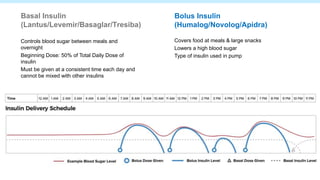
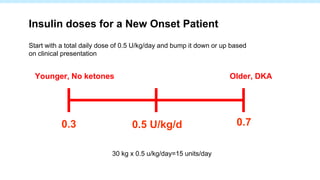
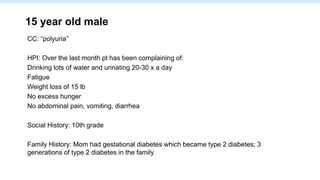
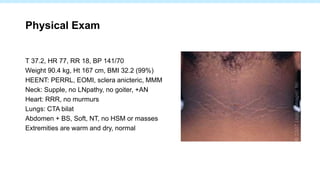
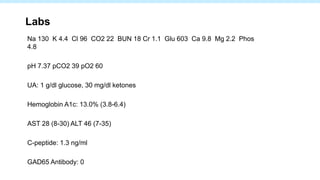
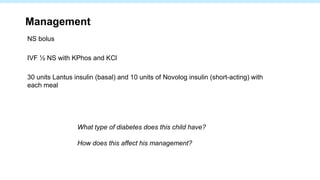
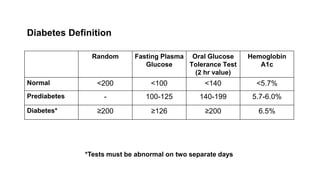
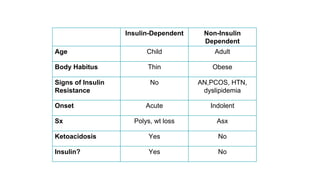
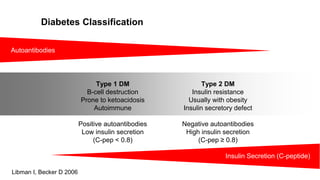
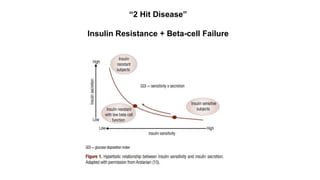
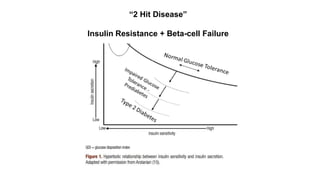
This 15-year-old male presented with polyuria, fatigue, and weight loss over the past month. His labs showed severely elevated blood glucose and ketones, along with an A1C of 13%. He was diagnosed with type 1 diabetes and started on basal and bolus insulin therapy. Type 1 diabetes results from beta cell destruction leading to insulin deficiency, whereas type 2 diabetes involves insulin resistance along with relative insulin deficiency. This patient's presentation with ketoacidosis and need for insulin therapy indicates he has type 1 rather than type 2 diabetes.

![SEARCH
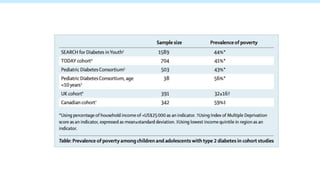
5 centers supported by CDC and NIDDK
– California (Kaiser Permanente Southern California, excluding San Diego
[7 counties])
– Colorado [14 counties, including Denver]
– Ohio [8 counties, including Cincinnati]
– South Carolina [4 counties, including Columbia]
– Washington state [5 counties, including Seattle]
Type 1a (Ab+, low c-pep(<0.6)); Type 1b (Ab-, low c-pep); type 2
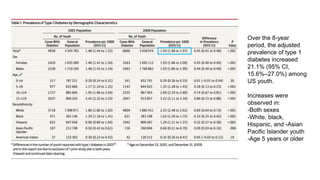
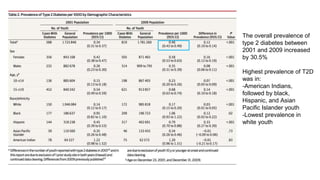
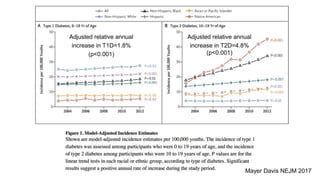
The study population included youth younger than 20 years residing in the
geographic study areas or who were members of participating health plans in
2001 and 2009.
Dabelea, JAMA 2014](https://image.slidesharecdn.com/2018t1dt2dresidentlecturejul3018-180730235806/85/Diabetes-Resident-Lecture-46-320.jpg)