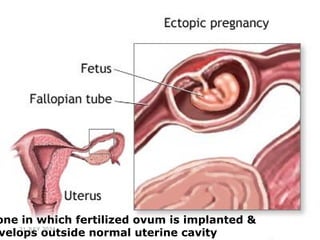
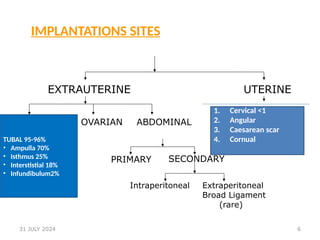
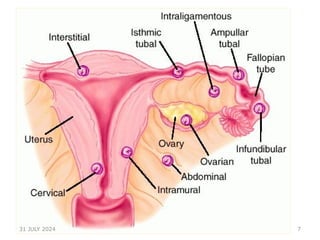
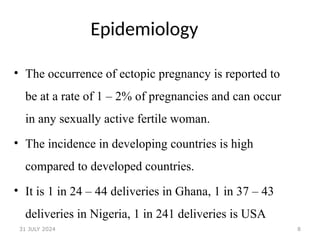
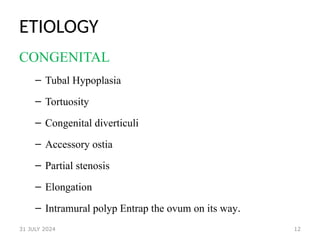
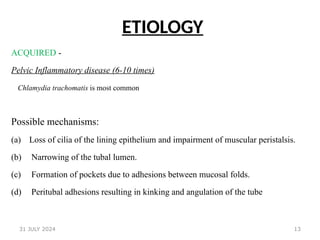
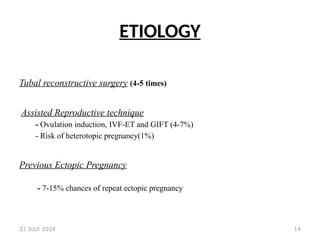
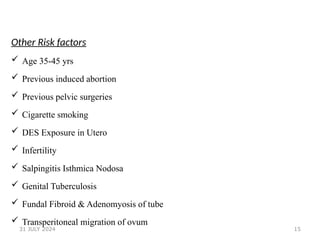
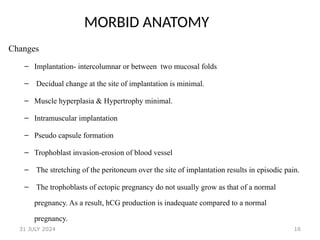
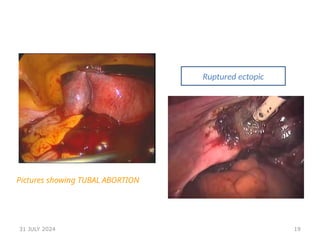
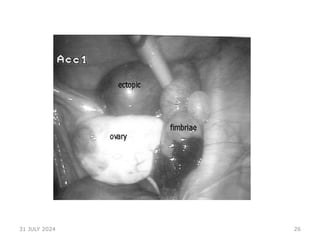
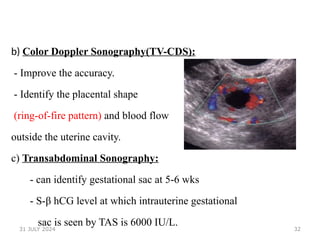
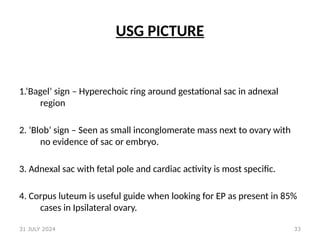
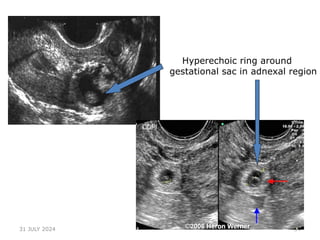
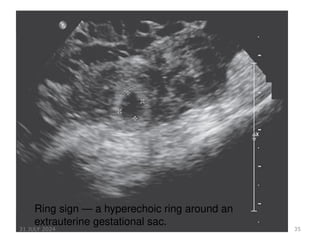
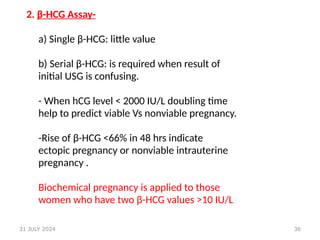
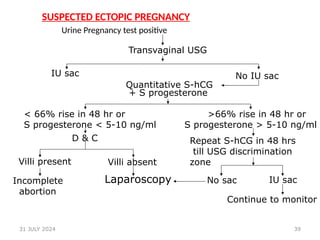
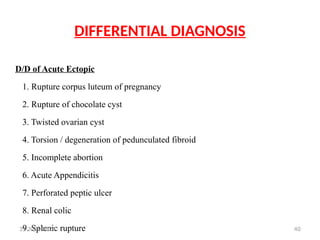
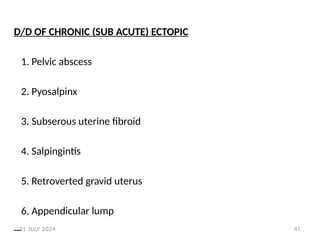
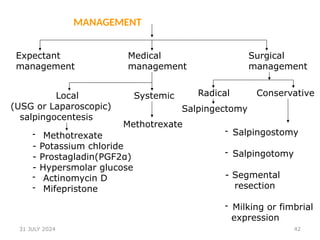
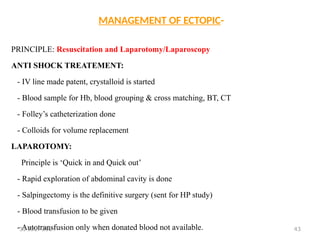
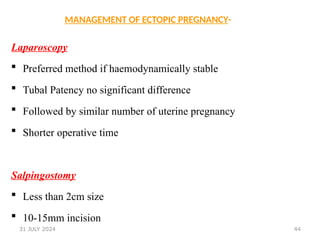
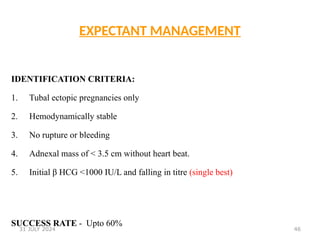
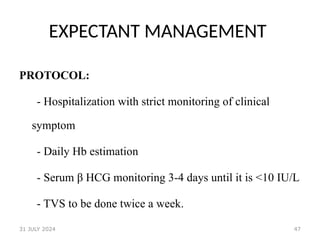
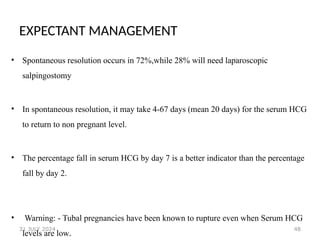
