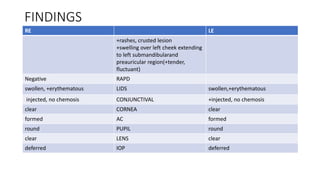
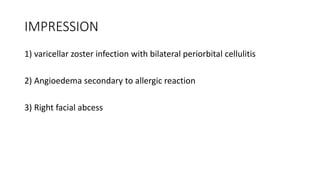
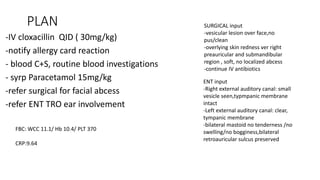
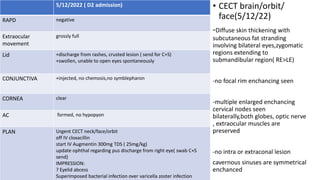
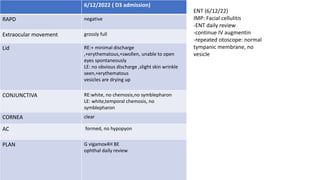
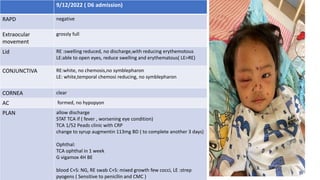
1. Case 1 involves a 1 year old female with varicella zoster infection and bilateral periorbital cellulitis following a reaction to acyclovir. She developed facial swelling and was treated with IV antibiotics.
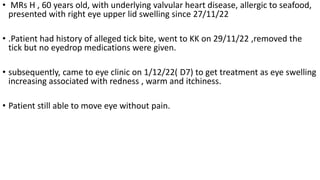
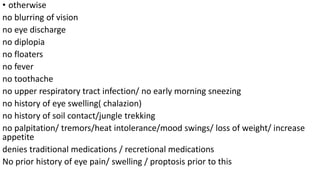
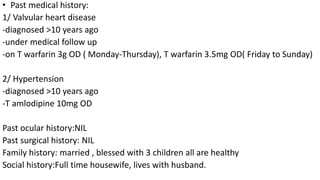
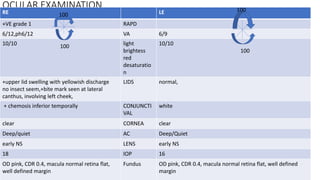
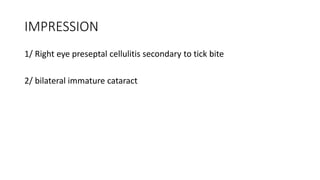
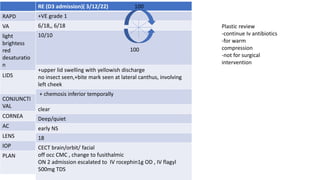
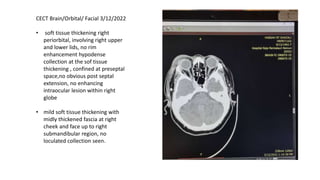
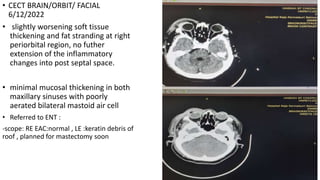
2. Case 2 is a 60 year old female with a history of valvular heart disease who presented with right eye swelling following an alleged tick bite. She was diagnosed with right eye preseptal cellulitis secondary to the tick bite and treated with IV antibiotics.
3. Both cases involved bacterial superinfection of existing conditions (varicella zoster infection and tick bite) leading to periorbital or preseptal cellulitis. They were treated with