This document is a doctoral thesis that examines total wrist arthroplasty (TWA), patient-rated outcome measures related to TWA, and periprosthetic osteolysis following TWA. The thesis includes studies using a multicenter international registry of TWA patients, radiographical and histopathological evaluations, and validation of translated patient-rated outcome measures. The overall aim is to evaluate outcomes of TWA, assess patient-rated outcomes, and investigate periprosthetic osteolysis.










![13
List
of
papers
I. Boeckstyns
MEH.
Wrist
arthroplasty
−
a
systematic
review.
Dan
Med
J
2014;61(5):A4834
11.
II. Herzberg
G,
Boeckstyns
M,
Sorensen
AI,
Axelsson
P,
Kroener
K,
Liverneaux
P,
et
al.
"Remotion"
total
wrist
arthroplasty:
preliminary
results
of
a
prospective
international
multicenter
study
of
215
cases.
J
Wrist
Surg.
2012
Aug;1(1):
17-‐22.
12
III. Boeckstyns
ME,
Herzberg
G,
Sorensen
AI,
Axelsson
P,
Kroner
K,
Liverneaux
PA,
et
al.
Can
total
wrist
arthroplasty
be
an
option
in
the
treatment
of
the
severely
destroyed
posttraumatic
wrist?
J
Wrist
Surg.
2013
Nov;2(4):
324-‐9.
13
IV. Boeckstyns
ME,
Herzberg
G,
Merser
S.
Favorable
results
after
total
wrist
arthroplasty:
65
wrists
in
60
patients
followed
for
5-‐9
years.
Acta
orthopaedica.
2013
Aug;84(4):
415-‐9.
14
V. Boeckstyns
MEH,
Herzberg
G:
Periprosthetic osteolysis after total wrist
arthroplasty. J Wrist Surg 2014;3:101–106 15
.
VI. Boeckstyns
MEH,
Toxværd
A,
Bansal
M,
Vadstrup
LS.
Wear
particles
and
osteolysis
in
patients
with
total
wrist
arthroplasty.
J
Hand
Surg
Am
2014;
39(12):2396-‐2404
16
.
VII. Herup
A,
Merser
S,
Boeckstyns
M.
[Validation
of
questionnaire
for
conditions
of
the
upper
extremity].
Ugeskr
laeger
2010;172(48):
3333-‐6.
17
VIII. Boeckstyns
MEH,
Merser
S:
Psychometric Properties of two Questionnaires in the
Context of Total Wrist Arthroplasty.
Dan
Med
J
2014;
61
(11):
A4939
18.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-13-320.jpg)


























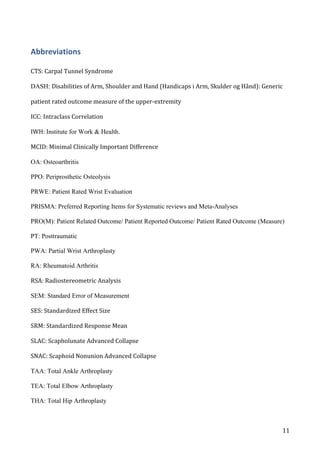
![47
Figure
11:
correlation
between
DASH-‐scores
in
a
test-‐retest
trial
on
54
patients
with
a
stable
upper-‐extremity
condition.
X-‐axis
=
scores
at
first
test,
y-‐axis
=
scores
at
retest
14-‐30
days
later.
ICC
=
0.85,
Spearman’s
rho
=
0.90.
(figure
1
in
Herup
A,
Merser
S,
Boeckstyns
M.
[Validation
of
questionnaire
for
conditions
of
the
upper
extremity].
Ugeskr
laeger
2010;172(48):
3333-‐6
(Paper
VII)).
As
the
DASH-‐questionnaire
is
increasingly
replaced
by
the
QuickDASH,
we
decided
to
assess
the
psychometric
properties
of
the
Danish
QuickDASH
and
another
widely
used
PROM
for
wrist
conditions
–
the
PRWE
-‐
in
patients
with
total
wrist
arthroplasty
(paper
VIII)
18.
In
a
prospective
cohort
of
102
cases,
we
evaluated
the
QuickDASH.
In
a
cross-‐sectional
study
and
in
a
test-‐retest
on
a
subgroup
of
the
patients
we
evaluated
both
the
QuickDASH
and
the
PRWE.
Internal
consistency
and
reproducibility
were
very
high
(Cronbach’s
alpha
0.96
/](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-47-320.jpg)





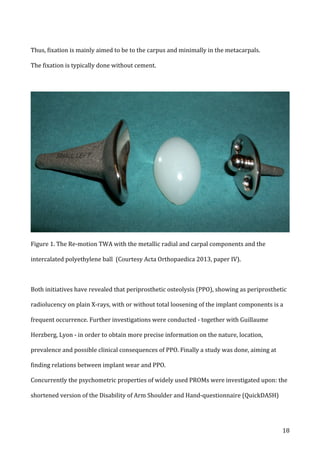
![54
component.
The
authors
stated
that
there
was
polyethylene
wear
and
metallosis
in
all
these
cases
38.
Similar
osteolysis
has
been
reported
using
metal-‐on-‐metal
implants
as
well.
Radmer
et
al.
reviewed
APH-‐implants
that
are
Titanium-‐coated
at
the
articular
surfaces,
without
intercalated
polyethylene
39.
Reigstad
et
al.
reported
focal
osteolysis
in
the
radius
around
a
metal-‐on-‐metal
implant
in
three
patients
without
affecting
the
clinical
outcome,
the
largest
including
most
of
the
radial
styloid,
which
stabilized
after
one
year
62
(figure
13).
Figure
13:
PPO
3
years
after
Motec
metal-‐on-‐metal
TWA
(Reigstad
O,
Lütken
T,
Grimsgaard
C,
et
al.
Promising
one-‐
to
six-‐year
results
with
the
Motec
wrist
arthroplasty
in
patients
with
post-‐traumatic
osteoarthritis.
J
Bone
Joint
Surg
[Br]
2012;94-‐B:1540-‐1545.
(Figure
4)62
,
reproduced
with
permission
and
copyright
©
of
the
British
Editorial
Society
of
Bone
and
Joint
Surgery
[citation].)
In
the
study
“Periprosthetic
osteolysis
after
total
wrist
arthroplasty”
(Paper
V),
juxta-‐articular
radiolucency
larger
than
2
mm
was
seen
in
18
of
44
cases
(41
%),
in
11
at
the
radial
side
only,](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-54-320.jpg)















![70
References
1.
Shrout
PE,
Fleiss
JL.
Intraclass
correlations:
uses
in
assessing
rater
reliability.
Psychological
bulletin.
Mar
1979;86(2):420-‐428.
2.
Hudak
PL,
Amadio
PC,
Bombardier
C.
Development
of
an
upper
extremity
outcome
measure:
the
DASH
(disabilities
of
the
arm,
shoulder
and
hand)
[corrected].
The
Upper
Extremity
Collaborative
Group
(UECG).
American
journal
of
industrial
medicine.
Jun
1996;29(6):602-‐608.
3.
Terwee
CB,
Bot
SD,
de
Boer
MR,
et
al.
Quality
criteria
were
proposed
for
measurement
properties
of
health
status
questionnaires.
Journal
of
clinical
epidemiology.
Jan
2007;60(1):34-‐42.
4.
Wamper
KE,
Sierevelt
IN,
Poolman
RW,
Bhandari
M,
Haverkamp
D.
The
Harris
hip
score:
Do
ceiling
effects
limit
its
usefulness
in
orthopedics?
Acta
orthopaedica.
Dec
2010;81(6):703-‐707.
5.
Angst
F,
Goldhahn
J,
Drerup
S,
Flury
M,
Schwyzer
HK,
Simmen
BR.
How
sharp
is
the
short
QuickDASH?
A
refined
content
and
validity
analysis
of
the
short
form
of
the
disabilities
of
the
shoulder,
arm
and
hand
questionnaire
in
the
strata
of
symptoms
and
function
and
specific
joint
conditions.
Quality
of
life
research
:
an
international
journal
of
quality
of
life
aspects
of
treatment,
care
and
rehabilitation.
Oct
2009;18(8):1043-‐
1051.
6.
MacDermid
JC.
Development
of
a
scale
for
patient
rating
of
wrist
pain
and
disability.
Journal
of
hand
therapy
:
official
journal
of
the
American
Society
of
Hand
Therapists.
Apr-‐Jun
1996;9(2):178-‐183.
7.
Beaton
DE,
Wright
JG,
Katz
JN,
Upper
Extremity
Collaborative
G.
Development
of
the
QuickDASH:
comparison
of
three
item-‐reduction
approaches.
The
Journal
of
bone
and
joint
surgery.
American
volume.
May
2005;87(5):1038-‐1046.
8.
Liang
MH.
Evaluating
measurement
responsiveness.
The
Journal
of
rheumatology.
Jun
1995;22(6):1191-‐1192.
9.
Liang
MH,
Lew
RA,
Stucki
G,
Fortin
PR,
Daltroy
L.
Measuring
clinically
important
changes
with
patient-‐oriented
questionnaires.
Medical
care.
Apr
2002;40(4
Suppl):II45-‐51.
10.
Middel
B,
van
Sonderen
E.
Statistical
significant
change
versus
relevant
or
important
change
in
(quasi)
experimental
design:
some
conceptual
and
methodological
problems
in
estimating
magnitude
of
intervention-‐related
change
in
health
services
research.
International
journal
of
integrated
care.
2002;2:e15.
11.
Boeckstyns
ME.
Wrist
arthroplasty-‐-‐a
systematic
review.
Danish
medical
journal.
May
2014;61(5):A4834.
12.
Herzberg
G,
Boeckstyns
M,
Sorensen
AI,
et
al.
"Remotion"
total
wrist
arthroplasty:
preliminary
results
of
a
prospective
international
multicenter
study
of
215
cases.
J
Wrist
Surg.
Aug
2012;1(1):17-‐22.
13.
Boeckstyns
ME,
Herzberg
G,
Sorensen
AI,
et
al.
Can
total
wrist
arthroplasty
be
an
option
in
the
treatment
of
the
severely
destroyed
posttraumatic
wrist?
J
Wrist
Surg.
Nov
2013;2(4):324-‐329.
14.
Boeckstyns
ME,
Herzberg
G,
Merser
S.
Favorable
results
after
total
wrist
arthroplasty:
65
wrists
in
60
patients
followed
for
5-‐9
years.
Acta
orthopaedica.
Aug
2013;84(4):415-‐419.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-70-320.jpg)
![71
15.
Boeckstyns
MEH,
Herzberg
G.
Periprosthetic
Osteolysis
after
Total
Wrist
Arthroplasty.
Journal
of
Wrist
Surgery.
2014;3(2):101-‐106.
16.
Boeckstyns
ME,
Toxvaerd
A,
Bansal
M,
Vadstrup
LS.
Wear
Particles
and
Osteolysis
in
Patients
With
Total
Wrist
Arthroplasty.
The
Journal
of
hand
surgery
.
2014;39(12):2396-‐2404.
17.
Herup
A,
Merser
S,
Boeckstyns
M.
[Validation
of
questionnaire
for
conditions
of
the
upper
extremity].
Ugeskrift
for
laeger.
Nov
29
2010;172(48):3333-‐3336.
18.
Boeckstyns
MEH,
Merser
S.
Psychometric
Properties
of
two
Questionnaires
in
the
Context
of
Total
Wrist
Arthroplasty.
Danish
medical
journal.
2014;61(11):A4939.
19.
Ritt
MJ,
Stuart
PR,
Naggar
L,
Beckenbaugh
RD.
The
early
history
of
arthroplasty
of
the
wrist.
From
amputation
to
total
wrist
implant.
Journal
of
hand
surgery.
Dec
1994;19(6):778-‐782.
20.
Zipple
J,
Meyer-‐Ralfs
M.
[Themistocles
Gluck
(1853-‐1942),
pioneer
in
endoprosthetics].
Zeitschrift
fur
Orthopadie
und
ihre
Grenzgebiete.
Feb
1975;113(1):134-‐139.
21.
Swanson
AB,
de
Groot
Swanson
G,
Maupin
BK.
Flexible
implant
arthroplasty
of
the
radiocarpal
joint.
Surgical
technique
and
long-‐term
study.
Clinical
orthopaedics
and
related
research.
Jul-‐Aug
1984(187):94-‐106.
22.
Lundkvist
L,
Barfred
T.
Total
wrist
arthroplasty.
Experience
with
Swanson
flexible
silicone
implants,
1982-‐1988.
Scandinavian
journal
of
plastic
and
reconstructive
surgery
and
hand
surgery
/
Nordisk
plastikkirurgisk
forening
[and]
Nordisk
klubb
for
handkirurgi.
1992;26(1):97-‐100.
23.
Schill
S,
Thabe
H,
Mohr
W.
[Long-‐term
outcome
of
Swanson
prosthesis
management
of
the
rheumatic
wrist
joint].
Handchirurgie,
Mikrochirurgie,
plastische
Chirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Handchirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Mikrochirurgie
der
Peripheren
Nerven
und
Gefasse
May
2001;33(3):198-‐206.
24.
Volz
RG.
[Clinical
experiences
with
a
new
total
wrist
prosthesis
(author's
transl)].
Archiv
fur
orthopadische
und
Unfall-‐Chirurgie.
Jul
23
1976;85(2):205-‐209.
25.
Cobb
TK,
Beckenbaugh
RD.
Biaxial
total-‐wrist
arthroplasty.
The
Journal
of
hand
surgery.
Nov
1996;21(6):1011-‐1021.
26.
Meuli
HC.
Arthroplasty
of
the
wrist.
Clinical
orthopaedics
and
related
research.
Jun
1980(149):118-‐125.
27.
Rahimtoola
ZO,
Rozing
PM.
Preliminary
results
of
total
wrist
arthroplasty
using
the
RWS
Prosthesis.
Journal
of
hand
surgery.
Feb
2003;28(1):54-‐60.
28.
Rahimtoola
ZO,
Hubach
P.
Total
modular
wrist
prosthesis:
a
new
design.
Scandinavian
journal
of
plastic
and
reconstructive
surgery
and
hand
surgery
/
Nordisk
plastikkirurgisk
forening
[and]
Nordisk
klubb
for
handkirurgi.
2004;38(3):160-‐165.
29.
Reigstad
A,
Reigstad
O,
Grimsgaard
C,
Rokkum
M.
New
concept
for
total
wrist
replacement.
Journal
of
plastic
surgery
and
hand
surgery.
Jun
2011;45(3):148-‐156.
30.
Menon
J.
Universal
Total
Wrist
Implant:
experience
with
a
carpal
component
fixed
with
three
screws.
The
Journal
of
arthroplasty.
Aug
1998;13(5):515-‐523.
31.
Herzberg
G.
Prospective
study
of
a
new
total
wrist
arthroplasty:
short
term
results.
Chirurgie
de
la
main.
Feb
2011;30(1):20-‐25.
32.
Nydick
JA,
Greenberg
SM,
Stone
JD,
Williams
B,
Polikandriotis
JA,
Hess
AV.
Clinical
outcomes
of
total
wrist
arthroplasty.
The
Journal
of
hand
surgery.
Aug
2012;37(8):1580-‐1584.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-71-320.jpg)
![72
33.
Bellemere
P,
Maes-‐Clavier
C,
Loubersac
T,
Gaisne
E,
Kerjean
Y.
Amandys((R))
implant:
novel
pyrocarbon
arthroplasty
for
the
wrist.
Chirurgie
de
la
main.
Sep
2012;31(4):176-‐
187.
34.
Szalay
G,
Stigler
B,
Kraus
R,
Bohringer
G,
Schnettler
R.
[Proximal
row
carpectomy
and
replacement
of
the
proximal
pole
of
the
capitate
by
means
of
a
pyrocarbon
cap
(RCPI)
in
advanced
carpal
collapse].
Handchirurgie,
Mikrochirurgie,
plastische
Chirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Handchirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Mikrochirurgie
der
Peripheren
Nerven
und
Gefasse
Jan
2012;44(1):17-‐22.
35.
Harlingen
D,
Heesterbeek
PJ,
M
JdV.
High
rate
of
complications
and
radiographic
loosening
of
the
biaxial
total
wrist
arthroplasty
in
rheumatoid
arthritis:
32
wrists
followed
for
6
(5-‐8)
years.
Acta
orthopaedica.
Dec
2011;82(6):721-‐726.
36.
Takwale
VJ,
Nuttall
D,
Trail
IA,
Stanley
JK.
Biaxial
total
wrist
replacement
in
patients
with
rheumatoid
arthritis.
Clinical
review,
survivorship
and
radiological
analysis.
