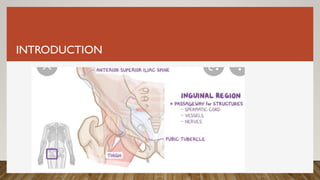
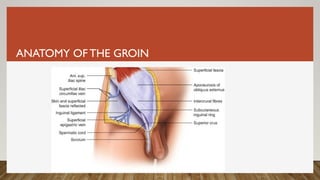
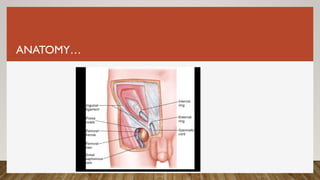
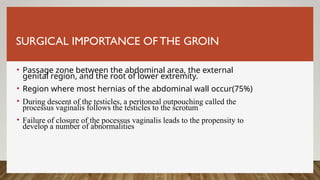
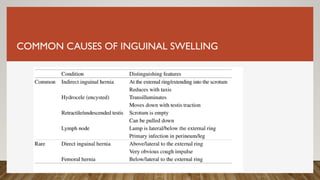
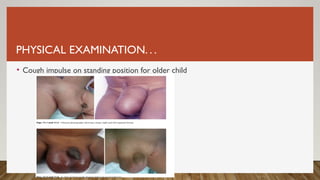
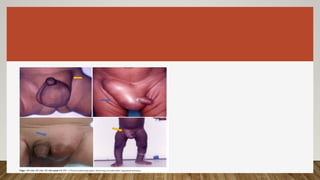
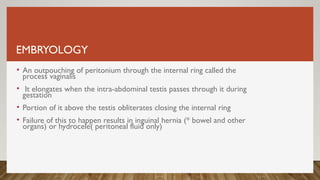
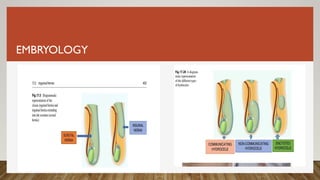
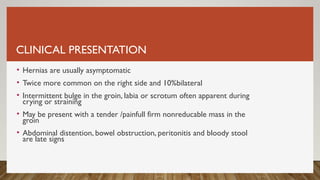
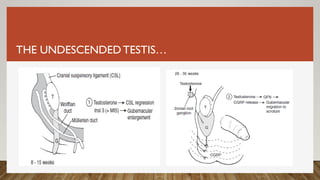
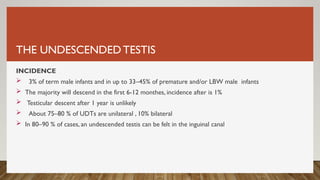
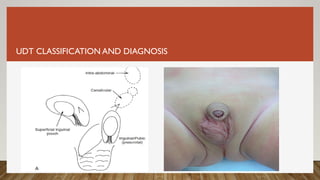
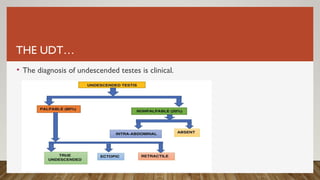
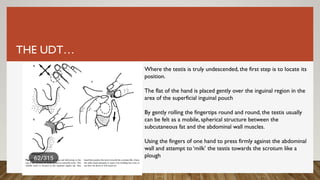
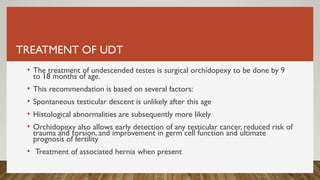
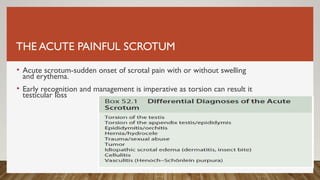
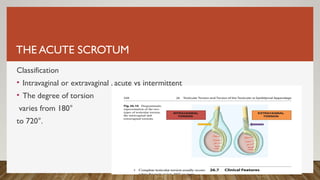
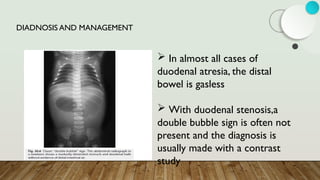
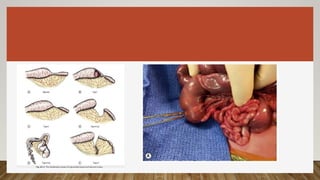
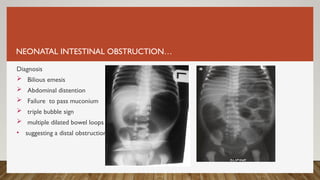
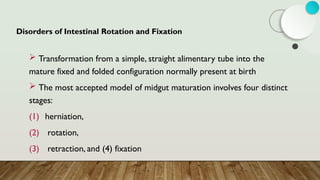
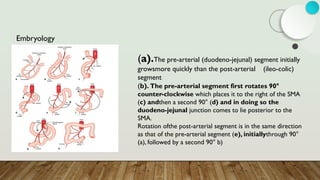
