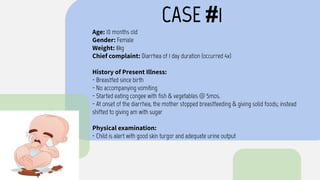
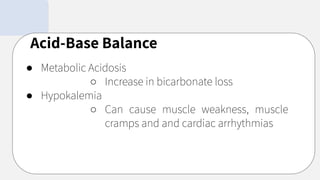
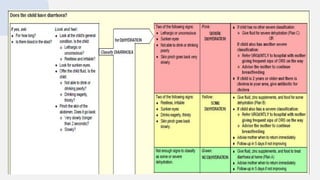
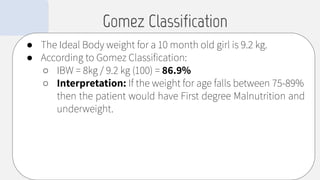
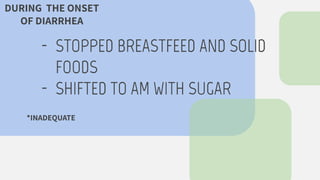
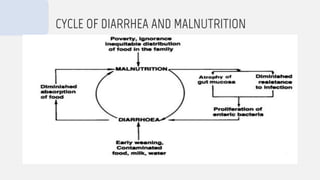
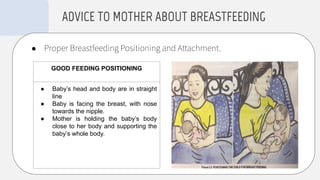
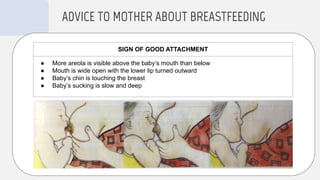
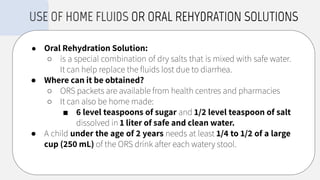
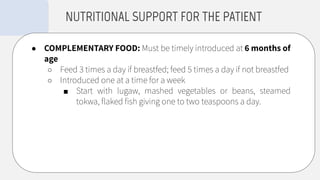
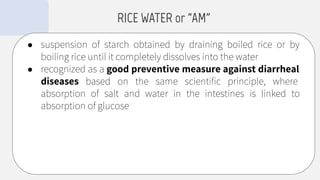
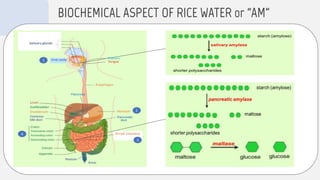
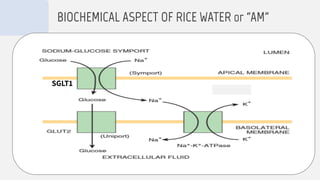
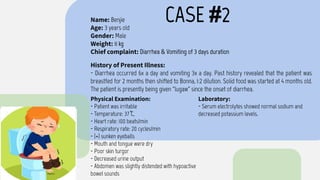
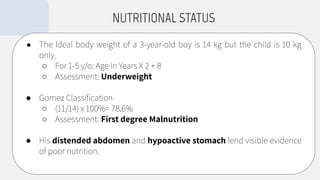
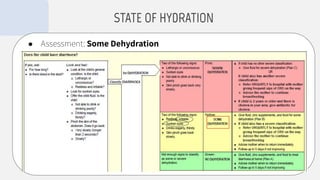
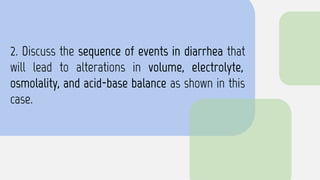
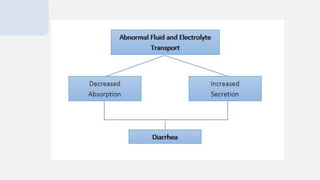
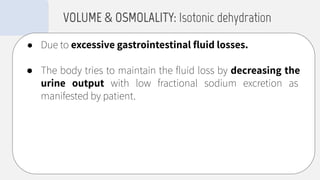
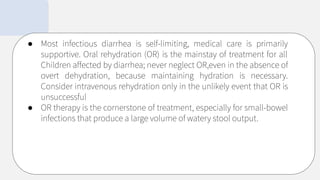
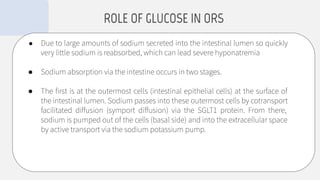
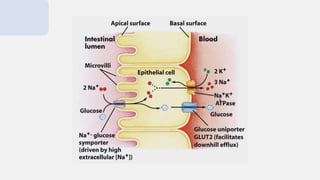
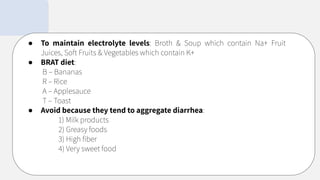
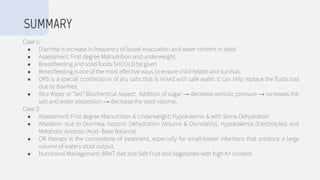
The document discusses two cases of pediatric diarrhea and provides recommendations for treatment. It evaluates the patients' nutritional status and hydration, describes the metabolic changes that occur during diarrhea, and advises breastfeeding and oral rehydration solutions to prevent dehydration. Proper feeding practices and nutrition are emphasized to break the cycle of malnutrition and diarrhea.