The
Journal
of
bone
and
joint
surgery.
British
volume.
Jul
2002;84(5):692-‐699.
37.
Ferreres
A,
Lluch
A,
Del
Valle
M.
Universal
total
wrist
arthroplasty:
midterm
follow-‐up
study.
The
Journal
of
hand
surgery.
Jun
2011;36(6):967-‐973.
38.
Ward
CM,
Kuhl
T,
Adams
BD.
Five
to
ten-‐year
outcomes
of
the
Universal
total
wrist
arthroplasty
in
patients
with
rheumatoid
arthritis.
The
Journal
of
bone
and
joint
surgery.
American
volume.
May
18
2011;93(10):914-‐919.
39.
Radmer
S,
Andresen
R,
Sparmann
M.
Total
wrist
arthroplasty
in
patients
with
rheumatoid
arthritis.
The
Journal
of
hand
surgery.
Sep
2003;28(5):789-‐794.
40.
MacDermid
JC.
Patient-‐Reported
Outcomes:
State-‐of-‐the-‐Art
Hand
Surgery
and
Future
Applications.
Hand
clinics.
Aug
2014;30(3):293-‐304.
41.
Liberati
A,
Altman
DG,
Tetzlaff
J,
et
al.
The
PRISMA
statement
for
reporting
systematic
reviews
and
meta-‐analyses
of
studies
that
evaluate
healthcare
interventions:
explanation
and
elaboration.
Bmj.
2009;339:b2700.
42.
Murray
DW,
Carr
AJ,
Bulstrode
C.
Survival
analysis
of
joint
replacements.
The
Journal
of
bone
and
joint
surgery.
British
volume.
Sep
1993;75(5):697-‐704.
43.
Olivecrona
H,
Noz
ME,
Maguire
GQ,
Jr.,
Zeleznik
MP,
Sollerman
C,
Olivecrona
L.
A
new
computed
tomography-‐based
radiographic
method
to
detect
early
loosening
of
total
wrist
implants.
Acta
radiologica.
Nov
2007;48(9):997-‐1003.
44.
Hansen
TB,
Larsen
K,
Bjergelund
L,
Stilling
M.
Trapeziometacarpal
joint
implants
can
be
evaluated
by
roentgen
stereophotogrammetric
analysis.
The
Journal
of
hand
surgery,
European
volume.
Jul
2010;35(6):480-‐485.
45.
Streiner
D,
Norman
G.
Health
measurements
scales:
a
practical
guide
to
their
developement
and
use.
New
York:
Oxford
University
Press;
2008.
46.
Guillemin
F,
Bombardier
C,
Beaton
D.
Cross-‐cultural
adaptation
of
health-‐related
quality
of
life
measures:
literature
review
and
proposed
guidelines.
Journal
of
clinical
epidemiology.
Dec
1993;46(12):1417-‐1432.
47.
Schonnemann
JO,
Hansen
TB,
Soballe
K.
Translation
and
validation
of
the
Danish
version
of
the
Patient
Rated
Wrist
Evaluation
questionnaire.
Journal
of
plastic
surgery
and
hand
surgery.
Dec
2013;47(6):489-‐492.
48.
Pierrart
J,
Bourgade
P,
Mamane
W,
Rousselon
T,
Masmejean
EH.
Novel
approach
for
posttraumatic
panarthritis
of
the
wrist
using
a
pyrocarbon
interposition
arthroplasty
(Amandys((R))):
Preliminary
series
of
11
patients.
Chirurgie
de
la
main.
Sep
2012;31(4):188-‐194.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-72-320.jpg)
![73
49.
Isselin
J.
[Partial
wrist
prosthesis:
concept
and
preliminary
results
in
13
cases].
Chirurgie
de
la
main.
Jun
2003;22(3):144-‐147.
50.
Lirette
R,
Kinnard
P.
Biaxial
total
wrist
arthroplasty
in
rheumatoid
arthritis.
Canadian
journal
of
surgery.
Journal
canadien
de
chirurgie.
Feb
1995;38(1):51-‐53.
51.
Cobb
TK,
Beckenbaugh
RD.
Biaxial
long-‐stemmed
multipronged
distal
components
for
revision/bone
deficit
total-‐wrist
arthroplasty.
The
Journal
of
hand
surgery.
Sep
1996;21(5):764-‐770.
52.
Courtman
NH,
Sochart
DH,
Trail
IA,
Stanley
JK.
Biaxial
wrist
replacement.
Initial
results
in
the
rheumatoid
patient.
Journal
of
hand
surgery.
Feb
1999;24(1):32-‐34.
53.
Rizzo
M,
Beckenbaugh
RD.
Results
of
biaxial
total
wrist
arthroplasty
with
a
modified
(long)
metacarpal
stem.
The
Journal
of
hand
surgery.
Jul
2003;28(4):577-‐584.
54.
Stegeman
M,
Rijnberg
WJ,
van
Loon
CJ.
Biaxial
total
wrist
arthroplasty
in
rheumatoid
arthritis.
Satisfactory
functional
results.
Rheumatology
international.
Apr
2005;25(3):191-‐194.
55.
Kretschmer
F,
Fansa
H.
[BIAX
total
wrist
arthroplasty:
management
and
results
after
42
patients].
Handchirurgie,
Mikrochirurgie,
plastische
Chirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Handchirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Mikrochirurgie
der
Peripheren
Nerven
und
Gefasse
Aug
2007;39(4):238-‐248.
56.
Ferlic
DC,
Clayton
ML.
Results
of
CFV
total
wrist
arthroplasty:
review
and
early
report.
Orthopedics.
Dec
1995;18(12):1167-‐1171.
57.
Levadoux
M,
Legre
R.
Total
wrist
arthroplasty
with
Destot
prostheses
in
patients
with
posttraumatic
arthritis.
The
Journal
of
hand
surgery.
May
2003;28(3):405-‐413.
58.
Fourastier
J,
Le
Breton
L,
Alnot
Y,
Langlais
F,
Condamine
JL,
Pidhorz
L.
[Guepar's
total
radio-‐carpal
prosthesis
in
the
surgery
of
the
rheumatoid
wrist.
Apropos
of
72
cases
reviewed].
Revue
de
chirurgie
orthopedique
et
reparatrice
de
l'appareil
moteur.
1996;82(2):108-‐115.
59.
Meuli
HC.
Hand
Arthroplasties.
London:
Martin
Dunitz;
2000.
60.
Vogelin
E,
Nagy
L.
Fate
of
failed
Meuli
total
wrist
arthroplasty.
Journal
of
hand
surgery.
Feb
2003;28(1):61-‐68.
61.
Strunk
S,
Bracker
W.
[Wrist
joint
arthroplasty:
results
after
41
prostheses].
Handchirurgie,
Mikrochirurgie,
plastische
Chirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Handchirurgie
:
Organ
der
Deutschsprachigen
Arbeitsgemeinschaft
fur
Mikrochirurgie
der
Peripheren
Nerven
und
Gefasse
Jun
2009;41(3):141-‐147.
62.
Reigstad
O,
Lutken
T,
Grimsgaard
C,
Bolstad
B,
Thorkildsen
R,
Rokkum
M.
Promising
one-‐
to
six-‐year
results
with
the
Motec
wrist
arthroplasty
in
patients
with
post-‐
traumatic
osteoarthritis.
The
Journal
of
bone
and
joint
surgery.
British
volume.
Nov
2012;94(11):1540-‐1545.
63.
Pech
J,
Veigl
D,
Dobias
J,
Popelka
S,
Bartak
V.
[First
experience
with
total
wrist
replacement
using
an
implant
of
our
design].
Acta
chirurgiae
orthopaedicae
et
traumatologiae
Cechoslovaca.
Aug
2008;75(4):282-‐287.
64.
Marcuzzi
A,
Ozben
H,
Russomando
A.
The
use
of
a
pyrocarbon
capitate
resurfacing
implant
in
chronic
wrist
disorders.
The
Journal
of
hand
surgery,
European
volume.
Aug
20
2013.
65.
Cooney
W,
Manuel
J,
Froelich
J,
Rizzo
M.
Total
Wrist
Replacement:
A
Retrospective
Comparative
Study.
Journal
of
Wrist
Surgery.
2012;1(2):165-‐172.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-73-320.jpg)
![74
66.
Bidwai
AS,
Cashin
F,
Richards
A,
Brown
DJ.
Short
to
medium
results
using
the
remotion
total
wrist
replacement
for
rheumatoid
arthritis.
Hand
surgery
:
an
international
journal
devoted
to
hand
and
upper
limb
surgery
and
related
research
:
journal
of
the
Asia-‐Pacific
Federation
of
Societies
for
Surgery
of
the
Hand.
2013;18(2):175-‐178.
67.
Kraay
MJ,
Figgie
MP.
Wrist
arthroplasty
with
the
trispherical
total
wrist
prosthesis.
Seminars
in
arthroplasty.
Jan
1995;6(1):37-‐43.
68.
van
Winterswijk
PJ,
Bakx
PA.
Promising
clinical
results
of
the
universal
total
wrist
prosthesis
in
rheumatoid
arthritis.
Open
Orthop
J.
2010;4:67-‐70.
69.
Morapudi
SP,
Marlow
WJ,
Withers
D,
Ralte
P,
Gabr
A,
Waseem
M.
Total
wrist
arthroplasty
using
the
Universal
2
prosthesis.
Journal
of
orthopaedic
surgery.
Dec
2012;20(3):365-‐368.
70.
Adams
BD.
Wrist
arthroplasty:
partial
and
total.
Hand
clinics.
Feb
2013;29(1):79-‐89.
71.
Bosco
JA,
3rd,
Bynum
DK,
Bowers
WH.
Long-‐term
outcome
of
Volz
total
wrist
arthroplasties.
The
Journal
of
arthroplasty.
Feb
1994;9(1):25-‐31.
72.
Gellman
H,
Hontas
R,
Brumfield
RH,
Jr.,
Tozzi
J,
Conaty
JP.
Total
wrist
arthroplasty
in
rheumatoid
arthritis.
A
long-‐term
clinical
review.
Clinical
orthopaedics
and
related
research.
Sep
1997(342):71-‐76.
73.
Meuli
HC.
Meuli
total
wrist
arthroplasty.
Clinical
orthopaedics
and
related
research.
Jul-‐
Aug
1984(187):107-‐111.
74.
Palmer
AK,
Werner
FW,
Murphy
D,
Glisson
R.
Functional
wrist
motion:
a
biomechanical
study.
The
Journal
of
hand
surgery.
Jan
1985;10(1):39-‐46.
75.
Ryu
JY,
Cooney
WP,
3rd,
Askew
LJ,
An
KN,
Chao
EY.
Functional
ranges
of
motion
of
the
wrist
joint.
The
Journal
of
hand
surgery.
May
1991;16(3):409-‐419.
76.
Krukhaug
Y,
Lie
SA,
Havelin
LI,
Furnes
O,
Hove
LM.
Results
of
189
wrist
replacements.
A
report
from
the
Norwegian
Arthroplasty
Register.
Acta
orthopaedica.
Aug
2011;82(4):405-‐409.
77.
Reigstad
A,
Mjorud
J.
Results
of
189
wrist
replacements.
Acta
orthopaedica.
Feb
2012;83(1):101;
author
reply
101-‐102.
78.
Murphy
DM,
Khoury
JG,
Imbriglia
JE,
Adams
BD.
Comparison
of
arthroplasty
and
arthrodesis
for
the
rheumatoid
wrist.
The
Journal
of
hand
surgery.
Jul
2003;28(4):570-‐
576.
79.
Cavaliere
CM,
Chung
KC.
A
systematic
review
of
total
wrist
arthroplasty
compared
with
total
wrist
arthrodesis
for
rheumatoid
arthritis.
Plastic
and
reconstructive
surgery.
Sep
2008;122(3):813-‐825.
80.
Nydick
JA,
Watt
JF,
Garcia
MJ,
Williams
BD,
Hess
AV.
Clinical
Outcomes
of
Arthrodesis
and
Arthroplasty
for
the
Treatment
of
Post-‐Traumatic
Wrist
Arthritis.
The
Journal
of
hand
surgery.
Apr
2
2013.
81.
Groot
D,
Gosens
T,
Leeuwen
NC,
Rhee
MV,
Teepen
HJ.
Wear-‐induced
osteolysis
and
synovial
swelling
in
a
patient
with
a
metal-‐polyethylene
wrist
prosthesis.
The
Journal
of
hand
surgery.
Dec
2006;31(10):1615-‐1618.
82.
Zilber
S,
Radier
C,
Postel
JM,
Van
Driessche
S,
Allain
J,
Goutallier
D.
Total
shoulder
arthroplasty
using
the
superior
approach:
influence
on
glenoid
loosening
and
superior
migration
in
the
long-‐term
follow-‐up
after
Neer
II
prosthesis
installation.
Journal
of
shoulder
and
elbow
surgery
/
American
Shoulder
and
Elbow
Surgeons
...
[et
al.].
Jul-‐Aug
2008;17(4):554-‐563.
83.
Herzberg
G.
Periprosthetic
bone
resorption
and
sigmoid
notch
erosion
around
ulnar
head
implants:
a
concern?
Hand
clinics.
Nov
2010;26(4):573-‐577.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-74-320.jpg)
![76
Paper
I
DANISH MEDICAL JOURNAL
ABSTRACT
INTRODUCTION: Severely painful or dysfunctional destroyed
wrists can be reconstructed by fusion, interposition of soft-
tissue or by arthroplasty using artificial materials. Total and
partial wrist arthroplasty (T/PWA) has been used on a regu-
lar basis since the 1960’s. The objective of this study was to
review the literature on second, third and fourth generation
implants.
METHODS: The review was conducted according to the
PRISMA – guidelines. A search was made using a proto-
colled strategy and well-defined criteria in PubMed, in the
Cochrane Library and by screening reference lists.
RESULTS: 37 publications describing a total of 18 implants
were selected for analysis. 16 of the publications were use-
ful for the evaluation of implant longevity. Despite method-
ological shortcomings in many of the source documents, a
summary estimate was possible.
CONCLUSION: It seems that T/PWA has a good potential to
improve function through pain reduction and preservation
of mobility. The risk of severe complications – deep infec-
tion and instability problems – is small with the available
implants. Implant survival of 90-100% at five years are re-
ported in most series – if not all – using newer second gen-
eration and third generation implants, but declines from
five to eight years. Periprosthetic osteolysis/radiolucency is
frequently reported. Its causes and consequences are not
clarified.
Painful, dysfunctionally destroyed wrists can be recon-
structed by fusion, interposition of soft-tissue or arthro-
plasty using artificial materials. Total or partial wrist ar-
throplasty (T/PWA) was attempted in the beginning of
the twentieth century and has been used on a more
regular basis since the 1960s. Several generations of im-
plants exist, the first being interposition of single-com-
ponent silicone implants, a procedure that is hardly ever
used today [1].
The second generation of implants was multi-com-
ponent implants [2-6]. There is no consensus on the def-
inition of second generation. Herein, we define it as an
implant consisting of a radial component and a carpal
component, fixated in one or more of the metacarpal
bones. Some of these systems have been developed
after the introduction of the third generation [7].
The third generation of implants is characterised by
minimal bone resection to avoid fixation in the metacar-
pal bones, with the exception of an optional and re-
stricted fixation in the second metacarpal. These im-
plants attempt to mimic the natural anatomy and
biomechanics of the wrist and the implants are largely
unconstrained [8-10]. Pyrocarbon was recently intro-
duced as a single-component interposition arthroplasty
[11] or hemiarthroplasty [12]. We define these as
“fourth generation” implants.
The objective of this study was to review the litera-
ture concerning T/PWA using second, third and fourth
generation implants. The questions to be answered
were: What is the present knowledge on clinical results,
complications and implant longevity. An effort was
made to draw general conclusions rather than to de-
scribe the results obtained in individual series.
METHODS
The review was conducted according to the PRISMA
guidelines [13].
Search strategy
We made a primary search through PubMed with the
Mesh terms “Wrist Arthroplasty” and “Wrist Replace-
ment”. We restricted the search to the 1994-2013-
period, considering earlier material to have historical
value only. We made a second search in the Cochrane
Library and a continuous supplementary search by scan-
ning the reference lists of the papers first included.
The inclusion criteria were: papers with primary
clinical data on second, third and fourth generation im-
plants. Excluded were: cadaveric studies; biomechanical
studies; studies not accessible in journals, books or on-
line; reviews without primary data. Double publications
and articles with overlap of cases were relative exclusion
criteria. Articles not written in English, Danish, Swedish,
Norwegian, French, Dutch or German were evaluated on
the basis of an English abstract, if available.
