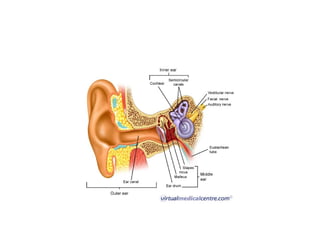
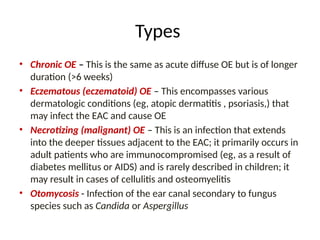
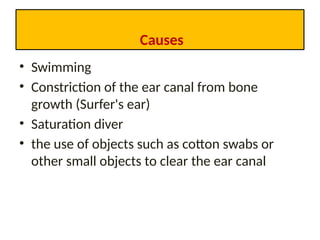
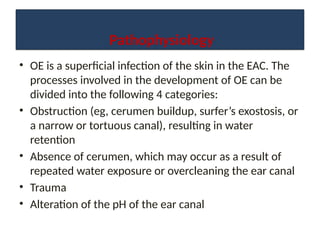
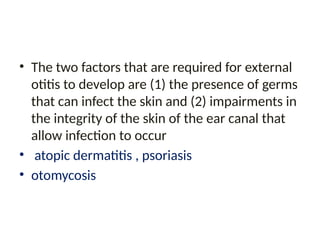
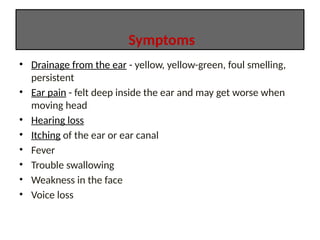
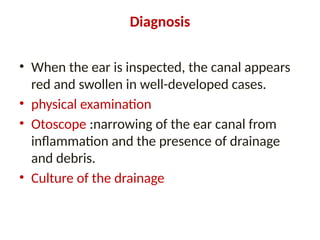
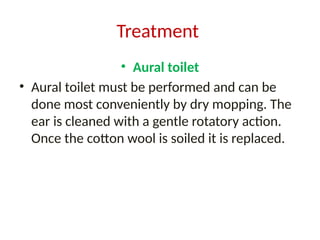
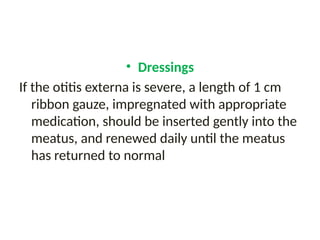
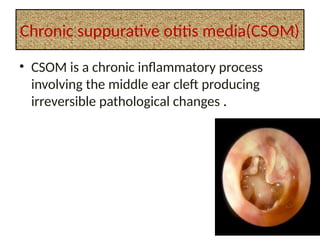
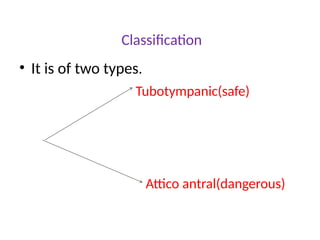
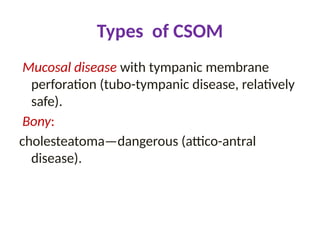
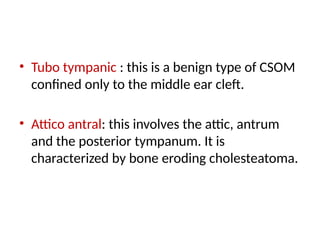
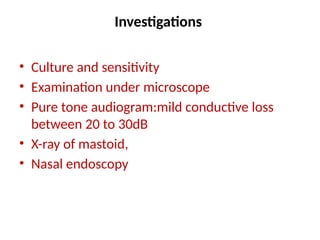
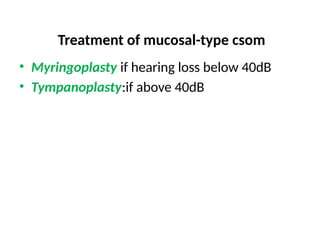
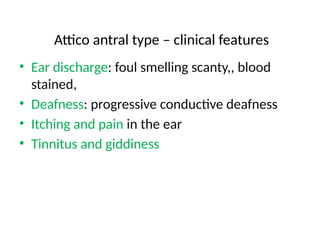
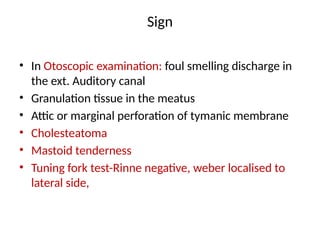
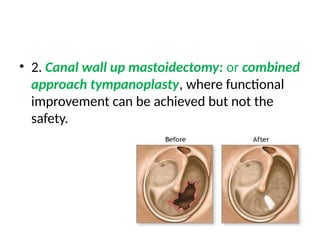
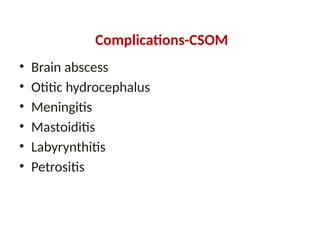
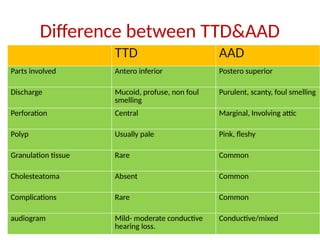
The document provides a comprehensive overview of ear disorders, detailing the anatomy of the ear and common conditions such as otitis externa and otitis media. It outlines the symptoms, diagnostic methods, and treatment options for various types of ear infections, including prevention strategies and the underlying causes of these conditions. Additionally, it differentiates between chronic suppurative otitis media types and highlights potential complications associated with untreated ear infections.