
Digestion of Proteins (cont.)
Figure 66-2
- 24.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
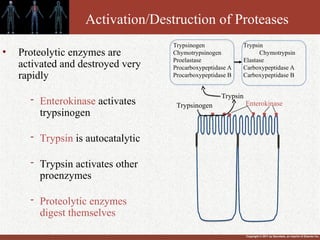
Activation/Destruction of Proteases
• Proteolytic enzymes are
activated and destroyed very
rapidly
- Enterokinase activates
trypsinogen
- Trypsin is autocatalytic
- Trypsin activates other
proenzymes
- Proteolytic enzymes
digest themselves
Enterokinase
Trypsin
Trypsinogen
Trypsinogen Trypsin
Chymotrypsinogen Chymotrypsin
Proelastase Elastase
Procarboxypeptidase A Carboxypeptidase A
Procarboxypeptidase B Carboxypeptidase B
- 25.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
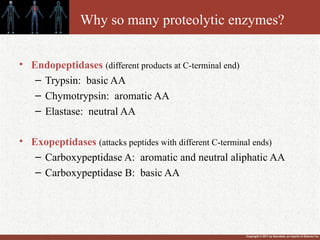
Why so many proteolytic enzymes?
• Endopeptidases (different products at C-terminal end)
– Trypsin: basic AA
– Chymotrypsin: aromatic AA
– Elastase: neutral AA
• Exopeptidases (attacks peptides with different C-terminal ends)
– Carboxypeptidase A: aromatic and neutral aliphatic AA
– Carboxypeptidase B: basic AA
- 26.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
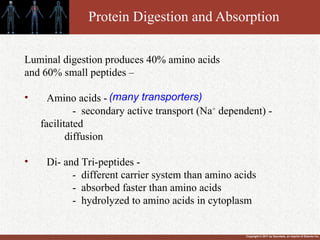
Protein Digestion and Absorption
Luminal digestion produces 40% amino acids
and 60% small peptides –
• Amino acids -
- secondary active transport (Na+
dependent) -
facilitated
diffusion
• Di- and Tri-peptides -
- different carrier system than amino acids
- absorbed faster than amino acids
- hydrolyzed to amino acids in cytoplasm
(many transporters)
- 27.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
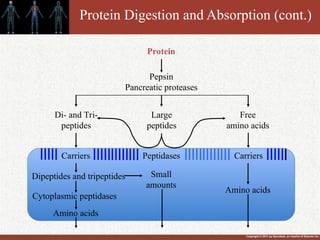
Protein Digestion and Absorption (cont.)
Dipeptides and tripeptides
Cytoplasmic peptidases
Amino acids
Di- and Tri-
peptides
Large
peptides
Free
amino acids
Carriers
Peptidases
Small
amounts
Amino acids
Protein
Pepsin
Pancreatic proteases
Carriers
- 28.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
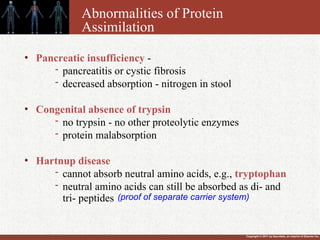
Abnormalities of Protein
Assimilation
• Pancreatic insufficiency -
- pancreatitis or cystic fibrosis
- decreased absorption - nitrogen in stool
• Congenital absence of trypsin
- no trypsin - no other proteolytic enzymes
- protein malabsorption
• Hartnup disease
- cannot absorb neutral amino acids, e.g., tryptophan
- neutral amino acids can still be absorbed as di- and
tri- peptides (proof of separate carrier system)
- 29.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
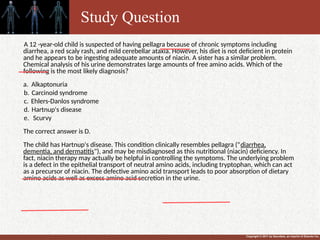
A 12 -year-old child is suspected of having pellagra because of chronic symptoms including
diarrhea, a red scaly rash, and mild cerebellar ataxia. However, his diet is not deficient in protein
and he appears to be ingesting adequate amounts of niacin. A sister has a similar problem.
Chemical analysis of his urine demonstrates large amounts of free amino acids. Which of the
following is the most likely diagnosis?
a. Alkaptonuria
b. Carcinoid syndrome
c. Ehlers-Danlos syndrome
d. Hartnup's disease
e. Scurvy
The correct answer is D.
