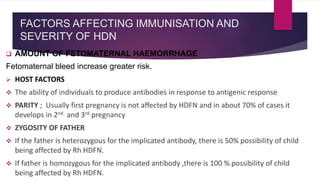
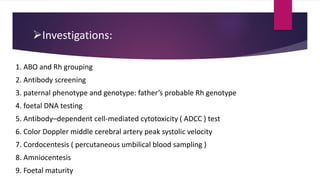
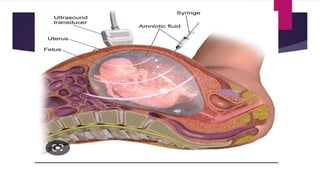
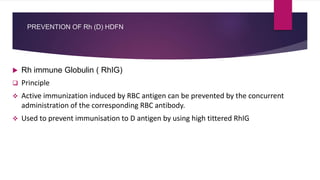
This document provides a comprehensive overview of Hemolytic Disease of the Fetus and Newborn (HDFN), which is primarily caused by Rh incompatibility between an Rh-negative mother and an Rh-positive fetus. The text discusses the etiology, pathophysiology, diagnosis, and management of HDFN, including preventive measures like Rh immune globulin (RhIg) administration. It emphasizes the serious consequences on both the fetus and newborn, like anemia and hyperbilirubinemia, and outlines the various classifications and diagnostic approaches necessary for effective care.