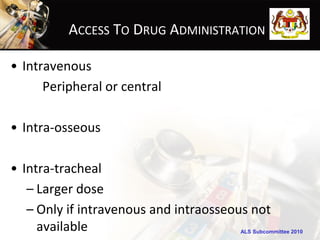
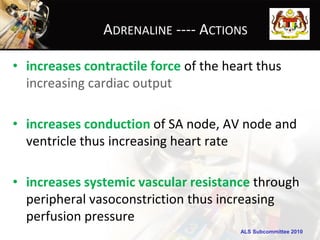
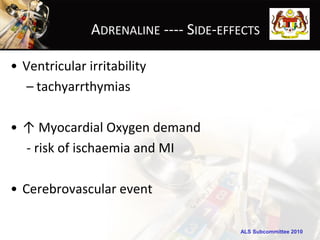
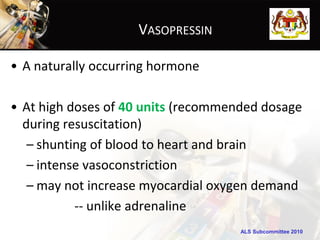
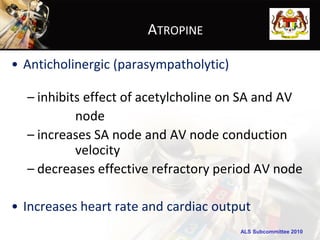
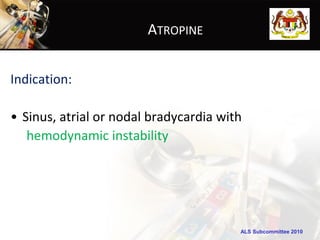
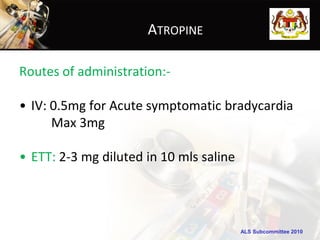
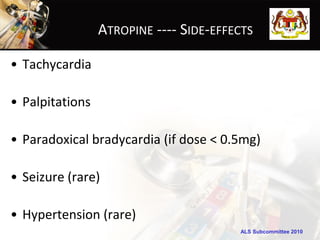
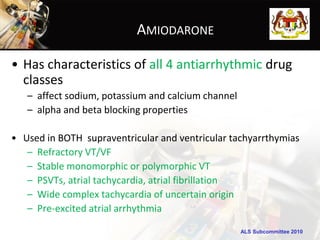
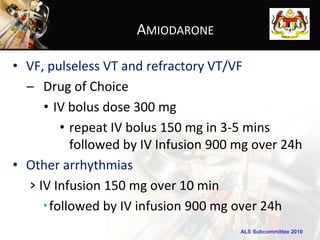
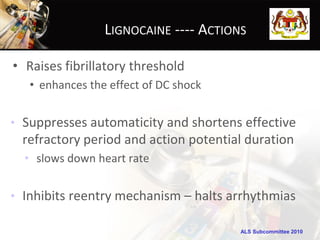
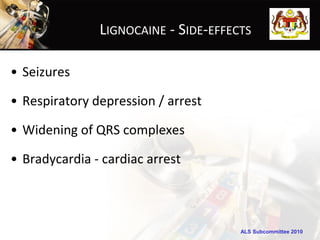
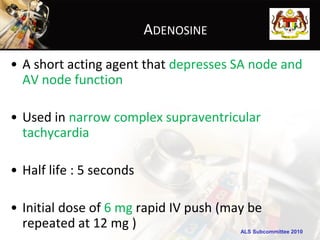
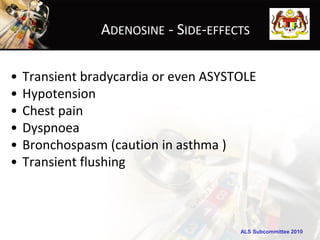
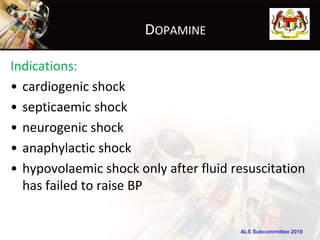
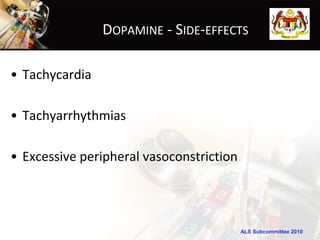
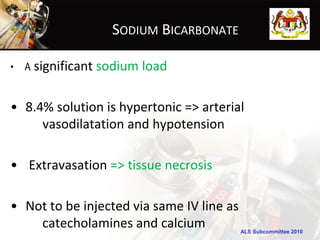
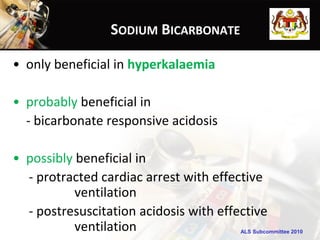
This document discusses drugs commonly used in cardiopulmonary resuscitation. It outlines several drugs including adrenaline, vasopressin, atropine, amiodarone, lignocaine, adenosine, and dopamine. For each drug, it describes the major indications, routes of administration, actions, and potential side effects. The objectives are to be able to state the commonly used resuscitation drugs, outline their major actions, and list two side effects for each.