The child has Hartnup's disease. This condition clinically resembles pellagra ("diarrhea,
dementia, and dermatitis"), and may be misdiagnosed as this nutritional (niacin) deficiency. In
fact, niacin therapy may actually be helpful in controlling the symptoms. The underlying problem
is a defect in the epithelial transport of neutral amino acids, including tryptophan, which can act
as a precursor of niacin. The defective amino acid transport leads to poor absorption of dietary
amino acids as well as excess amino acid secretion in the urine.
Study Question
- 30.
- 31.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
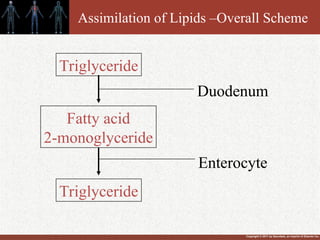
Assimilation of Lipids –Overall Scheme
Triglyceride
Fatty acid
2-monoglyceride
Triglyceride
Duodenum
Enterocyte
- 32.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
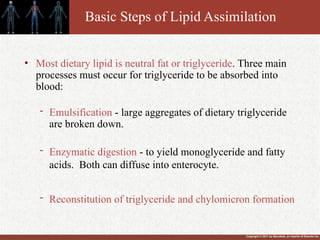
Basic Steps of Lipid Assimilation
• Most dietary lipid is neutral fat or triglyceride. Three main
processes must occur for triglyceride to be absorbed into
blood:
- Emulsification - large aggregates of dietary triglyceride
are broken down.
- Enzymatic digestion - to yield monoglyceride and fatty
acids. Both can diffuse into enterocyte.
- Reconstitution of triglyceride and chylomicron formation
- 33.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
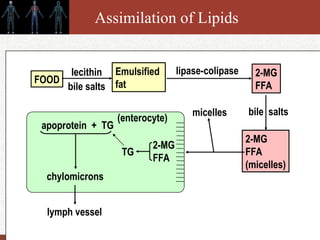
Assimilation of Lipids
Emulsified
fat
2-MG
FFA
FOOD
lecithin
bile salts
lipase-colipase
2-MG
FFA
(micelles)
bile salts
micelles
2-MG
FFA
TG
(enterocyte)
apoprotein + TG
chylomicrons
lymph vessel
- 34.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
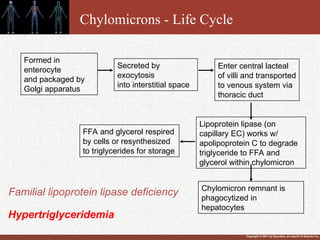
Chylomicrons - Life Cycle
Formed in
enterocyte
and packaged by
Golgi apparatus
Enter central lacteal
of villi and transported
to venous system via
thoracic duct
Secreted by
exocytosis
into interstitial space
Lipoprotein lipase (on
capillary EC) works w/
apolipoprotein C to degrade
triglyceride to FFA and
glycerol within chylomicron
FFA and glycerol respired
by cells or resynthesized
to triglycerides for storage
Chylomicron remnant is
phagocytized in
hepatocytes
Familial lipoprotein lipase deficiency
Hypertriglyceridemia
- 35.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Familial lipoprotein lipase deficiency
Familial lipoprotein lipase deficiency is a
rare genetic disorder characterized by
deficient activity of (lipoprotein lipase) that
breaks down fat molecules, causing the
accumulation of large quantities of fat
(lipoproteins) in the blood.
- 36.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
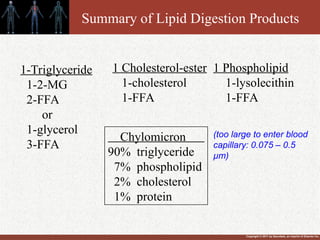
Summary of Lipid Digestion Products
1-Triglyceride
1-2-MG
2-FFA
or
1-glycerol
3-FFA
1 Cholesterol-ester
1-cholesterol
1-FFA
1 Phospholipid
1-lysolecithin
1-FFA
Chylomicron
90% triglyceride
7% phospholipid
2% cholesterol
1% protein
(too large to enter blood
capillary: 0.075 – 0.5
µm)
- 37.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
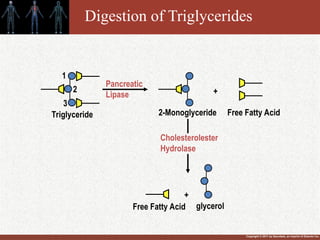
Digestion of Triglycerides
1
2
3
Pancreatic
Lipase
Triglyceride 2-Monoglyceride Free Fatty Acid
+
Free Fatty Acid
+
glycerol
Cholesterolester
Hydrolase
- 38.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
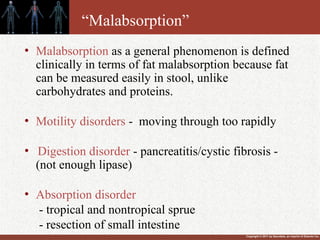
“Malabsorption”
• Malabsorption as a general phenomenon is defined
clinically in terms of fat malabsorption because fat
can be measured easily in stool, unlike
carbohydrates and proteins.