Quality assessment and handling of data
We focused on the number of cases, the methodology
and the observation period. Papers with less than ten
cases were considered to be less useful and are there-
fore only mentioned very briefly. Implant longevity was
primarily evaluated on the basis of papers with a cumu-
lated implant survival of at least five years; secondarily,
papers with a follow-up of a minimum of two years in
each case. Function was evaluated by well-validated and
relevant outcome measurement tools like the Disabil-
Michel E. H. Boeckstyns
SYSTEMATIC
REVIEW
Clinic for Hand Surgery,
Gentofte Hospital
Dan Med J
2014;61(5):A4834](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-76-320.jpg)
![77
DANISH MEDICAL JOURNAL
ities of Arm, Shoulder and Hand (DASH/QuickDASH), the
Patient-Rated Wrist Evaluation (PRWE) or the Michigan
Hand Questionnaire (MHQ). Series with clinical data col-
lected before operation and similarly at follow-up were
defined as prospective, even if there had been no men-
tion of a preoperative protocol. We made an effort to
clarify whether the authors were involved as inventors,
developers, or producers.
RESULTS
Selected publications
A total of 56 papers were eligible (Figure 1). Screening
for double publication or overlap of data led to the ex-
clusion of 12 papers [3, 7, 9-10, 14-21]. One paper [22]
was a retrospective review of TWA using three implants,
with a large overlap concerning the Biaxial implant with
two other included papers [4, 23], and there were data
on eight cases only concerning the second implant, the
Universal 2. Thus, only data concerning the Remotion
were used despite important methodological limitations
in this paper. Seven publications comprised less than ten
cases, which left 37 articles for final analysis of which 16
fulfilled the criteria for analysis of longevity. The eligible
studies represent a maximum of 1,127 cases, but the
precise number is probably somewhat smaller due to a
possible minor overlap between some of the series. 71%
were rheumatoid, 6% scapholunate advanced collapse
(SLAC) wrists, 4% scapho-nonunion advanced collapse
(SNAC) wrists, 4% other posttraumatic causes, 4% other
degenerative causes, 2% Kienboeck’s disease, and 9%
other or not well specified causes.
Implants
A total of 18 different implants were reported, including
certain modifications (Table 1). Of these, seven are no
longer available: the APH [19], Biaxial [4], CFV [24], Des-
tot [25], Meuli [3], Trispherical [26], Volz [27] and the
Rozing wrist system (RWS) [5]. Three have been rede-
signed: The Guepar [28], now marketed as Horus, the
Aphis [29] and Universal 1 [8]. The following are cur-
rently available: Amandys [11], Maestro [30], Motec [7],
Pech [31], RCPI [32], Remotion [9], Total Modular [6]
and Universal 2 [33]. The Amandys is an interposition
pyrocarbon implant, and the RCPI a pyrocarbon hemiar-
throplasty. All of the remaining devices have a carpal
and a radial component. The radial component of the
FIGURE 1
Flow diagram of search strategy.
Search for “wrist arthroplasty” and
“wrist replacement”:
Mesh-words:](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-77-320.jpg)
![78
DANISH MEDICAL JOURNAL
TABLE 1
Implants, number of cases and methodology in 37 publications.
Reference Implant
Gener-
ation
Cases
(rheumatoid
cases), n
data permitting
comparison
Validated
outcome measures
instrument Change in scores
Pierrart et al, 2012 [68] Amandys IV 11 (0) Not reported QDASH
PRWE
–
Bellemère et al, 2012a
[11] Amandys IV 25 (1) Reported QDASH
PRWE
Improved 27 and 29
points (p < 0.05)
Radmer et al, 2003 [41] APH II 40 (40) Not reported – –
Isselin, 2003a
[29] APHIS III 13 (0) Reported – –
Lirette & Kinnard, 1995 [42] Biaxial II 15 (15) Not reported – –
Cobb & Beckenbaugh, 1996a
[4] Biaxial II 57 (57) Reported – –
Cobb & Beckenbaugh, 1996a
[67] Biaxial (long stem) II 10 (10) Not reported – –
Courtman et al, 1999 [44] Biaxial II 26 (26) Not reportedc
– –
Takwale et al, 2002 [47] Biaxial II 66 (66) Not reported – –
Rizzo & Beckenbaugh, 2003a
[23] Biaxial (long stem) II 17 (approx. 15) Reported – –
Stegeman et al, 2005 [43] Biaxial II 16 (16) Not reported – –
Kretschmer & Fansa, 2007 [46] Biaxial II 42 (3) Reported – –
Van Harlingen et al, 2011 [45] Biaxial II 32 (32) Reported – –
Ferlic & Clayton, 1995a
[24] CFV II 15 (13) Not reported – –
Levadoux & Legré, 2003a
[25] Destot II 27 (0) Not reported – –
Fourastier et al, 1996a
[28] Guepar II 72 (72) Not reported – –
Nydick et al, 2012 [30] Maestro III 23 (5) Reported DASH Not recorded
preoperatively
Meuli, 2000 [52] Meuli II 54 (approx. 45) Not reported – –
Vögelin & Nagy, 2003 [66] Meuli II 16 (13) Not reported – –
Strunk & Bracker, 2009 [48] Meuli, Biaxial, Universal 2 II, II, III 41 (38) Not reported DASH –
Reigstad et al, 2012a
[36] Motec (II) 30 (0) Reported DASH Improved 26 points
(p < 0.05)
Pech et al, 2008a
[31] Pech II 32 (32) –e
– –
Marcuzzi et al, 2013 [32] RCPI IV 35 (0) Reported DASH Improved 45 points
(p < 0.05)
Cooney et al, 2012a
[22] Remotion III 22 (?) Reported DASH -
Herzberg et al, 2012 [38] Remotion III 112 (75) Reported QDASH Improved 21 points
(NS)
Bidwai et al, 2013 [51] Remotion III 10 (10) Reported – –
Rahimtoola & Rozing, 2003a
[5] RWS II 29 (approx. 27) Reported – –
Rahimtoola & Hubach, 2004a
[6] Total Modular II 32 (29) Reported – –
Kraay & Figgie, 1995b
[26] Trispherical II 35 (35) Not reportedd
(HSS) (Improved, significance
not reported)
Menon, 1998a
[8] Universal 1 III 31 (23) Reported – –
Van Winterswijk & Bakx, 2010 [40] Universal 2 III 17 (16) Reported DASH Improved 24 points
(significance not
reported)
Ferreres et al, 2011 [50] Universal 1/2 III 21 (15) Not reported PRWE –
Ward et al, 2011a
[39] Universal 1 III 24 (24) Reported DASH Improved 22 points
(significance not
reported)
Morapudi et al, 2012 [37] Universal 2 III 21 (19) Reported DASH
PRWE
Improved 10 and
46 points (p < 0.05)
Adams, 2013a
[33] Universal 2
(hemiarthroplasty using
radial component)
(III) 26 (3) Not reported – –
Bosco et al, 1994 [27] Volz II 18 (14) Not reported – –
Gellman et al, 1997 [49] Volz II 14 (14) Not reported – –
Total
APH = anatomic-physiologic; APHIS = Arthroplastie Physiologique Isselin; CFV = Clayton Ferlic Volz; DASH = Disabilities of Arm, Shoulder and Hand; HSS = hospital for special surgery;
PRWE = Patient-Rated Wrist Evaluation; QDASH = QuickDASH; RCPI = Resurfacing Capitate Pyrocarbon Implant; RWS = Rozing Wrist System.
a) Some of the authors may be involved in the development or production of the implant; b) No clear available information on the authors’ affiliation to the production; c) Only sum
flexion – extension and of radial-ulnar reported, but without mention of statistical significance; d) HSS-score reported – this scoring system was not eligible according to the protocol
due to its restricted use and validation; e) Full text in Czech, only abstract available in English.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-78-320.jpg)
![79
DANISH MEDICAL JOURNAL
Universal, the Remotion and the Maestro have been
used as hemiarthroplasties [33-35]. The APH and the
Motec are metal-on-metal prostheses; all others are
metal-on-polyethylene. Only the Trispherical is fully con-
strained. For further details concerning all these im-
plants, we refer to the primary publications.
Clinical results
Six papers provided preoperative as well as post-opera-
tive data on function, all reporting improvement (Table
1): four reported statistical significance [11, 32, 36, 37],
one a statistically non-significant improvement [38] and
two papers did not report significance [39, 40]. In two of
the papers, a t-test was used to assess significance,
which is debatable since the scoring systems are based
on ordinal scales [36, 37].
The mean or median range of flexion-extension at
follow-up was reported in 32 papers and ranged from 15
to 89 degrees. The mean or median range of radial-ulnar
deviation was reported in 27 papers and ranged from
seven to 48 degrees (Table 2).
In all, 13 of 36 papers reported grip strength at fol-
low-up, but only ten compared grip strength with pre-
operative values, eight showing increased and two de-
creased values.
A total of 12 papers evaluated pain on a visual ana-
logue scale, 14 on a verbal Likert scale and one used the
pain section of the PRWE. Thirteen of these 26 papers
demonstrated improvement of mean values and nine re-
ported statistical significance. The other 14 had no pre-
operative values for comparison. Clear information con-
cerning pain was missing in ten papers.
Complications
Besides the important issue of prosthetic loosening, we
selected two major complications because we expected
these to be most consistently defined and reported.
Deep infection (early or late) was reported in a total of
16 cases (1.4%). The infection rate ranged from 0% (in
23 series) to 13% [24]. Instability problems were related
to certain implants. Radmer reported 32 cases of “loos-
ening with subsequent dislocation” out of 40 cases using
the APH prosthesis [41], the main reason for abandoning
the use of this implant. A total of 22 of 278 (8%) Biax im-
plants in seven series were reported to have dislocated
[4, 42-48], and four out of 32 (13%) Volz prostheses
were reported to have subluxed or dislocated in two ser-
ies [27, 49]. Menon [8] reported dislocation of five out
of 37 (14%) cases, and Ward [39] reported one persis-
tent instability and one dislocation out of 24 Universal 1
TABLE 2
Motion at follow-up in publications on currently available implants.
Total range of motion
Implant
post-oper
degrees
change compared
degrees
post-oper
degrees
change compared
degrees
post-oper
degrees
change compared
degrees
Amandys
Bellemere et al, 2012 [11] 68 1 NS 36 0 NS – – –
Pierrart et al, 2012 [68] 71 – – 36 – – – – –
Maestro
Nydick et al, 2012 [30] 90 5 NS 43 8 < 0.05 – – –
Motec
Reigstad et al, 2012 [36] 120 16 NS
Pech
Pech et al, 2008 [31] – – - - – – – – –
RCPI
Marcuzzi et al, 2013 [32] 67 17 < 0.05 24 17 < 0.05 – – –
Remotion
Herzberg et al, 2012 [38] 66 –4 NS 33 2 < 0.05
for radial
flexion
– – –
Cooney et al, 2012 [22] 67 –6 – 27 7 – – – –
Bidwai et al, 2013 [51] 61 38 < 0.05 22 – – – – –
Total Modular
Rahimtoola & Hubach,
2004 [6]
63 17 < 0.05 24 7 < 0.05
for ulnar
flexion
– – –
Universal 2
Morapudi et al, 2012 [37] 53 15 < 0.05 – – – – – –
NS = non-significant; RCPI = Resurfacing Capitate Pyrocarbon Implant.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-79-320.jpg)
![80
DANISH MEDICAL JOURNAL
cases (8%). Van Winterswijk [40] reported dislocation in
one out of 17 Universal cases. This instability problem
seems to have been solved with the modified version,
the Universal 2 [37, 50].
Dislocation has been only a very small problem with
the Remotion: one in 144 reported cases (< 1%) [22, 38,
51]. In the two Amandys series, problems were seen in
seven out of 36 cases (19%). One recurrent subluxation
was reported out of 13 Isselin [29] implants, and one in-
stability problem out 23 Maestro implants [30]. No dislo-
cations or other instability problems worth mentioning
have been reported following the Destot, GUEPAR,
Meuli, Motec, Pech, RWS, Trispherical or RCPI [5, 25, 26,
28, 31, 32, 36, 51].
Radiology
Osteolysis or radiolucency at follow-up, with or without
loosening of the prosthetic components, was assessed in
varying ways. In 13 of the 37 series, no useful informa-
tion could be retrieved, whereas 20 papers reported os-
teolysis, ten of these mentioning radiolucency without
frank loosening of the implant components [5, 23, 36,
38, 39, 42, 45, 49-51].
In a consecutive series of Biaxial TWA with a follow-
up time of 5-9 years, there was progressive radiolucency
at the carpal component in 12 out of 46 wrists, seven of
which were revised. Subsidence of the carpal compo-
nent was present in seven cases after one year and in 20
cases at final follow-up [4].
Ten papers provided data that permitted an evaluation
of the cumulated survival at five years or more (Table 3).
Eight reported a cumulated five-year survival of 90% or
more and one a cumulated five-year survival of 75%. The
last paper reported 0.83 at ten years.
Small series
Seven papers included less than ten cases. Boyer &
Adams used the radial component of a Universal 2 total
wrist arthroplasty system in two rheumatoid cases as a
hemiarthroplasty in combination with a proximal row
carpectomy [34]. Roux developed a hemiarthroplasty for
usage primarily in comminuted distal radius fractures
with irreparable joint surfaces [53]. Lorei et al used a
custom Trispherical implant for the revision of three
failed TWAs [54]. O’Flynn reported on a single case of
failure of the hinge mechanism in a Trispherical TWA
[55]. Talwalkar et al reported on five revision Biaxial re-
placements [56]. Lundborg et al published five cases us-
ing a titanium/polyethylene ball-and-socket articulation
fixated with osseointegrated Titanium screws [18] and
with a further follow-up [57]. Daruwalla presented a
series of six Amandys pyrocarbon implants [58].
DISCUSSION
Although this review used systematic search criteria and
protocol inclusion and exclusion criteria, it was limited
by the quality of the source reports. After exclusion of
TABLE 3
Cumulated survival rate and/or revision rate of implants in 16 publications.
rate, n mean (range), yrsReference Implant Diagnosis at 5 yrs at 8 yrs at 10 yrs
Radmer et al, 2003 [41] APH RA (PSA, OA)b
– – – 36/37 4.3 (2-6.1)
Courtman et al, 1999 [44] Biaxial RA/PSA 1.0 – – – 2.8 (2-5.2)
Van Harlingen et al, 2011 [45] Biaxial RA 0.90c
0.81 – – 6.0 (5-8)
Cobb & Beckenbaugh, 1996a
[4] Biaxial RA – – 0.83 – 6.5 (5-9.9)
Takwale et al, 2002 [47] Biaxial RA 0.90c
0.83 – – 4.3 (1-8.3)
Cobb & Beckenbaugh, 1996a
[67] Biaxial (used for revision) RA – – – 2/10 3.8 (3-4.8)
Rizzo & Beckenbaugh, 2003a
[23] Biaxial (long stem) RA (OA)b
1.0 1.0 – – 6.2 (4.1-8.6)
Meuli, 2000a
[52] Meuli RA/PT 0.92 0.77 – – –(0.5-13)
Reigstad et al, 2012 [36] Motec SLAC/SNAC 0.93 – – – 3.2 (1.1-6.1)
Herzberg et al, 2012 [38] Remotion RA/PT/OA 0.92 0.92 – – 4.0 (2-8)
Rahimtoola & Rozing, 2003a
[5] RWS RA (PSA, OA)b
– – – 1/29 4.0 (2-8)
Menon, 1998a
[8] Uni 1 RA/OA – – – 4/37 6.7 (4-10)
Ward et al, 2011a
[39] Uni 1 RA 0.75 0.62c
0.40c
– 7.3 (5-10.8)
Ferreres et al, 2011 [50] Uni 1 and 2 RA (PSA, OA, misc.)b
1.0 1.0 – – 5.5 (3.2-8.8)
Gellman et al, 1997 [49] Volz RA – – – 1/14 6.5 (3.5-11.5)
Bosco et al, 1994 [27] Volz RA (PT)b
– – – 1/18 8.6 (3.5-12.5)
APH = anatomic-physiologic; OA = degenerative osteoarthritis; PSA = psoriatic arthritis; PT = posttraumatic arthritis; RA = rheumatoid arthritis; SLAC = scapholunate advanced col-
lapse; SNAC = scaphoid non-union advanced collapse.
a) Some of the authors may be involved in the development or production of the implant.
b) Diagnosis in bracket because of small percentage.
c) Evaluated on an illustration showing the cumulated implant survival curve in the publication.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-80-320.jpg)
![81
DANISH MEDICAL JOURNAL
one paper for language reasons and one paper reporting
data as a part of a less commonly used scoring system,
no more than 17 publications were prospective, even
when using a broad definition: data collected preopera-
tively as well as post-operatively. Of these 17 papers,
eight used a validated and widely used outcome meas-
urement system. This weakness of methodology applies
mainly to second generation implants. In at least 16 of
the 37 papers, one or several authors were involved as
or close to the inventors, developers or producers, but
this seemed not to have had an impact on the reported
clinical or longevity results. Finally, due to the lack of
more detailed information, our analyses were limited to
calculation of mean or median values, whereas calcula-
tion of statistically significant differences was impos-
sible. Despite these weaknesses, we find that some sum-
mary estimate of the results after T/PWA and some
general conclusions are possible.
