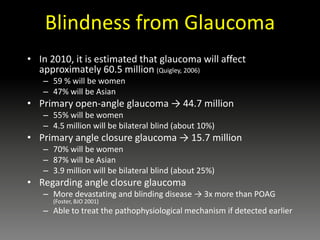
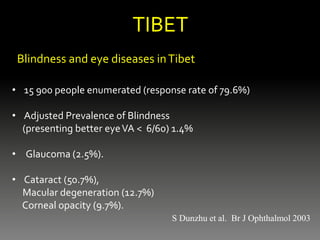
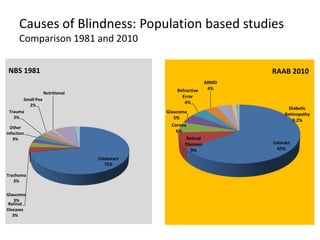
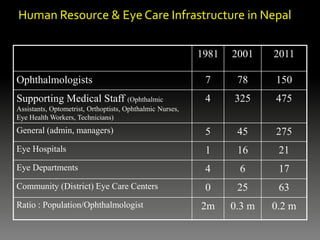
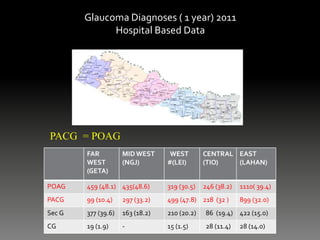
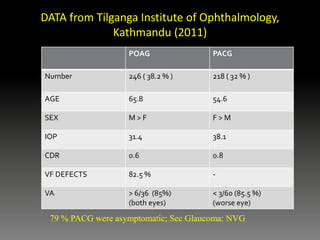
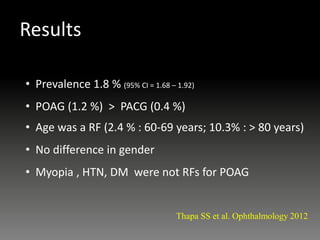
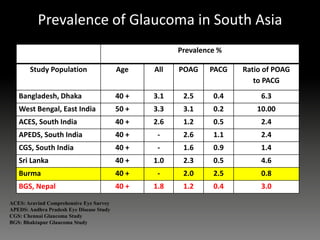
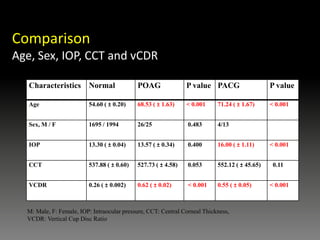
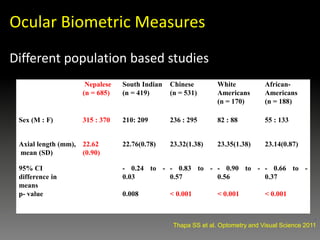
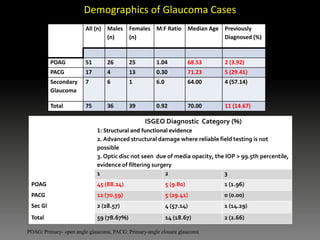
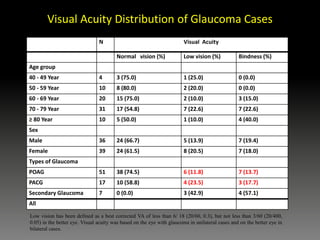
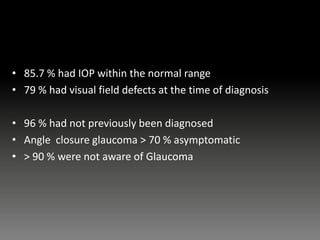
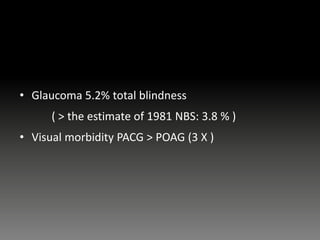
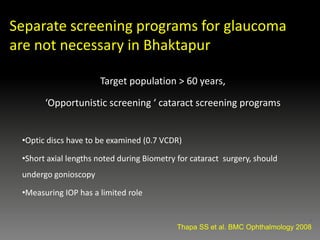
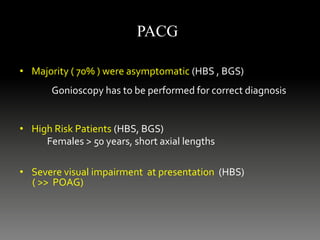
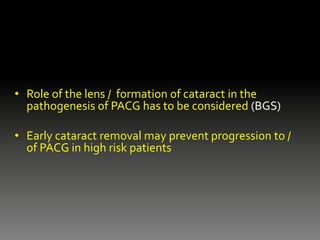
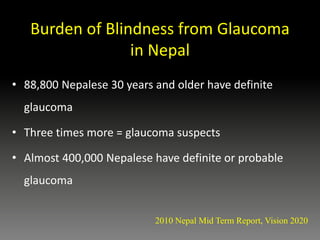
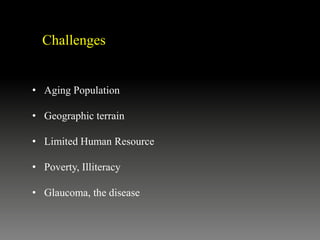
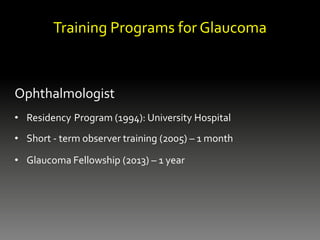
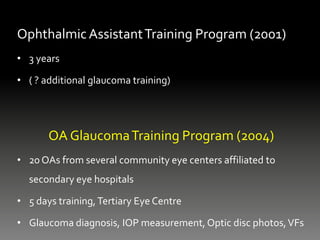
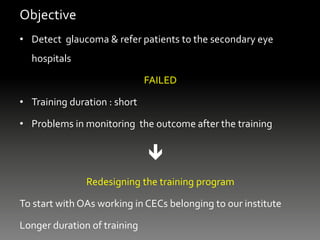