• Motility disorders - moving through too rapidly
• Digestion disorder - pancreatitis/cystic fibrosis -
(not enough lipase)
• Absorption disorder
- tropical and nontropical sprue
- resection of small intestine
- 39.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
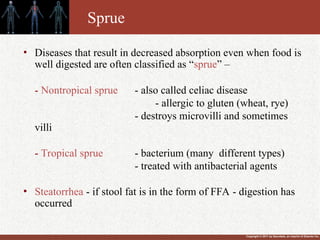
Sprue
• Diseases that result in decreased absorption even when food is
well digested are often classified as “sprue” –
- Nontropical sprue - also called celiac disease
- allergic to gluten (wheat, rye)
- destroys microvilli and sometimes
villi
- Tropical sprue - bacterium (many different types)
- treated with antibacterial agents
• Steatorrhea - if stool fat is in the form of FFA - digestion has
occurred
- 40.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
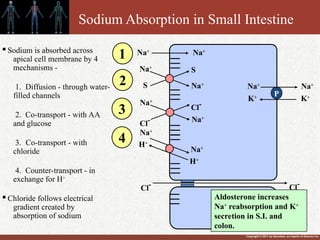
Sodium Absorption in Small Intestine
Na+
Na+
Na+
S
S
Na+
Na+
Cl-
Na+
Cl-
Na+
H+
Na+
H+
P
Na+
Na+
K+
K+
Cl-
Cl-
1
2
3
4
Aldosterone increases
Na+
reabsorption and K+
secretion in S.I. and
colon.
Sodium is absorbed across
apical cell membrane by 4
mechanisms -
1. Diffusion - through water-
filled channels
2. Co-transport - with AA
and glucose
3. Co-transport - with
chloride
4. Counter-transport - in
exchange for H+
Chloride follows electrical
gradient created by
absorption of sodium
- 41.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
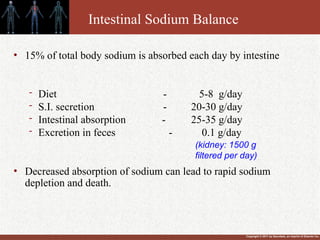
Intestinal Sodium Balance
• 15% of total body sodium is absorbed each day by intestine
- Diet - 5-8 g/day
- S.I. secretion - 20-30 g/day
- Intestinal absorption - 25-35 g/day
- Excretion in feces - 0.1 g/day
• Decreased absorption of sodium can lead to rapid sodium
depletion and death.
(kidney: 1500 g
filtered per day)
- 42.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
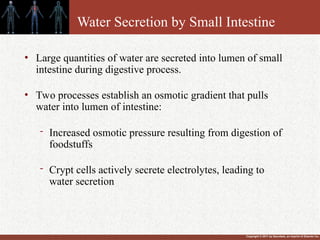
Water Secretion by Small Intestine
• Large quantities of water are secreted into lumen of small
intestine during digestive process.
• Two processes establish an osmotic gradient that pulls
water into lumen of intestine:
- Increased osmotic pressure resulting from digestion of
foodstuffs
- Crypt cells actively secrete electrolytes, leading to
water secretion
- 43.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
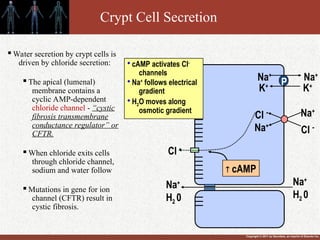
Crypt Cell Secretion
Cl -
Na+
Cl - Na+
P
Na+
Na+
K+
K+
Na+
H2 0
Na+
H2 0
Cl -
cAMP
cAMP activates Cl-
channels
Na+
follows electrical
gradient
H2O moves along
osmotic gradient
Water secretion by crypt cells is
driven by chloride secretion:
The apical (lumenal)
membrane contains a
cyclic AMP-dependent
chloride channel - “cystic
fibrosis transmembrane
conductance regulator” or
CFTR.
When chloride exits cells
through chloride channel,
sodium and water follow
Mutations in gene for ion
channel (CFTR) result in
cystic fibrosis.