The majority of the data are based on rheumatoid
cases, although other diagnoses are increasingly repre-
sented in recent publications. The general opinion has
generally been that better longevity must be expected in
low-demand patients, typically rheumatoid patients. It is
not possible throughout the different series to compare
results in rheumatoid and non-rheumatoid patients, but
the series of Herzberg [38], which consists of 75 rheuma-
toid and 37 non-rheumatoid cases, draws on prospective
data and concludes that there are no clinically or statis-
tically significant differences. This is consistent with an
emerging consensus that non-rheumatoid patients may
do better because of a better bone stock, provided that
their level of activity is restricted [33].
In terms of complications, it appears that the risk of
deep infection is small. Likewise, it seems that the insta-
bility problems of earlier designs have been solved, ex-
cept for the Amandys implant. Time must show if this re-
quires modification of the implant or if the issue can be
solved by modified surgical techniques.
In general, mean values for motion at follow-up are
similar for most implants and within the functional
range defined by Palmer et al [59], although somewhat
smaller than the more rigorous range defined by Ryu &
Cooney [60] (Table 2). An exception may be the Maestro
that showed better motion in the single series with this
implant [30]. On the other hand, there is less consist-
ency concerning the change in motion from before oper-
ation to follow-up. This may be attributed to different
case selections, different post-operative protocols or
factors related to the implant itself, but it is impossible
to clarify this on basis of the published data. The general
tendency is that the mean level of function, as evaluated
with patient-rated outcome measures, increases, and
that pain is reduced. However, a general summary of the
extent of the pain reduction through the different re-
ports is impossible.
The main advantage of T/PWA over total wrist fu-
sion (TWF) is claimed to be a higher degree of function-
ality. Although many patients with bilateral procedures
– TWA on one side and TWF on the other – would have
preferred arthroplasty on both sides, this is not always
the case [47]. The present work did not aim to make a
comparison between these two solutions, but the ques-
tion is important. Murphy et al made a comparison be-
tween TWA (24 rheumatoid wrists) and TWF (27 rheu-
matoid wrists) in a retrospective design [20]. Treatment
groups were well matched by patient characteristics and
radiographic staging. There were no statistically signifi-
cant differences between arthroplasty and arthrodesis
in either DASH or PRWE scores.
Cavaliere & Chung compared TWA with TWF in a
systematic review of the literature [61]. They identified
18 total wrist arthroplasty studies representing 503 pro-
cedures and 20 TWF studies representing 860 proced-
ures in rheumatoid patients. They concluded that the
outcomes for TWF were comparable and possibly better
than those for TWA. One major limitation in that study
was that the methodology in the source publications
was often very weak.
In a subsequent study [62], TWA was associated
with the highest expected gain in quality-adjusted life-
years (QALY). This finding reflects the attitude of medical
specialists, but is, of course, not evidence of the super-
iority of TWA. In a third study, the authors compared
costs per QALY [63]. TWA turned out to have only a
small incremental cost over the traditional TWF proced-
ure. However, this study is limited by the uncertainty as-
sociated with utility values, life span and complication
rates. Especially, we question the assumption in the
model, that prostheses are durable enough to last the
duration of the patient’s life.
Nydick et al compared TWA (seven wrists) and TWF
(15 wrists) [10] in posttraumatic arthritis. The PRWE
scores were significantly better in the arthroplasty
group, but there were no differences in DASH scores.
FACT BOX
Several generations of total wrist arthroplasty have been used on a regular basis since the 1960s and
hemiarthroplasty has been introduced in recent years.
Many designs have been utilised and quite a few abandoned or modified. Currently, ten different im-
plants are available.
Wrist arthroplasty has a good potential for improvement of function through pain reduction and preser-
vation of mobility, but its superiority above total wrist fusion has not been proven in controlled ran-
domised trials.
The five-year implant survival is higher than 90% in most series using late second generation and third
generation implants. Implant survival seems to decline from five to eight years.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-81-320.jpg)
![82
DANISH MEDICAL JOURNAL
Besides its retrospective design, the weakness of this
study was the very small number of TWA and the fact
that all cases had been treated at the same clinic, imply-
ing that there had been a preoperative decision to pre-
fer TWA in some patients and TWF in others.
In our study, a reasonable appreciation of the lon-
gevity of the implants was possible in 16 papers, al-
though only ten provided information on cumulated im-
plant survival. The most widely accepted and commonly
used definition of failure in implant survival analysis is
“removal of implants”, but the decision to remove an
implant depends on the attitude of the surgeons: Some
might advise not to remove an implant, even in the pres-
ence of some (tolerable) pain; some might advise re-
moval of an implant with periprosthetic osteolysis, even
if the implant seems to be stable and in the absence of
pain. Thus, it is argued that other definitions should be
considered, but until another consensus is reached, re-
moval of implants remains the definition of choice.
Generally, the five-year implant survival rate was
higher than 90% (Table 3), but declining at eight years.
One exception is the low survival reported by Ward et al
[39]. This series contains exclusively rheumatoid cases,
but there were no statistically significant differences be-
tween the ten revised and ten non-revised wrists in
terms of age, Simmen classification, dominance or pre-
operative DASH score. Another notable result concerns
the metal-on-metal APH prosthesis. Solitary loosening of
the carpal component was predominant. The authors
believed that the main cause of loosening was bone re-
sorption induced by titanium debris, and they aban-
doned the use of this implant [41]. Krughaug et al re-
ported on the survival of 189 TWA in the Norwegian
Arthroplasty Register [64]: The cumulated survival of the
Biax was 85% at five years and approximately 78% at
eight years, which is somewhat lower than in the series
we have analysed. The survival of the Gibbon/Motec
was obviously lower than that published by Reigstad et
al [36], which can possibly be attributed to underreport-
ing to the register [65].
Six papers merely permitted a calculation of the re-
vision rate, which is much weaker information. Indeed,
a given revision rate in series with a long observation
period has a quite different value than the same revision
rate in a series with a short observation period. Failed
TWA can successfully be revised by fusion [8, 15, 22, 36,
39, 41, 66], by total or partial replacement of the com-
ponents [8, 15, 22, 39, 66, 67] or by total or partial re-
moval of the components with or without soft-tissue
interposition, typically fascia lata [4, 39].
Although reported in 20 articles, periprosthetic os-
teolysis/radiolucency, with or without gross loosening,
has been systematically investigated in two series only
[4, 47]. The remaining studies report on the phenom-
enon but use no standardised definitions or methods.
Osteolysis occurred frequently around both the radial
and carpal components, whereas frank loosening of the
component was more frequent on the carpal side.
Radiostereographic studies have not been published.
The cause of periprosthetic osteolysis is not clear,
but has been attributed to a local osteolytic reaction to
metallic or polyethylene debris. In this review, we can
confirm that it occurs in metal-on-polyethylene [4-6, 23,
27, 28, 39, 43-47, 49-51] as well as in metal-on-metal
prostheses [36, 41], but we are unable to clarify its
causes or consequences. To our knowledge, no system-
atic analyses of metallic ion levels in blood have been
published [36, 41].
CONCLUSION
Despite the methodological shortcomings in a consider-
able proportion of the published papers, some general
conclusions are possible. It seems that T/PWA has a
strong potential for improvement of function through
pain reduction and preservation of mobility. The risk of
severe complications – deep infection and instability
problems – is small with the available implants. An im-
plant survival of 90-100% at five years is reported in
most series – if not all – using newer second generation
and third generation implants, but implant survival de-
clines from five to eight years.
There is a need of continuous research with a focus
on indications (rheumatoid versus non rheumatoid, age-
groups, level of activity etc.) and on long-term results
achieved through large prospective multicentre studies,
national registries or even with post-market surveillance
registries of implants that are no longer available.
Furthermore, the question as to which extent and on
what indications TWA is superior to TWF still needs to
be answered definitely.
Finally, the possible causes and consequences of
the frequently reported periprosthetic loosening must
be exposed by radiostereographical methods, histo-
X-ray of the Remotion
total wrist arthroplasty.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-82-320.jpg)



![86
The Kaplan–Meier survival graphs are shown in ►Figs. 2
and 3. At the average follow-up of this study, the survival rate
(with failure defined as implant revision) was 96% in the
rheumatoid group of wrists and 92% in the non-RA group.
Clinical and Radiological Results of 112 Wrists with
More Than 2 Years of Follow-Up
The clinical results (mean: 4 years; minimum: 2 years, maxi-
mum: 8 years) are reported in ►Table 1. Except for radial
deviation and grip strength improvement, we could not find
any statistically significant differences between rheumatoid
and non-RA wrists. Patient’s satisfaction was high both in the
rheumatoid (88% very satisfied or satisfied) and in the non-RA
groups (95% very satisfied or satisfied).
In terms of radiological results, implant positioning was
subjectively judged by the operating surgeon as optimal (86%)
or suboptimal (11%) in 97% of the rheumatoid wrists and 100%
of the non-RA wrists (optimal: 79% and suboptimal: 21%).
Loosening with implant migration was observed in 4% of the
rheumatoid wrists and 3% of the non-RA wrists (nonsignifi-
cant [ns], p ¼ 1.000). Loosening without implant migration
was observed in 8% of the rheumatoid wrists and 15% of the
non-RAwrists (ns, p ¼ 0.2520). Overall, the incidence of signs
of periprosthetic loosening was 12% in the rheumatoid group
compared with 18% in the non-RA group (the Fischer exact
test; level of significance 0.05).
Discussion
The use of TWA to treat end-stage rheumatoid and non-RA
arthritis is very controversial due to the high range of
complications reported in previous series.1
Historically, the
first total silicone wrist implants were abandoned because of
unacceptable revision rates.5
They were followed by a first
generation of metal-polyethylene total wrist arthroplasties
that still had high complications and revisions rates.9
Even
some newer metal-polyethylene prostheses designs showed
at first promising results followed by unacceptable longer
follow-up results.10,11
A recent systematic meta-analysis of a
large series of total wrist arthroplasties (most of the first
generation metal-polyethylene TWA) concluded that existing
data do not support widespread application of TWA for
rheumatoid arthritic wrists.5
This is why many surgeons prefer total wrist fusion to treat
end-stage rheumatoid or non-RA wrist arthritis. Indeed, total
wrist fusion will remain the only option for a destroyed RA
wrist with bony destruction and complete loss of the carpal
architecture.12
However, there are many debatable issues
Figure 3 Probability of implant survival in nonrheumatoid patients
(failure defined as revision).
Table 1 Clinical Results of TWA in 112 Wrists with At Least 2 Years of Follow-Up
Rheumatoid Nonrheumatoid Statistical Significance (p)
VAS pain improvement (100-point scale) 48 points 54 points ns
QuickDASH improvement 20 points 21 points ns
Wrist extension, degrees 29 (þ2) 36 (À4) ns
Wrist flexion, degrees 29 (À3) 37 (À5) ns
Ulnar deviation, degrees 24 (þ7) 28 (þ2) ns
Radial deviation, degrees 5 (À1) 10 (À4) 0.015
Grip strength improvement (% of preoperative value) 40 19 0.033
ns, not significant; TWA, total wrist arthroplasty; VAS, visual analog scale.
Figure 2 Probability of implant survival in rheumatoid patients
(failure defined as revision).
Journal of Wrist Surgery
TWA: Prospective Multicenter Study Herzberg et al.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-86-320.jpg)

![88
Disclaimer
There was no conflict of interests from any of the authors
of this article.
References
1 Trail IA, Stanley JK. Total wrist arthroplasty. In: Gelberman RH, ed.
The Wrist. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins;
2010:457–471
2 Krukhaug Y, Lie SA, Havelin LI, Furnes O, Hove LM. Results of 189
wrist replacements. A report from the Norwegian Arthroplasty
Register. Acta Orthop 2011;82(4):405–409
3 Rizzo M, Ackerman DB, Rodrigues RL, Beckenbaugh RD. Wrist
arthrodesis as a salvage procedure for failed implant arthroplasty. J
Hand Surg Eur Vol 2011;36(1):29–33
4 Harlingen D, Heesterbeek PJC, J de Vos M. High rate of complica-
tions and radiographic loosening of the biaxial total wrist arthro-
plasty in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years.
Acta Orthop 2011;82(6):721–726
5 Cavaliere CM, Chung KC. A systematic review of total wrist
arthroplasty compared with total wrist arthrodesis for rheuma-
toid arthritis. Plast Reconstr Surg 2008;122(3):813–825
6 Ferreres A, Lluch A, Del Valle M. Universal total wrist arthroplasty:
midterm follow-up study. J Hand Surg Am 2011;36(6):
967–973
7 Herzberg G. Prospective study of a new total wrist arthroplasty:
short term results. Chir Main 2011;30(1):20–25
8 Ward CM, Kuhl T, Adams BD. Five to ten-year outcomes of the
Universal wrist arthroplasty in patients with rheumatoid arthritis.
J Bone Joint Surg Am 2011;93(10):914–919
9 Takwale VJ, Trail IA, Stanley JK. Biaxial total wrist replacements in
patients with rheumatoid arthritis. J Bone Joint Surg Br 2002;84
(5):692–699
10 Radmer S, Andresen R, Sparmann M. Wrist arthroplasty with a
new generation of prostheses in patients with rheumatoid arthri-
tis. J Hand Surg Am 1999;24(5):935–943
11 Radmer S, Andresen R, Sparmann M. Total wrist arthroplasty in
patients with rheumatoid arthritis. J Hand Surg Am 2003;28
(5):789–794
12 Herren DB, Simmen BR. Limited and complete fusion of the
rheumatoid wrist. J Am Soc Surg Hand 2002;2:21–32
13 Herzberg G. Management of bilateral advanced rheumatoid wrist
destruction. J Hand Surg Am 2008;33(7):1192–1195
14 Adams BD, Grosland NM, Murphy DM, McCullough M. Impact of
impaired wrist motion on hand and upper-extremity performance
(1). J Hand Surg Am 2003;28(6):898–903
15 De Smet L, Truyen J. Arthrodesis of the wrist for osteoarthritis:
outcome with a minimum follow-up of 4 years. J Hand Surg [Br]
2003;28(6):575–577
16 Meads BM, Scougall PJ, Hargreaves IC. Wrist arthrodesis using a
Synthes wrist fusion plate. J Hand Surg [Br] 2003;28(6):571–574
17 Barbier O, Saels P, Rombouts JJ, Thonnard JL. Long-term functional
results of wrist arthrodesis in rheumatoid arthritis. J Hand Surg
[Br] 1999;24(1):27–31
18 Trieb K. Treatment of the wrist in rheumatoid arthritis. J Hand Surg
Am 2008;33(1):113–123
19 Adey L, Ring D, Jupiter JB. Health status after total wrist arthrodesis
for posttraumatic arthritis. J Hand Surg Am 2005;30(5):932–936
20 Sauerbier M, Kluge S, Bickert B, Germann G. Subjective and
objective outcomes after total wrist arthrodesis in patients with
radiocarpal arthrosis or Kienböck’s disease. Chir Main 2000;19
(4):223–231
21 Palmer AK, Werner FW, Murphy D, Glisson R. Functional wrist
motion: a biomechanical study. J Hand Surg Am 1985;10(1):39–46
22 Cobb TK, Beckenbaugh RD. Biaxial total wrist arthroplasty. J Hand
Surg Am 1996;21(6):1011–1021
23 Meuli HC. Total wrist arthroplasty. Experience with a nonce-
mented wrist prosthesis. Clin Orthop Relat Res 1997;(342):77–83
Journal of Wrist Surgery
TWA: Prospective Multicenter Study Herzberg et al.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-88-320.jpg)

![90
conversion to fusion was necessary. Moreover, fixation of
the distal component in the metacarpals was another
severe problem with these designs, often leading to subsi-
dence through the dorsal metacarpal cortices.4–6
The last
generation requires less bone resection and avoids meta-
carpal fixation,1,7
which could imply better and more
durable results. However, clinical documentation remains
modest because of limited numbers of patients or short
follow up.8–10
This is especially true in the case of wrists
with severe posttraumatic joint destruction. Carpal desta-
bilization after longstanding scaphoid nonunion (scaphoid
nonunion advanced collapse [SNAC] wrists), scapholunate
dissociation (scapholunate advanced collapse [SLAC]
wrists), or sequel of intraarticular distal radius fractures
is usually treated with partial or total fusion, and the
possibility of treating the advanced stages of these con-
ditions with TWA have not been investigated on a larger
scale. One recent study has demonstrated that results after
TWA in nonrheumatoid cases are comparable to those
obtained in rheumatoid arthritis,11
but without specific
data on posttraumatic cases, and thus the potential of TWA
in posttraumatic cases remains to be evaluated.