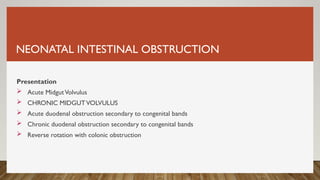
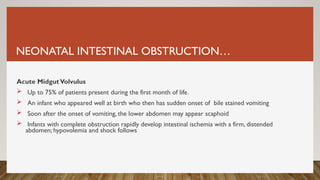
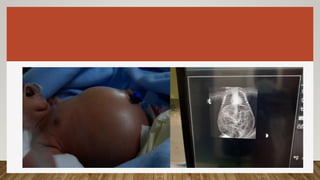
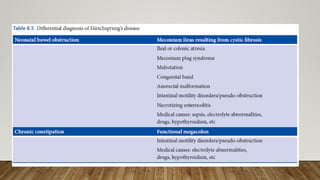
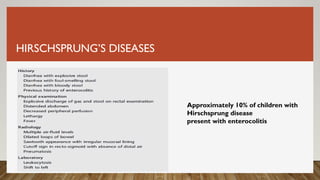
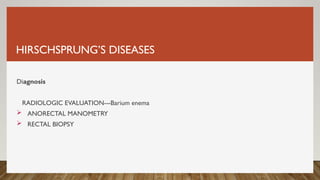
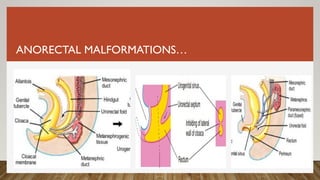
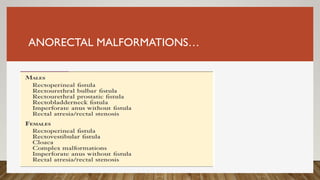
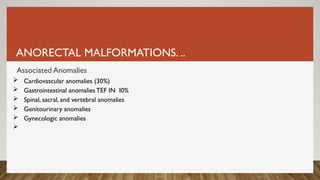
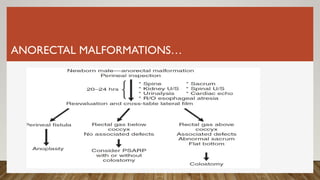
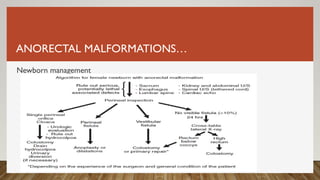
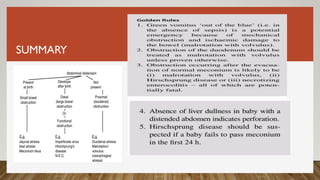
The document covers pediatric surgical topics including groin lumps in children, management of inguinal hernias and hydroceles, undescended testis, and neonatal intestinal obstruction. Key conditions such as testicular torsion, Hirschsprung's disease, and anorectal malformations are discussed along with their clinical presentations, diagnosis, and surgical management. Emphasis is placed on the importance of timely identification and intervention in these surgical emergencies.