- 44.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Diarrhea
• Diarrhea is the third leading cause of death by disease
worldwide
- 5-8 million children per year worldwide
- 250,000 hospital visits in US
- 8 million office visits in US
- 45.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
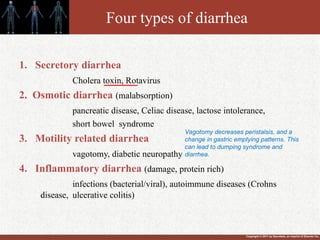
Four types of diarrhea
1. Secretory diarrhea
Cholera toxin, Rotavirus
2. Osmotic diarrhea (malabsorption)
pancreatic disease, Celiac disease, lactose intolerance,
short bowel syndrome
3. Motility related diarrhea
vagotomy, diabetic neuropathy
4. Inflammatory diarrhea (damage, protein rich)
infections (bacterial/viral), autoimmune diseases (Crohns
disease, ulcerative colitis)
Vagotomy decreases peristalsis, and a
change in gastric emptying patterns. This
can lead to dumping syndrome and
diarrhea.
- 46.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Rotavirus
By the age of five, nearly every child in
the world has
been infected with rotavirus at least once.
More than 500,000 children under five
years of age die from rotavirus infection
each year
Malabsorption occurs because enterocytes
are damaged: SGLT1 transporter is
disrupted and brush border disaccharidase
activity is reduced (increases osmotic
load)
ENS secretory reflexes are activated
Lactose intolerance can last for weeks
- 47.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
Cholera (Vibrio cholerae)
Cause
- cholera toxin stimulates secretion of
water and electrolytes from crypt cells
- lose 10 L or more fluid per day
Prognosis
- untreated, 50% will die
- treated, <1% will die
Treatment
- Antiobiotics: children, furazolidone.
adults, erythromycin, tetracycline.
- oral rehydration solutions (glucose
and
electrolytes)
- glucose facilitated absorption of
sodium
and water remains intact
- 48.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
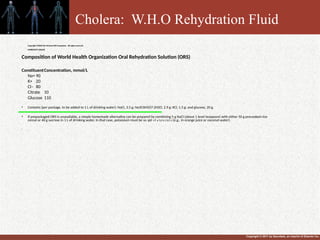
•
.
Copyright ©2006 The McGraw-Hill Companies. All rights reserved.
HARRISON'S ONLINE
Composition of World Health Organization Oral Rehydration Solution (ORS)
ConstituentConcentration, mmol/L
Na+ 90
K+ 20
Cl– 80
Citrate 10
Glucose 110
• Contains (per package, to be added to 1 L of drinking water): NaCl, 3.5 g; Na3C6H5O7·2H2O, 2.9 g; KCl, 1.5 g; and glucose, 20 g.
• If prepackaged ORS is unavailable, a simple homemade alternative can be prepared by combining 5 g NaCl (about 1 level teaspoon) with either 50 g precooked rice
cereal or 40 g sucrose in 1 L of drinking water. In that case, potassium must be supplied separately (e.g., in orange juice or coconut water).
•
Cholera
Cholera: W.H.O Rehydration Fluid
- 49.
Copyright © 2011by Saunders, an imprint of Elsevier Inc.
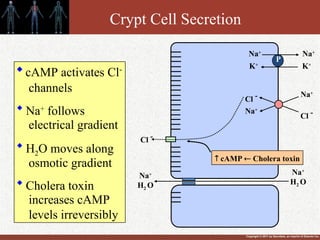
Crypt Cell Secretion
Cl -
Na+
Cl - Na+
P
Na+
Na+
K+
K+
Na+
H2 O
Na+
H2 O
Cl -
cAMP Cholera toxin
cAMP activates Cl-
channels
Na+
follows
electrical gradient
H2O moves along
osmotic gradient
Cholera toxin
increases cAMP
levels irreversibly
- 50.
![Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Abnormalities of Carbohydrate
Assimilation
Lactose Intolerance [acquired lactase deficiency or primary adult
hypolactasia] most common
Symptoms - abdominal cramps, bloating, diarrhea, and flatulence
Diagnosis - feed lactose - look for glucose in plasma
- H2 breath test
Cause - absence of brush border lactase
Prevalence: 80% blacks and Hispanics, ~100% Asians, 15-20%
white Europeans
Treatment – avoid milk, drink predigested milk (lactose free milk)
or take calcium supplements
Lack of glucose / galactose carrier - rare
diagnosed at birth
feed fructose
(what if??)
(SGLT-1)](https://image.slidesharecdn.com/digestionsandabsorptioningit-260121054652-55eaba6a/85/Hello-Digestions-and-Absorption-in-GIT-ppt-21-320.jpg)