The purpose of this study was to report the results of a
multicenter series using one last-generation TWA in post-
traumatic cases. The questions to be answered were primarily
how TWA performs in patients with severe posttraumatic
wrist problems in terms of (1) patient-related outcome
measures, (2) objective measures, (3) radiological findings,
and (4) longevity of the implants.
Methods
The Re-Motion Total Wrist implant (Small Bone Innovation,
Morristown, PA) has a ball-and-socket design with a radial
and a carpal chromium-cobalt component that are titanium
coated. There is an intercalated polyethylene component
that primarily articulates with the radial component
but also has some articulation with the carpal plate
(►Fig. 1). The carpal plate is fixated to the carpus by its
stem and two screws, of which only the most radial
normally may penetrate the metacarpal for a very short
distance (►Fig. 2). Typically the procedure is done without
using cement.
In 2009 we created a web-based registry in which sur-
geons using the Re-Motion Total Wrist could enter prospec-
tively collected data. Seven participating centers that
contributed with at least 15 consecutive cases and regular
follow-up examinations were selected, and the data they had
entered in the registry were analyzed: preoperative data on
the etiology of wrist destruction, pain (0–100 on a visual
analogue scale [VAS]), function (0–100 according to the
QuickDASH questionnaire), active wrist motion, forearm
rotation and grip strength (with the JAMAR Dynamometer),
data concerning the operative procedure and complications,
Fig. 1 The Re-motion Total Wrist.
Fig. 2 X-ray view of the Re-motion Total Wrist (frontal view).
Journal of Wrist Surgery Vol. 2 No. 4/2013
Can TWA Be an Option in the Treatment of a Destroyed Wrist? Boeckstyns et al. 325
Downloadedby:MichelBoeckstyns.Copyrightedmaterial.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-90-320.jpg)
![91
and data from the clinical follow-up examinations, performed
at 6 weeks, 6 months, and 1 year after the arthroplasty and
thereafter yearly without upper limit. The evaluation of the
surgeons regarding the position of the implants and the
presence of osteolysis, with or without loosening, made at
the annual postoperative follow-up examinations was noted,
loosening being assessed in terms of angulation or subsidence
on serial radiographs (posteroanterior [PA] and lateral views).
In the present study, only cases with a posttraumatic diagno-
sis were included, and only cases with minimum 2 years of
follow-up. Revision cases were excluded.
Statistics
Kaplan-Meier survival analysis was used to estimate the
cumulative probability of remaining free of revision (i.e.,
reoperation with total or partial removal of the implants).
A nonparametric Wilcoxon signed-rank test was used for data
not normally distributed (QuickDASH scores), and the
parametric Student’s t-test was used for normally distributed
data (range of motion, grip strength, and VAS scores). Signifi-
cance was set at a P-value of less than 0.05.
Results
At the time, when this analysis was performed, the seven
participating centers had included 253 cases. Of these, 54
were posttraumatic cases, and 35 of them had a follow-up
period of minimum 2 years. Our follow-up analysis is based
on these 35 cases, the demographics of which are listed
in ►Table 1. In all cases, the extent of joint destruction was
considered to exclude the possibility of performing partial
wrist fusion. The revision rate and the implant survival curve,
however, were calculated on the basis of all 54 cases in order
not to exclude possible early revisions.
The following complications were encountered: one case
of reflex sympathetic dystrophy and one case of carpal tunnel
syndrome. Mean follow-up time was 39 (24–96) months.
In ►Table 2, the clinical data before operation and at the latest
performed follow-up are shown.
Patient-Related Outcome Measures
There was an improvement of 42 points in VAS score (highly
significant) and of 14 points in QuickDASH-score (not
significant).
Objective Outcome Measures
Grip strength improved slightly (not significant). Motion was
not different at follow-up, except for improved rotation (not
significant) (►Table 2). This was not only the case for the
mean values, but also for the individual patients, There was a
direct correlation between preoperative motion and motion
at follow-up.
Radiological Findings
At final follow-up no signs of loosening (angulation, subsi-
dence, or any other change in position of the implants) were
reported. Some degree of osteolysis without loosening of the
implants was reported in six cases.
Longevity of the Implants
Two cases were revised. The total revision rate was thus 3.7%,
calculated as the percentage of all the 54 posttraumatic
wrists. One case was revised two and a half years after
operation due to malposition of the implants, causing painful
impingement. At revision all components were found solidly
fixated. The components were exchanged, but the radius had
to be decorticated widely, and fixation of the new radial
component failed. Ultimately the wrist was fused successful-
ly. In the other case the carpal component loosened and was
Table 1 Demographics
Age (mean and range) 63 (33–81) years
Gender (men/women) 17/18
Side (dominant/nondominant) 18/16
1 NA
Follow-up (mean and range) 3 (2–8)
Diagnosis 22 SNAC/SLAC
11 malunited distal
radius fractures
2 carpal fracture-
dislocations
Table 2 Clinical results at latest follow-up compared with
preoperative values
Mean values
and range
Significance
Pain (VAS 0–100)
Preoperative
Postoperative
65 (35–100)
23 (0–82)
p ¼ 0.0000018
Function
(QuickDASH 0–100)
Preoperative
Postoperative
47 (12–79)
33 (0–77)
p ¼ 0.33
Grip strength (kg)
Preoperative
Postoperative
18 (2–42)
22 (2–43)
p ¼ 0.29
Motion (degrees)
Extension
Preoperative
Postoperative
Flexion
Preoperative
Postoperative
Radial flexion
Preoperative
Postoperative
Ulnar flexion
Preoperative
Postoperative
Pronation
Preoperative
Postoperative
Supination
Preoperative
Postoperative
37 (0–70)
34 (0–80)
36 (0–70)
33 (0–80)
12 (0–35)
9 (0–25)
19 (0–52)
22 (0–46)
77 (30–90)
82 (60–90)
74 (10–90)
79 (45–90)
p ¼ 0.43
p ¼ 0.56
p ¼ 0.37
p ¼ 0.33
p ¼ 0.21
p ¼ 0.15
Journal of Wrist Surgery Vol. 2 No. 4/2013
Can TWA Be an Option in the Treatment of a Destroyed Wrist? Boeckstyns et al.326
Downloadedby:MichelBoeckstyns.Copyrightedmaterial.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-91-320.jpg)

![93
chosen to conduct the registry. Nevertheless, we believe that a
sufficient range of criteria has been selected to permit valid
conclusions.
We consider the Kaplan-Meier method for the analysis
of implant survival as a powerful tool in the evaluation of
the durability of TWA. The method makes it possible to
analyze data from patients with different lengths of follow-
up, taking into account dropouts for any reason.28
It has
been used for evaluation of implants in the hand and wrist
for many years.6,8,17,29
A disadvantage is the fundamental
assumption that patients who are lost to follow-up and
patients who have died have the same failure rate as those
who comply with regular follow-up examinations, which is
not necessarily true. However, there were no dropouts in
our series.
The most widely accepted and commonly used defini-
tion of failure in implant survival analysis is revision
(removal of implants). This endpoint has been criticized
because the criteria used to decide the need for removal
may vary between patients and surgeons, and sometimes it
is argued that other definitions should be considered. These
could be severe pain or the presence of radiolucency or
subsidence combined with moderate or severe pain. Yet
other definitions can be considered, but as yet there exist
no clear indicators of early loosening of TWA (i.e., before
subsidence is evident on plain radiographs) that can be
used for routine purposes, and it will remain difficult to
compare survival analyses until consensus is reached about
which other outcome measures should be used rather than
revision. In our study the decision to revise implants is
based on the judgment of several surgeons or units that
work independently, which is an advantage compared with
studies in which the decision is made by a single surgeon
and solely dependent on this person’s views. We have
demonstrated a favorable survival rate for the Re-Motion
TWA in posttraumatic diagnoses at 4–8 years, with some
revisions during the early years. This finding must be
interpreted correctly: The survival rate at the “tail” of the
curve is less reliable because of the small number of
patients with long follow-up, and it must be expected
that the incidence of revision will increase as the implants
inevitably wear out, which also is indicated by the number
of implants with signs of loosening at follow-up in this
study. For this reason we prefer to conclude cautiously that
the implant survival was 90% at four years and not to
make any assumptions beyond that.
It is not the intention of this article to advocate for the
general use of TWA for painful posttraumatic wrist de-
struction but merely, for the sake of general scientific
information, to report on the results we have obtained. In
many cases, partial wrist fusion or selective denervation
certainly remains the first-choice solution; if those ap-
proaches are not feasible, total wrist fusion also remains
an option.
Conflict of Interest
None
References
1 Divelbiss BJ, Sollerman C, Adams BD. Early results of the Universal
total wrist arthroplasty in rheumatoid arthritis. J Hand Surg Am
2002;27(2):195–204
2 Lundkvist L, Barfred T. Total wrist arthroplasty. Experience with
Swanson flexible silicone implants, 1982-1988. Scand J Plast
Reconstr Surg Hand Surg 1992;26(1):97–100
3 Jolly SL, Ferlic DC, Clayton ML, Dennis DA, Stringer EA. Swanson
silicone arthroplasty of the wrist in rheumatoid arthritis: a long-
term follow-up. J Hand Surg Am 1992;17(1):142–149
4 Dennis DA, Ferlic DC, Clayton ML. Volz total wrist arthroplasty in
rheumatoid arthritis: a long-term review. J Hand Surg Am 1986;
11(4):483–490
5 Meuli HC, Fernandez DL. Uncemented total wrist arthroplasty. J
Hand Surg Am 1995;20(1):115–122
6 van Harlingen D, Heesterbeek PJ, J de Vos M. High rate of compli-
cations and radiographic loosening of the biaxial total wrist
arthroplasty in rheumatoid arthritis: 32 wrists followed for 6
(5–8) years. Acta Orthop 2011;82(6):721–726
7 Menon J. Universal Total Wrist Implant: experience with a carpal
component fixed with three screws. J Arthroplasty 1998;13(5):
515–523
8 Ward CM, Kuhl T, Adams BD. Five to ten-year outcomes of the
Universal total wrist arthroplasty in patients with rheumatoid
arthritis. J Bone Joint Surg Am 2011;93(10):914–919
9 Ferreres A, Lluch A, Del Valle M. Universal total wrist arthro-
plasty: midterm follow-up study. J Hand Surg Am 2011;36(6):
967–973
10 Herzberg G. Prospective study of a new total wrist arthroplasty:
short term results. Chir Main 2011;30(1):20–25
11 Herzberg G, Boeckstyns M, Ibsen Sørensen A, et al. “ReMotion”
total wrist arthroplasty: preliminary results of a prospective
international multicenter study of 215 cases. J Wrist Surg 2012;
01:17–22
12 Murphy DM, Khoury JG, Imbriglia JE, Adams BD. Comparison of
arthroplasty and arthrodesis for the rheumatoid wrist. J Hand Surg
Am 2003;28(4):570–576
13 Cavaliere CM, Chung KC. A systematic review of total
wrist arthroplasty compared with total wrist arthrodesis
for rheumatoid arthritis. Plast Reconstr Surg 2008;122(3):
813–825
14 Sauerbier M, Kluge S, Bickert B, Germann G. Subjective and
objective outcomes after total wrist arthrodesis in patients with
radiocarpal arthrosis or Kienböck’s disease. Chir Main 2000;19(4):
223–231
15 Adey L, Ring D, Jupiter JB. Health status after total wrist arthrode-
sis for posttraumatic arthritis. J Hand Surg Am 2005;30(5):
932–936
16 Kretschmer F, Fansa H. BIAX total wrist arthroplasty: management
and results after 42 patients [in German]. Handchir Mikrochir Plast
Chir 2007;39(4):238–248
17 Levadoux M, Legré R. Total wrist arthroplasty with Destot pros-
theses in patients with posttraumatic arthritis. J Hand Surg Am
2003;28(3):405–413
18 Nydick JA, Greenberg SM, Stone JD, Williams B, Polikandriotis JA,
Hess AV. Clinical outcomes of total wrist arthroplasty. J Hand Surg
Am 2012;37(8):1580–1584
19 Reigstad O, Lütken T, Grimsgaard C, Bolstad B, Thorkildsen R,
Røkkum M. Promising one- to six-year results with the Motec
wrist arthroplasty in patients with post-traumatic osteoarthritis. J
Bone Joint Surg Br 2012;94(11):1540–1545
20 Reigstad A, Mjørud J. Results of 189 wrist replacements. Acta
Orthop 2012;83(1):101, author reply 101–102
21 Bellemère P, Maes-Clavier C, Loubersac T, Gaisne E, Kerjean Y.
Amandys(®) implant: novel pyrocarbon arthroplasty for the wrist.
Chir Main 2012;31(4):176–187
Journal of Wrist Surgery Vol. 2 No. 4/2013
Can TWA Be an Option in the Treatment of a Destroyed Wrist? Boeckstyns et al.328
Downloadedby:MichelBoeckstyns.Copyrightedmaterial.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-93-320.jpg)











![105
Acknowledgment
We would like to acknowledge Dr. Marion Burnier, Lyon,
for her assistance with the radiologic evaluation.
Conflict of Interest
None
References
1 Zhu YH, Chiu KY, Tang WM. Review Article: Polyethylene wear and
osteolysis in total hip arthroplasty. J Orthop Surg (Hong Kong)
2001;9(1):91–99
2 Orishimo KF, Claus AM, Sychterz CJ, Engh CA. Relationship be-
tween polyethylene wear and osteolysis in hips with a second-
generation porous-coated cementless cup after seven years of
follow-up. J Bone Joint Surg Am 2003;85-A(6):1095–1099
3 Oparaugo PC, Clarke IC, Malchau H, Herberts P. Correlation of wear
debris-induced osteolysis and revision with volumetric wear-rates
of polyethylene: a survey of 8 reports in the literature. Acta Orthop
Scand 2001;72(1):22–28
4 McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG,
Charron KD. Wear rate of highly cross-linked polyethylene in total
hip arthroplasty. A randomized controlled trial. J Bone Joint Surg
Am 2009;91(4):773–782
5 Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear
and osteolysis outcomes for first-generation highly crosslinked
polyethylene. Clin Orthop Relat Res 2011;469(8):2262–2277
6 Goosen JHM, Castelein RM, Verheyen CCPM. Silent osteolysis asso-
ciated with an uncemented acetabular component: A monitoring
and treatment algorithm. Curr Orthop 2005;19:288–293
7 Boeckstyns ME, Herzberg G, Merser S. Favorable results after total
wrist arthroplasty: 65 wrists in 60 patients followed for 5–9 years.
Acta Orthop 2013;84(4):415–419
8 Radmer S, Andresen R, Sparmann M. Total wrist arthroplasty in
patients with rheumatoid arthritis. J Hand Surg Am 2003;28(5):
789–794
9 Lirette R, Kinnard P. Biaxial total wrist arthroplasty in rheumatoid
arthritis. Can J Surg 1995;38(1):51–53
10 Stegeman M, Rijnberg WJ, van Loon CJ. Biaxial total wrist arthro-
plasty in rheumatoid arthritis. Satisfactory functional results.