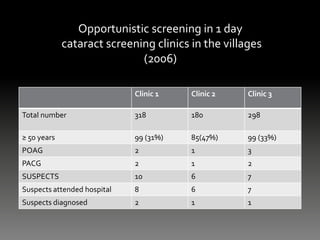
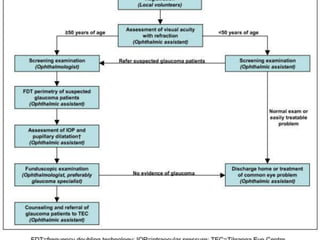
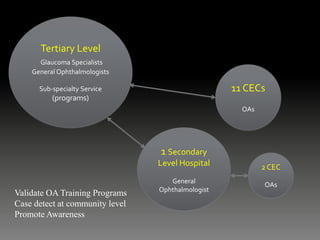
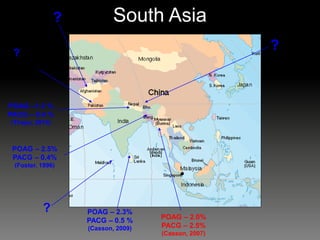
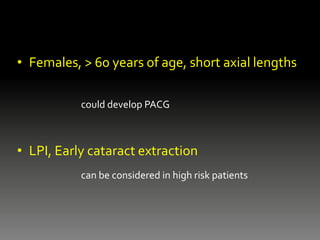
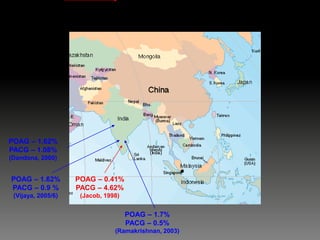
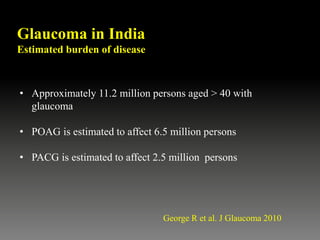
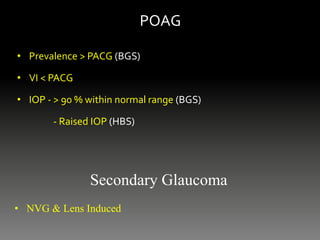
Glaucoma poses significant challenges for care in the Himalayan regions of Tibet and Nepal. It is a leading cause of irreversible blindness. Hospital data from Nepal shows primary angle-closure glaucoma is more common and causes greater visual impairment than primary open-angle glaucoma. Population studies estimate glaucoma accounts for 5% of blindness, higher than previously thought. Most cases are asymptomatic and diagnosed late with severe vision loss. Strategies to address challenges include training programs to expand the eye care workforce and opportunistic screening to enhance case detection.