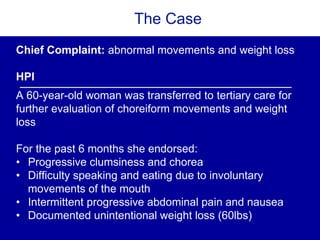
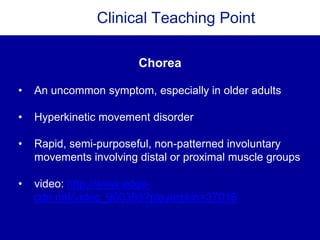
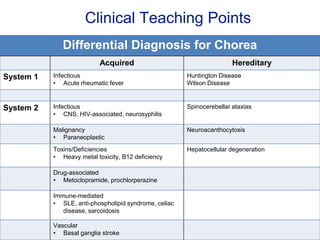
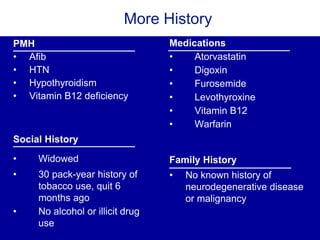
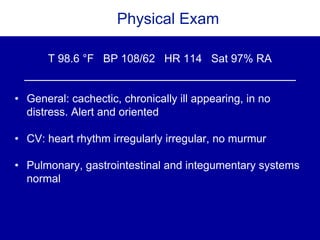
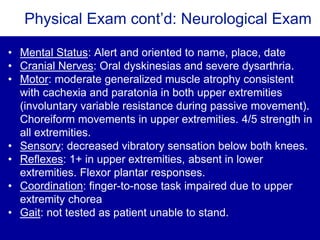
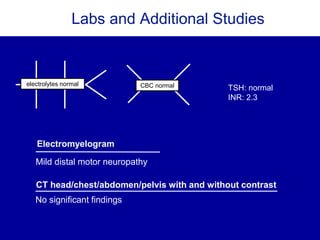
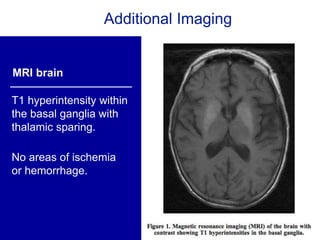
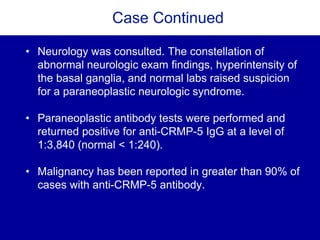
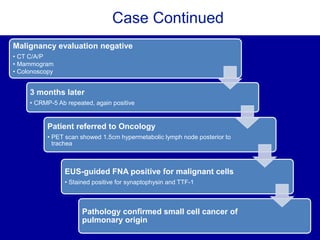
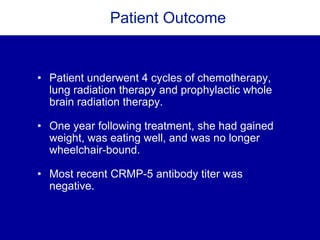
This case describes a 60-year-old woman presenting with choreiform movements, weight loss, and dysarthria over the past 6 months. Imaging showed T1 hyperintensity in the basal ganglia. She tested positive for anti-CRMP-5 antibodies, which are associated with malignancy in over 90% of cases. Further workup revealed a small cell lung cancer. Her symptoms improved with cancer treatment and decreasing antibody levels, indicating this was a paraneoplastic neurological syndrome.