Rheumatol Int 2005;25(3):191–194
11 Courtman NH, Sochart DH, Trail IA, Stanley JK. Biaxial wrist
replacement. Initial results in the rheumatoid patient. J Hand
Surg [Br] 1999;24(1):32–34
12 Harlingen Dv, Heesterbeek PJ, J de Vos MHigh rate of complications
and radiographic loosening of the biaxial total wrist arthroplasty
in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years. Acta
Orthop 2011;82(6):721–726
13 Kretschmer F, Fansa H. BIAX total wrist arthroplasty: management
and results after 42 patients [in German]. Handchir Mikrochir Plast
Chir 2007;39(4):238–248
14 Rizzo M, Beckenbaugh RD. Results of biaxial total wrist arthro-
plasty with a modified (long) metacarpal stem. J Hand Surg Am
2003;28(4):577–584
15 Fourastier J, Le Breton L, Alnot Y, Langlais F, Condamine JL, Pidhorz
L. Guépar’s total radio-carpal prosthesis in the surgery of the
rheumatoid wrist. Apropos of 72 cases reviewed [in French]. Rev
Chir Orthop Repar Appar Mot 1996;82(2):108–115
16 Reigstad O, Lütken T, Grimsgaard C, Bolstad B, Thorkildsen R,
Røkkum M. Promising one- to six-year results with the Motec
wrist arthroplasty in patients with post-traumatic osteoarthritis. J
Bone Joint Surg Br 2012;94(11):1540–1545
17 Bidwai AS, Cashin F, Richards A, Brown DJ. Short to medium results
using the Remotion total wrist replacement for rheumatoid ar-
thritis. Hand Surg 2013;18(2):175–178
18 Herzberg G, Boeckstyns M, Sorensen AI, et al. “Remotion” total
wrist arthroplasty: preliminary results of a prospective interna-
tional multicenter study of 215 cases. J Wrist Surg 2012;1(1):
17–22
19 Rahimtoola ZO, Rozing PM. Preliminary results of total wrist
arthroplasty using the RWS Prosthesis. J Hand Surg [Br] 2003;
28(1):54–60
20 Rahimtoola ZO, Hubach P. Total modular wrist prosthesis: a new
design. Scand J Plast Reconstr Surg Hand Surg 2004;38(3):
160–165
21 Ward CM, Kuhl T, Adams BD. Five to ten-year outcomes of the
Universal total wrist arthroplasty in patients with rheumatoid
arthritis. J Bone Joint Surg Am 2011;93(10):914–919
22 Ferreres A, Lluch A, Del Valle M. Universal total wrist arthro-
plasty: midterm follow-up study. J Hand Surg Am 2011;36(6):
967–973
23 Gellman H, Hontas R, Brumfield RH Jr, Tozzi J, Conaty JP. Total wrist
arthroplasty in rheumatoid arthritis. A long-term clinical review.
Clin Orthop Relat Res 1997;(342):71–76
24 Bosco JA III, Bynum DK, Bowers WH. Long-term outcome of Volz
total wrist arthroplasties. J Arthroplasty 1994;9(1):25–31
25 Cobb TK, Beckenbaugh RD. Biaxial total-wrist arthroplasty. J Hand
Surg Am 1996;21(6):1011–1021
26 Groot D, Gosens T, Leeuwen NC, Rhee MV, Teepen HJ. Wear-
induced osteolysis and synovial swelling in a patient with a
metal-polyethylene wrist prosthesis. J Hand Surg Am 2006;
31(10):1615–1618
27 Herzberg G. Periprosthetic bone resorption and sigmoid notch
erosion around ulnar head implants: a concern? Hand Clin 2010;
26(4):573–577
28 van Schoonhoven J, Fernandez DL, Bowers WH, Herbert TJ. Salvage
of failed resection arthroplasties of the distal radioulnar joint
using a new ulnar head prosthesis. J Hand Surg Am 2000;25(3):
438–446
Journal of Wrist Surgery Vol. 3 No. 2/2014
Total Wrist Arthroplasty: Osteolysis Boeckstyns, Herzberg106
Thisdocumentwasdownloadedforpersonaluseonly.Unauthorizeddistributionisstrictlyprohibited.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-105-320.jpg)

![107
with the implant remaining steadily anchored in the
bone.3
Periprosthetic osteolysis with or without complete
loosening occurs in other joints as well and has been
frequently reported after total wrist arthroplasty
(TWA).8e13
Since 2003, we have been using the
Re-motion TWA (SBI, Inc, Morrisville, PA) as an
alternative to total wrist arthrodesis for the recon-
struction of severely destroyed and painful wrists.
This implant contains an articular component made of
conventional polyethylene that articulates with a
metallic CreCo component.
Our hypothesis was that the occurrence of poly-
ethylene debris in the interphase tissue between
prosthesis or cement and bone was correlated with
the degree of PPO. A secondary aim of the study was
to investigate the occurrence of metal particles in the
periprosthetic tissue, the level of Cr and Co ions in
the blood of patients, and the possible role of infec-
tious or rheumatoid activity in the development of
PPO.
MATERIALS AND METHODS
Ethics
The study conformed to the ethical guidelines of the
1975 Helsinki Declaration. The Scientific Ethical
Committee for the Capital Region in Denmark
approved the study (Study H-2-2013-032). We ob-
tained written informed consent from all patients.
Selection of patients
Re-motion TWA is an elliptical ball and socket
design consisting of radial and carpal CreCo com-
ponents that are titanium coated and an intercalated
polyethylene ball. It mainly articulates with the radial
component in an unconstrained link but also permits
a rotational articulation of 20
with the carpal plate. It
requires minimal bone resection and is designed to
act much like a surface replacement. The carpal plate
is fixated to the carpus by its stem and 2 screws. The
polyethylene in the carpal ball is of a conventional,
not highly cross-linked type. All patients in whom a
Re-motion TWA was implanted at Gentofte Hospital,
Denmark, between September 2003 and April 2010
(21 patients) were eligible for this study.
We excluded wrists that had been revised to a new
TWA or arthrodesis (3 patients), those who were
unable to participate for geographical reasons (2 pa-
tients), those who had not given informed consent
(1 patient), those with conditions that contraindicated
the surgical procedure (one patient: recent ipsilateral
shoulder fracture), and those who were already
included with the contralateral wrist (one patient).
Thus, 13 patients were included. Table 1 shows the
demographics. We obtained tissue samples from the
implantebone or implantecementebone interphase,
collected blood samples, obtained plain x-ray exam-
inations, and updated the clinical status in June 2013.
Surgical procedure
We used Bier block for anesthesia, made a 2- to 3-cm
straight incision in the existing dorsal surgical scar,
and approached the dorsal wrist capsule between the
third and fourth extensor compartments. Through
windows in the capsule we collected samples from the
soft tissue surrounding the implant for bacteriological
cultures. From the dorsal interphase area between the
radial component and the radius and from the inter-
phase area between the carpal plate and the carpus, we
collected tissue samples for histopathological exami-
nation. In one patient we also collected tissue under an
ulnar head component; but to avoid a potential con-
founding influence, we did not include this in the an-
alyses aimed at testing our hypothesis. We closed the
wound with resorbable sutures in the capsule and
nonresorbable sutures in the skin. Patients were
allowed to mobilize the wrist without delay.
Histopathological examination
After fixation in 10% buffered formaldehyde all tissue
samples were sectioned and embedded in paraffin.
Sections cut at 2 mm thickness were prepared, stained
with hematoxylineeosin, and examined by light and
polarized microscopy. The amount of foreign body
particles was graded semi-quantitatively from 0 to 3, in
which 0 represented no particles; 1, particles present
but hard to find; 2, no problem in identifying particles;
and 3, a marked amount of particles as seen on
TABLE 1. Demographics of the 13 Patients
Included
Age, y (mean [range]) 68 (53e87)
Sex 2 male, 11 female
Mean follow-up, y
(mean [range])
6 (3e10)
Diagnosis
Rheumatoid arthritis 6
Idiopathic osteoarthritis 4
Posttraumatic arthritis 3
Fixation technique 2 cemented, 11 not cemented*
*Cemented fixation was used when the bone was considered too
fragile to support uncemented implant components.
WEAR PARTICLES AND OSTEOLYSIS AFTER TOTAL WRIST ARTHROPLASTY 2397
J Hand Surg Am. r Vol. 39, December 2014](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-107-320.jpg)







![115
Paper
VII
VIDENSKAB 3333Ugeskr Læger 172/48 29. november 2010
ORIGINALARTIKEL
Håndkirurgisk Afsnit,
Ortopædkirurgisk
Afdeling,
Gentofte Hospital
Validering af spørgeskema
ved lidelser i overekstremiteten
Alex Herup, Søren Merser Michel Boeckstyns
RESUME
INTRODUKTION: Disability of the arm, shoulder and hand
(DASH) er et amerikansk udviklet spørgeskema, der kan an-
vendes på patienter med lidelser i overekstremiteten. Ud fra
besvarelsen af spørgeskemaet kan der udregnes en numerisk
DASH-score. Scoren kan anvendes som et udtryk for patientens
opfattelse af invalideringsgraden. DASH kan anvendes på pa-
tienter med alle former for lidelser i overekstremiteten og er
anvendelig både ved akutte og kroniske tilstande, hvad enten
de er opstået på traumatisk vis eller ej. I denne undersøgelse er
DASH anvendt på en gruppe danske patienter med forskellige
overekstremitetslidelser. Formålet var at vurdere reproducer-
barheden af de danske patienters DASH-scorer for at belyse,
om spørgeskemaet er anvendeligt i det kliniske arbejde med
danske patienter.
MATERIALE OG METODER: Der deltog i alt 83 patienter, hvoraf
73 havde håndrelaterede lidelser, og ti havde skuldergener. De
inkluderede patienter var alle i stabil sygdomsfase, typisk med
kronisk lidelse, og de blev spurgt, om de ville udfylde DASH-
spørgeskemaet i forbindelse med forundersøgelse inden op-
skrivning til operation eller ved afslutning af et behandlings-
forløb i ambulatoriet.
RESULTATER: Der var i alt 54 patienter, der opfyldte alle krav
vedrørende aflevering og besvarelse af DASH. DASH-scorene lå
numerisk tæt på hinanden med en Intra Class Coefficient på
0,85. Cronbachs alfa blev udregnet til 0,96, hvilket er udtryk for,
at de indgående deltest måler det samme. Spearmankoefficien-
ten var samlet 0,9, og første og anden besvarelse var stærkt
korrelerede.
KONKLUSION: Undersøgelsen viser god reproducerbarhed af
DASH, og scoringen er stabil og pålidelig og kan anvendes på
danske patienter.
DASH står for disability of the arm, shoulder and hand.
Spørgeskemaet er udviklet af The Insitute of Work and
Health, Toronto, Ontario, Canada og The American
Academy of Orthopaedic Surgeons [1]. Det indeholder
30 spørgsmål: 21 vedrørende evnen til at udføre
praktiske aktiviteter, seks vedrørende symptomer i
overekstremiteterne og tre vedrørende psykosociale
forhold. Endvidere er der inkluderet to valgfrie mo-
duler med fire spørgsmål i hver. Det ene modul hen-
vender sig til sportsfolk og udøvende kunstnere,
mens det andet er et arbejdsmodul for patienter på
arbejdsmarkedet. Disse valgfri moduler er ikke an-
vendt i denne undersøgelse. Der foreligger endvidere
en kort version af spørgeskemaet, Quick DASH.
Transkulturel adaptation (dvs. valideret oversæt-
telse) af DASH er udført til talrige sprog og kulturer:
I skrivende stund er 35 adapterede versioner god-
kendt, og seks er under udarbejdelse. Der er fastlagt
strenge krav til oversættelsesprocessen og godken-
delse af skemaet på nye sprog, hvilket varetages af
the Institute of Work and Health i Canada [1], som har
udviklet DASH og ejer rettighederne til spørgeske-
maet. I korthed omfatter processen først oversættel-
sen fra originalsproget til målsproget, og herefter
tilbageoversættelse til originalsproget og sammenlig-
ning af tilbageoversættelsen med den originale ver-
sion. I forløbet deltager forskellige grupper af både
medicinsk faglige personer og sprogfaglige personer.
Den danske oversættelse af DASH er blevet godkendt
i 2004. Den danske oversættelse er den eneste autori-
serede version, og modifikationer er ikke tilladt hver-
ken i indhold eller udformning, da selv små ændrin-
ger kan påvirke måleegenskaberne.
Spørgsmålene i spørgeskemaet skal besvares
med en værdi fra 1 til 5 (fra »ingen gene« til »værst
mulig gene«). Den samlede score beregnes som
[(summen af n svar/n)-1] × 25. En DASH-score må
ikke udregnes, hvis der er mere end tre ubesvarede
spørgsmål. Den højest mulige score (værste gene) er
således 100 og den laveste 0 (ingen gener).
Scoring af de valgfrie moduler gøres efter samme
formel, dog med det forbehold, at scoren ikke må ud-
regnes, hvis der mangler besvarelser.
DASH har vist sig at være velegnet til vurdering
af patienter med lidelser og symptomer fra overeks-
tremiteterne inden for ortopædkirurgien. Specielt an-
vendes DASH meget i håndkirurgien, og det bruges
internationalt på en bred og varieret patientgruppe.
Eksempelvis patienter med karpaltunnelsyndrom [2],
reumatoid artritis [3], distal radius-fraktur [4], flek-
sorseneskade [5], discus triangularis-skade [6],
osteoartrose i hånden [7], amputationsskader [8]
m.m. DASH anvendes i et mere begrænset omfang
inden for skulderkirurgi [9].
Der er ved tidligere undersøgelser fundet god
reproducerbarhed af scoringerne i originalsproget
[10, 11].](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-115-320.jpg)
![116
3334 VIDENSKAB Ugeskr Læger 172/48 29. november 2010
Formålet med denne undersøgelse var primært
at undersøge reproducerbarheden af DASH-spørge-
skemaet som et led i den transkulturelle adaptation
og sammenligne denne reproducerbarhed med origi-
nalversionen, sekundært at undersøge spørgeskema-
ets interne konsistens.
MATERIALE OG METODER
Indgangskriterierne var håndrelaterede eller skulder-
relaterede gener i stabil fase hos patienter, der var
henvist til forundersøgelse på Ortopædkirurgisk Af-
deling, Gentofte Hospital. Vi tilstræbte et materiale
af en størrelse og en fordeling af diagnosegrupperne,
der svarede til den originale amerikanske reproducer-
barhedsundersøgelse [10].
Ved forundersøgelsen blev patienterne bedt om
at udfylde spørgeskemaet uden nærmere information
om reproducerbarhedsundersøgelsen for at undgå,
at denne viden skulle påvirke deres senere besva-
relse. En uge efter forundersøgelsen fik patienterne
tilsendt et nyt spørgeskema, der nu indeholdt skriftlig
information om den pågående reproducerbarheds-
undersøgelse og anmodning om at indsende deres
besvarelse inden for en uge i en vedlagt frankeret
returkuvert. Besvarelserne blev indsamlet og data be-
arbejdet i et sekretariat, hvis medarbejdere ikke
havde direkte kontakt med patienterne.
Patienter som ikke ønskede at udfylde skema-
erne, udfyldte skemaerne mangelfuldt (dvs. mere
end tre ubesvarede spørgsmål) eller indsendte deres
svar mere end 31 dage efter forundersøgelsen, blev
ekskluderet.
STATISTIK
Da formålet med undersøgelsen ikke blot var at vur-
dere reproducerbarheden af DASH, men særligt at
undersøge om reproducerbarheden af den danske
version svarede til den originale version og andre
oversættelser, har vi valgt de samme statistiske test,
som blev anvendt i tidligere publikationer.
Beaton anvendte i sin originalpublikation Intra
Class Coefficient (ICC) model 2.1 [12], mens andre
har anvendt ICC model 1.1 [13]. Begge er korrela-
tionskoefficienter for kategoriske data, henholdsvis i
en tovejs- og en envejs ANOVA-analyse. Korrelations-
koefficienterne Pearson og Spearman er udtryk for
sammenhængen mellem første og anden DASH-
score. De indikerer således, om der er en høj første
score og en høj anden score, men er ikke nødvendig-
vis et udtryk for, om scorene rent numerisk er iden-
tiske. Vi mener, at Spearmanmodellen til test af data
på en rangordenskala er mest relevant i dette test/
retest studie, men vi har supplerende udregnet
Pearsons koefficient til sammenligning med andre
arbejder, hvor den anvendes [10].
Udregning af kappakoefficient fravalgte vi, da
den egentlige kappakoefficient er beregnet til nomi-
nelle skalaer og i øvrigt ikke er anvendt i de materia-
ler, vi ønskede at sammenligne os med.
Til evaluering af spørgeskemaets interne kon-
sistens har vi i lighed med andre [13-17] anvendt
Cronbachs alfa [18].
Alle statistiske beregninger og grafik er lavet
med open source-programmet R version 2.07, (R
Development Core Team (2008)). Der er anvendt
følgende R-packages:
Dataimport fra Microsoft Access-database med
RODBC (oprindeligt Michael Lapsley og fra oktober
2002 Brian D. Ripley (2008)). R til LATEX2e kode
med Hmisc (Harrell, Jr. (2007)) .Cronbachs alfa med
irr (Matthias Gamer samt Jim Lemon og Ian Fellows
(2007)).
RESULTATER
I alt indgik 83 patienter, hvoraf 73 patienter havde
håndrelateret gener og ti skulderrelaterede gener.
I alt 29 patienter blev sekundært ekskluderet: I otte
tilfælde var besvarelsen mangelfuld, 18 skemaer var
udfyldt senere end efter 31 dage, og tre angav ikke
datoen. Således omfattede korrelationsanalyserne
54 tilfælde.
Diagnosekategorier i undersøgelsen fremgår af
Tabel 1.
For så vidt angår de 54 patienter, hvor en score
kunne udregnes for begge besvarelser, var kun 30 ud
af 3.240 mulige spørgsmål (1%) ubesvarede. Det
hyppigst ubesvarede spørgsmål angik patienternes
Håndtrykskraft an-
vendes indimellem
som samlet mål for
håndfunktion.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-116-320.jpg)
![117
VIDENSKAB 3335Ugeskr Læger 172/48 29. november 2010
sexliv og udgjorde 20% af de ubesvarede spørgsmål.