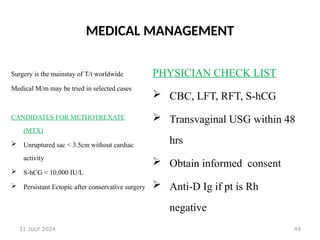
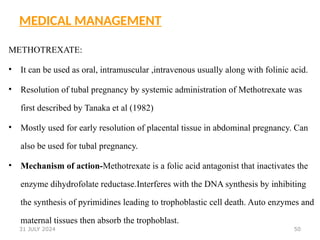
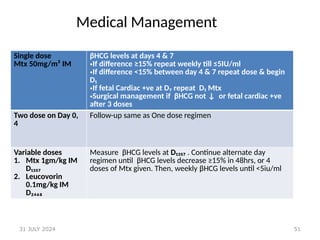
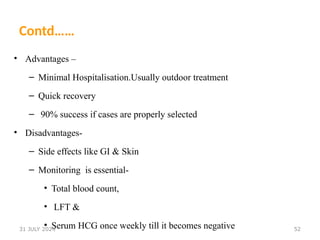
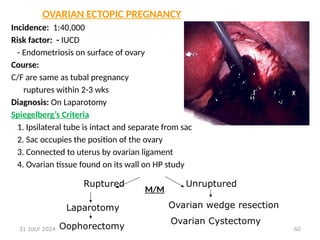
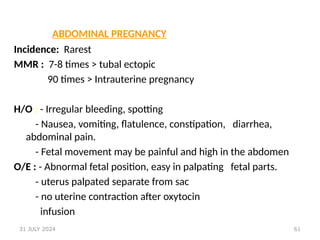
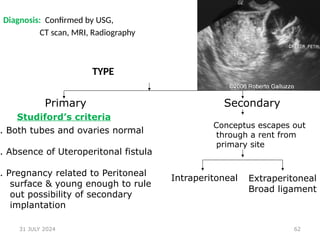
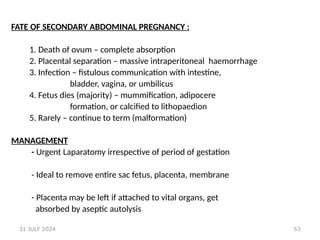
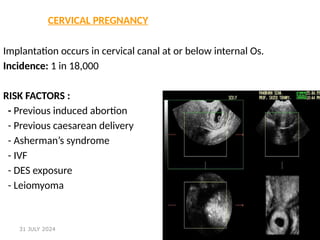
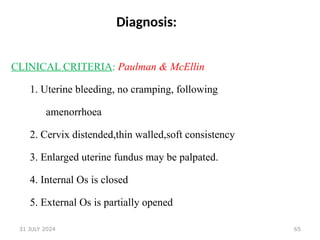
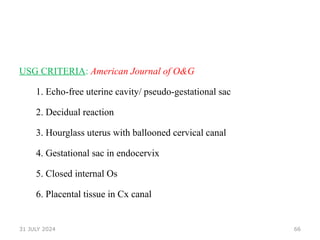
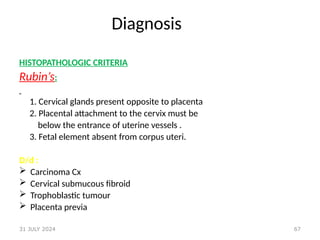
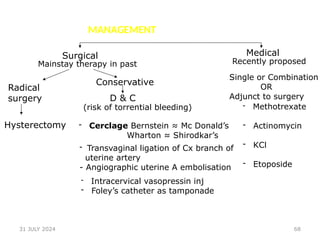
The document is a tutorial presentation on ectopic pregnancy, including its definition, epidemiology, etiology, clinical approaches, diagnosis, differential diagnoses, and management strategies. Ectopic pregnancy is described as a significant public health issue in sub-Saharan Africa, posing serious risks to women's health and reproductive potential. The presentation emphasizes the importance of early recognition and intervention to reduce morbidity and mortality associated with ectopic pregnancies.