De øvrige manglende svar var jævnt fordelt på de
øvrige spørgsmål.
Figur 1 viser den lineære korrelation mellem
DASH-scorene for skema 1 og skema 2.
For de 54 patienter, der indgik i de statistiske
beregninger, var ICC-værdierne 0,85, både ved an-
vendelse af envejs- og af tovejsanalysemodellen.
Pearson- og Spearmankoefficienterne var henholds-
vis på 0,89 og 0,90. Cronbachs alfa var på 0,96.
DISKUSSION
Reproducerbarheden af DASH-scoringerne i vores
undersøgelse havde en ICC-værdi på 0,85, både ved
anvendelse af en envejs- og en tovejsmodel.
Reproducerbarhed bedømmes som værende
»moderat god«, hvis ICC-værdierne er mellem 0,4 og
0,75 og »meget god« ved værdier over 0,75 [19].
Vores undersøgelsesresultat viser således »meget
god« overensstemmelse. Næsten identiske værdier er
fundet i andre arbejder [15, 16].
Nogle materialer angiver ICC-værdier, der ligger
noget højere end vores [14, 20]. Dette gælder også
originalmaterialet [10] med en værdi på 0,96. For-
skellen er dog ikke større, end at reproducerbarheden
i vores materiale må anses for at være af samme stør-
relsesorden som i den oprindelige DASH.
Den stærke korrelation bekræftes af Spearman-
og Pearsonkoefficienterne, som var næsten identiske
på 0,89 og 0,90, og de bekræfter således begge den
stærke korrelation. Cronbachs alfa angiver en meget
høj intern konsistens, der svarer til andre undersøgel-
ser [13-17]. Den jævne spredning af scorene, som
fremgår af Figur 1, viser endvidere, at spørgeskemaet
for det første har en god diskriminativ evne (evne til
at skelne patienter med få symptomer fra patienter
med flere symptomer) og for det andet, at reprodu-
cerbarheden ikke er afhængig af værdien af selve
scoren: Besvarelserne fra såvel patienter med lav
score som fra patienter med høj score var korrele-
rede. Endelig viser spredningen af scorene, at vores
materiale havde en bred fordeling og således repræ-
senterede et bredt symptomsværhedsspektrum.
Antallet af frafaldne respondenter i denne under-
søgelse er højt, men skal imidlertid vurderes på bag-
grund af undersøgelsens design, hvor der ikke forelå
en forhåndsaccept fra patienternes side, og hvor der
ingen direkte patientkontakt var ved anden besva-
relse. Det var således op til patienterne selv, om de
fandt det vigtigt at deltage og overholde tidsfristen.
Disse forhold var uundgåelige for at mindske biaspå-
virkningen mellem første og anden besvarelse, og vi
vurderer, at størrelsen af materialet – trods eksklusio-
nerne – er acceptabelt til vurdering af reproducerbar-
heden og sammenligningen med andre materialer.
Især finder vi det vigtigt, at kun 10% måtte eksklude-
res på grund af mangelfuld besvarelse. Det er tidli-
gere blevet diskuteret, hvorvidt spørgsmålet vedrø-
rende patienternes evne til at dyrke sex burde udgå,
men man har valgt at beholde spørgsmålet og dette
må respekteres for ikke at påvirke spørgeskemaets
validitet i forhold til udenlandske versioner, således
at sammenlignelighed er mulig. Set ud fra et repro-
ducerbarhedssynspunkt mener vi, at den danske
oversættelse af DASH er korrekt, idet reproducerbar-
heden af den danske oversættelse er god ved sam-
menligning med den oprindelige version.
Hvad angår intervallets længde mellem første og
anden besvarelse har vi på forhånd valgt 31 dage som
maksimum for at mindske risikoen for variationer,
der kan tilskrives reelle ændringer i selve sygdom-
mens forløb. Tidligere er det dog påvist, at det ikke er
af afgørende betydning, om der er et kort eller langt
tidsinterval mellem test/retest-tidspunkterne for
DASH [14], og dette kan vores undersøgelse be-
Diagnose Antal
Dupuytrens kontraktur 22
Artrose i 1. fingers rodled 17
Andre håndrelaterede sygdomme 34
Skulderlidelser 10
Diagnoseliste
TABEL 1
80
60
40
20
0
0 20 40 60
DASH-score, skema 1
80
Patienter, der opfyldte alle kriterier.
Øvrige patienter.
DASH-score, skema 2Den lineære korrelation
mellem DASH-scorerne
for skema 1 og skema 2.
DASH = disability of the
arm, shoulder and hand.
FIGUR 1](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-117-320.jpg)
![118
3336 VIDENSKAB Ugeskr Læger 172/48 29. november 2010
kræfte, idet vi fandt ICC-værdier på 0,85 for den en-
delige gruppe på 54 patienter og en ICC-værdi på
0,87, når også de tilfælde inkluderes, hvor tidsfristen
blev overskredet.
KONKLUSION
Vores udregninger bekræfter, at der er god overens-
stemmelse mellem patienternes scoring ved første og
anden besvarelse af DASH-spørgeskemaet, og at
overensstemmelsen er af samme størrelsesorden, som
den der blev opnået i den originale version, hvilket
bekræfter den transkulturelle adaptations validitet.
Desuden påvises en god intern konsistens i spør-
geskemaet.
Overordnet viser DASH-scoren sig derfor som
stabil, valid og derfor velegnet til evaluering både i
klinikken og i videnskabelige undersøgelser.
KORRESPONDANCE: Alex Herup, Hvedevej 6, 2765 Smørum.
E-mail: al.herup@sport.dk
ANTAGET: 23. januar 2010
FØRST PÅ NETTET: 14. juni 2010
INTERESSEKONFLIKTER: Ingen
LITTERATUR
1. Solay S, Beaton DE, McConnell S et al. DASH outcome measure user’s manual.
2. ed. Toronto: Institute for Work Health, 2002.
2. Hobby JL, Watts C, Elliot D. Validity and responsiveness of the patient evalua-
tion measure as an outcome measure for carpal tunnel syndrome. J Hand Surg
(Br) 2005;30:350-4.
3. Chiari-Grisar C, Koller U, Stamm TA et al. Performance of the disabilities of the
arm, shoulder and hand outcome questionnaire and the Moberg picking up
test in patients with finger joint arthroplasty. Arch Phys Med Rehabil
2006;87:203-6.
4. Keller M, Steiger R. [Open reduction and internal fixation of distal radius exten-
sion fractures in women over 60 years of age with the dorsal radius plate (pi-
plate)]. Handchir Mikrochir Plast Chir 2006;38:82-9.
5. Su BW, Solomons M, Barrow A et al. Device for zone-II flexor tendon repair. A
multicenter, randomized, blinded, clinical trial. J Bone Joint Surg Am
2005;87:923-35.
6. Ruch DS, Papadonikolakis A. Arthroscopically assisted repair of peripheral trian-
gular fibrocartilage complex tears: factors affecting outcome. Arthroscopy
2005;21:1126-30.
7. De Smet L. Responsiveness of the DASH score in surgically treated basal joint
arthritis of the thumb: preliminary results. Clin Rheumatol 2004;23:223-4.
8. Davidson J. A comparison of upper limb amputees and patients with upper
limb injuries using the Disability of the Arm, Shoulder and Hand (DASH). Disabil
Rehabil 2004;26:917-23.
9. Bengtsson M, Lunsjo K, Hermodsson Y et al. High patient satisfaction after
arthroscopic subacromial decompression for shoulder impingement: a prospec-
tive study of 50 patients. Acta Orthop 2006;77:138-42.
10. Beaton DE, Katz JN, Fossel AH et al. Measuring the whole or the parts? Validity,
reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand
outcome measure in different regions of the upper extremity. J Hand Ther
2001;14:128-46.
11. Turchin DC, Beaton DE, Richards RR. Validity of observer-based aggregate sco-
ring systems as descriptors of elbow pain, function, and disability. J Bone Joint
Surg Am 1998;80:154-62.
12. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability.
Psychol Bull 1979;86:420-8.
13. Lee EW, Lau JS, Chung MM et al. Evaluation of the Chinese version of the Dis-
ability of the Arm, Shoulder and Hand (DASH-HKPWH): cross-cultural adapta-
tion process, internal consistency and reliability study. J Hand Ther
2004;17:417-23.
14. Atroshi I, Gummesson C, Andersson B et al. The disabilities of the arm, shoulder
and hand (DASH) outcome questionnaire: reliability and validity of the Swedish
version evaluated in 176 patients. Acta Orthop Scand 2000;71:613-8.
15. Imaeda T, Toh S, Nakao Y et al. Validation of the Japanese Society for Surgery
of the Hand version of the Disability of the Arm, Shoulder, and Hand question-
naire. J Orthop Sci 2005;10:353-9.
16. Padua R, Padua L, Ceccarelli E et al. Italian version of the Disability of the Arm,
Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and valid-
ation. J Hand Surg (Br) 2003;28:179-86.
17. Themistocleous GS, Goudelis G, Kyrou I et al. Translation into Greek, cross-
cultural adaptation and validation of the Disabilities of the Arm, Shoulder, and
Hand Questionnaire (DASH). J Hand Ther 2006;19:350-7.
18. Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika
1951;16:297-334.
19. Rankin G, Stokes M. Reliability of assessment tools in rehabilitation: an illustra-
tion of appropriate statistical analyses. Clin Rehabil 1998;12:187-99.
20. Orfale AG, Araujo PM, Ferraz MB et al. Translation into Brazilian Portuguese,
cultural adaptation and evaluation of the reliability of the Disabilities of the
Arm, Shoulder and Hand Questionnaire. Braz J Med Biol Res 2005;38:293-
302.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-118-320.jpg)
![119
Paper
VIII
DANISH MEDICAL JOURNAL
ABSTRACT
INTRODUCTION: Patient-rated outcome measures are fre-
quently used to assess the results of total wrist arthro-
plasty, but their psychometric properties have not yet been
evaluated in this group of patients. The purpose of our
study was to assess the psychometric properties of the Dan-
ish Quick Disabilites of Arm Shoulder and Hand (QuickDASH)
and Patient-rated Wrist Evaluation questionnaires in pa-
tients with total wrist arthroplasty.
MATERIAL AND METHODS: In a prospective cohort of 102
cases, we evaluated the QuickDASH. Furthermore, in a
cross-sectional study and a test-retest on a subgroup of the
patients, we evaluated the Patient-rated Wrist Evaluation.
RESULTS: Internal consistency and reproducibility were very
high (Cronbach’s alpha 0.96/0.97; Spearman’s rho 0.90/
0.91; intraclass coefficient 0.91/0.92), and there were no
floor or ceiling effects. The responsiveness of the Quick-
DASH was high (standardised response mean 1.06 and ef-
fect size 1.07). The construct validity of both scales was
confirmed by three a priori formulated hypotheses: a mod-
erate, negative correlation of scores with grip-strength;
a moderate, positive correlation with pain and a very weak
or no correlation with mobility. Rheumatoid patients scored
significantly higher on the QuickDASH than other patients
did. The scores of both questionnaires were very closely
related.
CONCLUSION: Both questionnaires are valid and equivalent
for use in patients with total wrist arthroplasty.
FUNDING: This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit
sectors.
TRIAL REGISTRATION: not relevant.
The QuickDASH questionnaire was developed by extract-
ing 11 of 30 items from the original DASH questionnaire.
It aims at measuring function, disability and symptoms
in persons with disorders of the upper limb with a short
patient-rated outcome instrument [1]. In a systematic
review, Kennedy et al identified studies validating the
original English version and cultural adaptations [2]. The
diagnostic groups in these studies vary widely. In one
study only, patients with upper limb arthroplasties were
included, but none of them had wrist arthroplasties [3].
The Patient-rated Wrist Evaluation questionnaire
(PRWE) [4] was originally designed as a specific instru-
ment for the assessment of distal radius fractures and
wrist injuries, but this questionnaire has not been vali-
dated in the specific context of wrist arthoplasty.
The purpose of our study was to assess and
compare the psychometric properties of the Danish
QuickDASH and PRWE in a group of patients with total
wrist arthroplasty (TWA) with regard to construct valid-
ity, reproducibility, internal consistency, responsiveness
and floor/ceiling effects.
MATERIAL AND METHODS
Study populations
In Group 1, we included consecutive patients operated
with a third generation TWA at Gentofte Hospital or at
Rigshospitalet, Denmark, during the 1999-2013 period.
We evaluated the patients with the DASH or QuickDASH
questionnaires: eight Universal (Integra Life Sciences
Corp., Plainsboro, NJ, USA) and 96 Remotion (SBI Inc.,
Morrisville, PA, USA). Two patients were excluded be-
cause they did not attend the 12-month follow-up exam-
ination. This group (102 patients) was used for the as-
sessment of the construct validity, internal consistency,
floor/ceiling effects and responsiveness of the Quick-
DASH (Figure 1).
Group 2 consisted of a subset of Group 1: we in-
cluded only the patients from Gentofte Hospital. This
group was used for the general assessment of the PRWE
and of the reproducibility of the QuickDASH (Figure 1).
There were 69 females and 33 males in Group 1,
and 41 females and 22 males in Group 2. The mean age
was 59.5 (29-83) years in Group 1 and 58.8 (31-83) in
Group 2. There were 57 rheumatoid patients versus 45
non-rheumatoid patients in Group 1 and 29 rheumatoid
versus 34 non-rheumatoid patients in Group 2.
Clinical design
In Group 1, we used data collected at the 12-month fol-
low-up after TWA to evaluate construct validity, internal
consistency, and floor/ceiling effects in a cross-sectional
study. The responsiveness of the QuickDASH was calcu-
lated in a prospective cohort study using data collected
preoperatively and at a 1-year follow-up.
Group 2 were entered into a cross-sectional study
to evaluate the PRWE and into a test-retest trial to
evaluate the reproducibility of both questionnaires. The
Psychometric properties of two questionnaires
in the context of total wrist arthroplasty
Michel E.H. Boeckstyns1
Søren Merser2
ORIGINAL
ARTICLE
1) Clinic for Hand
Surgery
2) Informatics
Statistical Consulting
Dan Med J
2014;61(11):A4939](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-119-320.jpg)
![120
DANISH MEDICAL JOURNAL
questionnaires were sent to the patients’ private ad-
dresses by surface mail with a request to return it within
a week and without informing them about the intention
to retest. Six days after reception of the answer, a sec-
ond questionnaire was sent in which we explained our
wish to assess its reproducibility. A total of 53 returned
the first questionnaire. One of these had insufficient an-
swers to calculate a QuickDASH score, and we did not
send her a second questionnaire. Four other patients did
not return the second questionnaire. Thus, we had 48
sets of responses for the test-retest. The mean interval
between the responses was 14.1 days (range: 6-29 days).
Instruments and measurements
The QuickDASH consists of six items concerning the abil-
ity to perform activities of daily living (ADL), two con-
cerning social and work ability, one concerning pain and
two concerning other symptoms. Each item has five re-
sponse options (scored 1-5) which are used to create a
summative score ranging from 0 (no disability or symp-
toms) to 100 (maximal disability or symptoms). If more
than one item is missing in the QuickDASH, a score can-
not be calculated
The PRWE consists of eight items concerning ADL,
two concerning social and work ability and five concern-
ing pain. They are grouped into two sections: pain and
function. Each item is rated on a Likert scale from 0 to
10 producing a summative score for each section. The
total wrist score is calculated by adding the function
score divided by two plus the pain score, and ranges
from zero (no disability or symptoms) to 100 (maximal
disability or symptoms). If an item is missing, it is re-
placed with the mean score of the subscale. Both ques-
tionnaires were translated into Danish according to the
Guillemin guidelines [5-7].
Reproducibility expresses to which extent scores
can be reproduced in a test-retest.
Construct validity indicates the correlation between
the measurements and theoretical considerations. To
assess construct validity, we formulated three hypoth-
eses a priori. Firstly, there should be a moderate, nega-
tive correlation between the scores and grip strength –
the latter being a good indicator of hand function – but
not a high correlation, considering the individual vari-
ance across patients related to their age, sex and body
size. Secondly, we postulated a moderate, positive cor-
relation with pain, because good function implies a low
degree of pain. However, we did not expect a very high
correlation since the questionnaire is not intended to
simply measure pain. Thirdly, we postulated a weak or
no correlation of the scales with wrist motion, knowing
that even fused wrists are consistent with acceptable
hand function.
For the testing of our hypotheses, we measured
grip strength with the JAMAR (Sammon Preston Inc.,
Bolingbrook, IL, USA). We used a visual analogue scale
(VAS) for evaluation of “general level of pain throughout
the day”. To express motion, we used the total dorsal/
palmar wrist motion which was measured with a
goniometer.
Floor and ceiling effects show the proportion of in-
dividuals who achieve the highest or lowest possible nu-
meric value of a score and are considered present when
more than 15% of the individuals achieve these values
[8]. A ceiling or floor effect indicates that the measure-
ment instrument cannot be used for the entire con-
tinuum of patients.
FIGURE 1
Flow chart illustrating how the two patient groups, treated at Rigshos-
pitalet and Gentofte Hospital were selected. In Group 1, two patients
had been excluded due to lack of response at the one-year follow-up.
In Group 2, the number of patients was reduced from 53 to 48 in the
test-retest trial due to lack of second response.
Rigshospitalet Gentofte Hospital
Assessment of PREW:
– Construct validity
– Internal consistency
– Floor-/ceiling effect
(n = 53)
Assessment of QuickDASH:
– Construct validity
– Internal consistency
– Floor-/ceiling effect
– Responsiveness
(n = 102)
Reproducibility of
PREW and QuickDash
(n = 48)
PRWE = Patient-rated Wrist Evaluation questionnaire.
QuickDASH = Quick Disabilities of Arm Shoulder and Hand questionnaire.
Cemented remotion
total wrist arthro-
plasty.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-120-320.jpg)
![121
DANISH MEDICAL JOURNAL
Internal consistency measures to which extent the
different items that propose to measure the same gen-
eral construct tend to produce similar scores, i.e.
whether there is general internal agreement between
the items.
Responsiveness is the ability of a scale to measure a
meaningful or important change in a clinical state, e.g.
how it responds to treatment.
Statistical analysis
Correlations for construct validity were evaluated with
Spearman’s rho, values ± 0.8 to ± 1.0 indicating a very
strong relationship, ± 0.6 to ± 0.8 a strong relationship,
± 0.4 to ± 0.6 a moderate relationship, ± 0.2 to ± 0.4 a
weak relationship,and ± 0.0 to ± 0.2 a very weak or no
relationship [9].
Internal consistency was assessed with Cronbach’s
alpha. Scales are considered to be internally consistent if
Cronbach’s alpha is between 0.7 and 0.9 [10]. Values
higher than 0.9 might indicate item redundancy.
Responsiveness was expressed with the standard-
ised response mean (SRM) and the effect size (ES) [11].
We considered values between 0 and 0.2 as “trivial”, be-
tween 0.2 and 0.5 as “small”, between 0.5 and 0.8 as
“moderate” and higher than 0.8 as “large”.
Reproducibility was expressed with Spearman’s rho
and the intraclass coefficient (ICC3) with the same inter-
val definitions as mentioned.
Rheumatoid patients typically have multiple joint
involvement to a higher extent than non-rheumatoid pa-
tients. We made separate analyses for these diagnostic
subgroups in order to evaluate any bias. To compare the
scores between rheumatoid and non-rheumatoid cases,
we used the Wilcoxon rank-sum test.
The level of significance was set at p 0.05.
Trial registration: not relevant.
RESULTS
For 17 of 308 testings (5.5%), the QuickDASH score could
not be calculated, whereas all of the 100 PRWE scores
could be calculated. Rheumatoid patients scored signifi-
cantly higher according to the QuickDASH in Group 1,
but not in Group 2. Table 1 shows the result of the test-
ing of the hypotheses for construct validity. Reprodu-
cibility, internal consistency and responsiveness are
listed in Table 2. There were no statistically significant
differences between the psychometric properties of the
questionnaires in rheumatoid and non-rheumatoid
cases. There was a very high correlation between the
QDASH and the PRWE scores (Spearman’s rho = 0.90).
The scatter plot in Figure 2 demonstrates that the scores
are very similar, but not exactly numerically equivalent.
The QuickDASH scores are approximately five points
higher in the lower end of the scales (low disability),
while they are approximately ten points lower in the
higher end (high disability).
DISCUSSION
Earlier reports have demonstrated the validity of the
QuickDASH for assessment of patients with shoulder, el-
bow and basal thumb joint arthroplasty [3] and the va-
lidity of the PRWE for assessment of basal thumb joint
arthroplasty [12]. Our study indicates excellent psycho-
metric properties of the questionnaires when applied to
patients with TWA. The a priori formulated hypotheses
concerning construct validity were confirmed. Repro-
ducibility was very high. Cronbach’s alpha indicated a
strong internal consistency and possibly redundancy of
items. There were no floor/ceiling effects. Responsive-
TABLE 1
Construct validity of QuickDASH and PRWE according to three a priori
formulated hypotheses concerning the correla-tion of the scores with
grip strength, pain and wrist motion.
Spearman’s rho QuickDASH (p-value) PRWE (p-value)
Versus grip strength –0.56 ( 0.001) –0.50 ( 0.001)
Versus pain 0.54 ( 0.001) 0.59 ( 0.001)
Versus motion –0.10 (0.13) 0.22 (0.14)
PRWE = Patient-rated Wrist Evaluation questionnaire.
QuickDASH = Quick Disabilities of Arm Shoulder and Hand question-
naire.
TABLE 2
Reproducibility, responsiveness, internal consistency and floor-ceiling ef-
fect of the questionnaires.
QDASH PRWE
Reproducibility, Group 2
Spearman’s rho (p-value)
ICC, mean (range)
0.90 ( 0.001)
0.91 (0.85-0.95)
0.91 ( 0.001)
0.92 (0.87-0.96)
Responsiveness, Group 1
SRMa
ES
1.06
1.07
NA
NA
Internal consistency,
Cronbach’s alpha
Group 1
Group 2
0.96
NA
NA
0.97
Floor-ceiling effect, % of total
Group 1:
Floor
Ceiling
Group 2:
Floor
Ceiling
4
0
NA
NA
NA
NA
4
0
ES = effect size; ICC = intraclass coefficient; NA = not applicable; PRWE =
Patient-rated Wrist Evaluation question-naire; QuickDASH = Quick Dis-
abilities of Arm Shoulder and Hand questionnaire; SD = standard devi-
ation; SRM = standardised response mean.
a) Mean score (± SD) was 55.2 (± 18.3) preoperatively and 35.4 (± 23.7)
post-operatively. Difference in score was 19.6 (± 18.5).](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-121-320.jpg)
![122
DANISH MEDICAL JOURNAL
ness to treatment was high according to the QuickDASH.
It may be argued that we could have chosen to measure
internal consistency, construct validity and floor/ceiling
effects of the QuickDASHin in Group 2, as we did for the
PRWE, but we chose to take advantage of a larger avail-
able sample. In the systematic review of the measure-
ment properties of the QuickDASH and its cross cultural
adaptations performed by Kennedy et al [2], the studies
were assessed with a recently described method: con-
sensus-based standards for the selection of health
measurement instruments (COSMIN). The studies with
the best methodological quality showed high Cronbach’s
alpha values for internal consistency (0.92-0.94) and ICC
values that ranged from 0.90 to 0.94. Hypothesis testing
was evaluated in nine studies with a range of overall
methodological quality: one excellent, six fair and two
poor. Correlations were in the expected magnitude and
direction: high for target construct (pain, function),
moderate for work disability measures and low for men-
tal health measures. Coefficients for the correlation with
pain were 0.64 to 0.73. Several studies found acceptable
SRM/ES after treatment of known efficacy (0.58-1.77),
which indicates that the Quick DASH is sensitive to vary-
ing amounts of change. Thus, the reported psychometric
properties were generally in agreement with our find-
ings, although they were not investigated in patients
with TWA.
At present, no systematic review of the psychomet-
ric properties of the PRWE is available, and it is far be-
yond the scope of this study to do so with the COSMIN
method, but we have identified a number of relevant
papers. Table 3 shows a summary of the internal con-
sistency, reproducibility and responsiveness in these
studies. A weak correlation with wrist motion and a
moderate correlation with grip strength were found in
patients with tendon interposition arthroplasty [12, 16,
18]. Correlations with VAS scores were moderate [14,
16, 17]. Fairplay et al found a high internal consistency
(Cronbach’s alpha = 0.96) and reproducibility (Spear-
man’s rho = 0.93) in 63 patients with chronic wrist or
hand pain [15]. These figures also are consistent with
our findings in TWA patients.
One weakness of our study is that we were unable
to assess the responsiveness of the PRWE since the Dan-
ish questionnaire was not available when we started
sampling data in 2003. The surgical procedure itself is in-
frequent to an extent that it is necessary to collect data
throughout several years in order to obtain sufficiently
large numbers. Apart from this flaw, our analysis shows
very similar psychometric properties for the two ques-
tionnaires. The fact that the scores produced by the
scales were numerically very close is unexpected, be-
cause the QuickDASH is generally considered a generic
upper limb instrument, whereas the PRWE is considered
a specific wrist evaluation instrument. Notwithstanding
the important fact that the psychometric properties of
the two questionnaires did not differ between rheuma-
toid and non-rheumatoid patients, the scores of the
rheumatoid patients in Group 1 were higher than the
scores of the non-rheumatoid patients, which means
that they had a higher grade of disability.
This must be interpreted in the light of the fact that
the rheumatoid patients generally have multiple joint in-
volvement. The difference was not significant in Group
2, which might be attributed to a smaller and hence an
underpowered sample. It is also interesting and unex-
pected that the scores of both scales correlated equally
with the general pain level, expressed on a visual ana-
logue scale, because the PRWE contains a very detailed
section with five specific pain questions, whereas the
QDASH only has two general pain questions. This con-
firms that the level of pain is important, but not crucial
for the construct measured and that multiple questions
regarding pain may be superfluous and may contribute
to item redundancy. The lack of correlation of the scores
with mobility is in agreement with the study of Murphy
et al 2003 [19] that failed to demonstrate any difference
in DASH or PRWE scores between TWA and total wrist
FIGURE 2
Scatter plot showing the QuickDASH- and the PRWE-scores in patients
with total wrist arthro-plasty. The curved line is the LOESS (local regres-
sion) line, the thin solid line is the regression line and the thick solid line
is the line of equivalency. Dots located on the line of equivalency repre-
sent patients whose QuickDASH and PRWE-scores are equal. Dots below
this line indicate a QuickDASH-score that is lower than the PRWE-score
for a given patient and vice-versa. The trend indicated by the LOESS-line
is that the QuickDASH scores are approximately five points higher than
the PRWE-scores in the lower end of the scales, whereas they are ap-
proximately ten points lower in the higher end.
20
20 40 60 80 PRWE0
0
40
60
80
QuickDASH
PRWE = Patient-rated Wrist Evaluation questionnaire.
QuickDASH = Quick Disabilities of Arm Shoulder and Hand questionnaire.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-122-320.jpg)
![123
DANISH MEDICAL JOURNAL
fusion (TWF) in a group of patients with generalised
arthritis.
In our study, we were unable to assess the criterion
validity of the scales. Criterion-related validity is based
on evidence that shows the extent to which the scores
of the instrument are related to a criterion measure or
gold standard. The challenge is that there is no readily
available gold standard: The authors and the institutions
that developed the QuickDASH state that its criterion va-
lidity has not been tested because of the absence of a
gold standard measure for the concept of upper-limb
disability and hand function [20]. Nor could we make a
direct assessment of the respondent burden, defined as
the time, energy, and other demands placed on the pa-
tients to whom the instruments are administered be-
cause our patients answered the questionnaires unat-
tended. However, the low number of missing items and
the number of responses in the test-retest indicate an
acceptable respondent burden and feasibility.
Future research must include other methods for
evaluating scaling properties, like the Rasch analysis, not
the least to assess unidimensionality and possible item
redundancy suggested by the very high Cronbach’s
alpha.
CORRESPONDENCE: Michel E.H. Boeckstyns, Kløverbakken 11, 2830 Virum,
Denmark. E-mail mibo@dadlnet.dk
ACCEPTED: 20 August 2014
CONFLICTS OF INTEREST: none. Disclosure forms provided by the authors
are available with the full text of this article at www.danmedj.dk
LITERATURE
1. Beaton DE, Wright JG, Katz JN. Development of the QuickDASH:
comparison of three item-reduction approaches. J Bone Joint Surg
2005;87:1038-46.
2. Kennedy CA, Beaton DE, Smith P et al. Measurement properties of the
QuickDASH (disabilities of the arm, shoulder and hand) outcome measure
and cross-cultural adaptations of the QuickDASH: a systematic review.
Qual Life Res 2013;22:2509-47.
3. Angst F, Goldhahn J, Drerup S et al. How sharp is the short QuickDASH?
A refined content and validity analysis of the short form of the disabilities
of the shoulder, arm and hand questionnaire in the strata of symptoms
and function and specific joint conditions. Qual Life Res 2009;18:1043-51.
4. MacDermid JC. Development of a scale for patient rating of wrist pain and
disability. J Hand Ther 1996;9:178-83.
5. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-
related quality of life measures: literature review and proposed guidelines.
J Clin Epidemiol 1993;46:1417-32.
6. Herup A, Merser S, Boeckstyns M. Validation of questionnaire for condi-
tions of the upper extremity. Ugeskr Læger 2010;172:3333-6.
7. Schønnemann JO. A comparison between two types of osteosynthesis for
distal radius fractures using validated Danish outcome measures. Aarhus:
Faculty of Health Sciences, University of Aarhus, 2010.
8. Terwee CB, Bot SD, de Boer MR et al. Quality criteria were proposed for
measurement properties of health status questionnaires. J Clin Epidemiol
2007;60:34-42.
9. Chung MK. Correlation coefficient. In: Salkin NJ, ed. Encyclopedia of
measurement and statistics. London: Sage Publications, 2007:189-201.
10. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Edu
2011;2:53-5.
11. Husted JA, Cook RJ, Farewell VT et al. Methods for assessing responsive-
ness: a critical review and recommendations. J Clin Epidemiol 2000;
53:459-68.
12. John M, Angst F, Awiszus F et al. The patient-rated wrist evaluation
(PRWE): cross-cultural adaptation into German and evaluation of its
psychometric properties. Clin Exp Rheumatol 2008;26:1047-58.
13. MacDermid JC, Turgeon T, Richards RS et al. Patient rating of wrist pain
and disability: a reliable and valid measurement tool. J Orthop Trauma
1998;12:577-86.
14. Kim JK, Kang JS. Evaluation of the Korean version of the patient-rated wrist
evaluation. J Hand Ther 2013;26:238-43.
15. Fairplay T, Atzei A, Corradi M et al. Cross-cultural adaptation and validation
of the Italian version of the patient-rated wrist/hand evaluation question-
naire. J Hand Surg Eur 2012;37:863-70.
TABLE 3
Psychometric properties of different versions of the PRWE in published studies.
Reference Version Diagnosis Cases, n
Internal consistency,
Cronbach’s alpha Reproducibility Responsiveness
MacDermid et al, 1998 [13] English Wrist fractures 101 – ICC 0.90 –
MacDermid et al, 2000b
English Wrist fractures 59 – – SRM = 2.27
Kim Kang, 2013 [14] Korean Wrist fractures 63 0.94 ICC = 0.96 ES = 0.94
SRM = 0.98
Wilcke et al, 2009b
Swedish Wrist fractures 99/49a
0.94-0.97 Spearman’s
rho = 0.99
ES = 1.3
SRM = 1.4-1.7
Mellstrand et al, 2011b
Swedish Wrist injuries 124 0.97 ICC = 0.93 SRM = 1.29
Fairplay et al, 2012 [15] Italian Chronic wrist pain 63 0.96 Spearman’s
rho = 0.93
–
Imaeda et al, 2010b
Japanese Various wrist conditions 117/50a
0.95 ICC = 0.92 ES = 1.9
SRM = 1.6
John et al, 2008 [12] German CMC1-arthritis after interposition 103/51a
0.97 ICC = 0.86 –
Hemelaers et al, 2008 [16] German Wrist fractures 44 0.98 ICC = 0.94 –
Wong et al, 2007b
Chinese (Hong Kong) Wrist injuries 47 0.78-0.93 – –
Schonnemann et al, 2013 [17] Danish Wrist fractures 60 0.94 ICC = 0.88 ES= 0.62
Present study Danish Total wrist arthroplasty 52/48a
0.97 ICC = 0.92
Spearman’s
rho = 0.91
ES = 1.07
SRM = 1.06
ES = effect size; CMC = carpometacarpal; ICC = intraclass coefficient; PRWE = Patient-rated Wrist Eval-uation questionnaire; SD = standard deviation; SRM = standardised response
mean.
a) The second figure refers to a subset of cases used in a test-retest.
b) Reference available from corresponding author.](https://image.slidesharecdn.com/0de89a47-de39-40ba-9d2b-8caf3d34da15-160120195349/85/DISPUTATS-FINAL-123-320.jpg)


