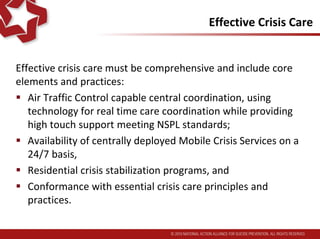
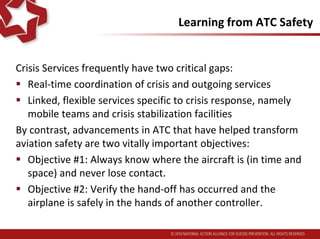
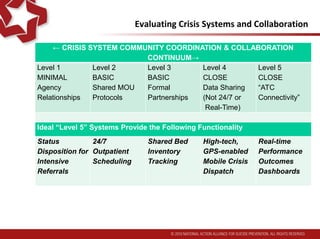
The Task Force recommends transforming crisis services to a comprehensive system with these core elements: central coordination with real-time technology; 24/7 mobile crisis services; crisis stabilization facilities; and conforming to essential crisis care principles. It recommends adopting Air Traffic Control-like coordination standards and Zero Suicide practices. National and state authorities should review ATC-qualified crisis systems and implement comparable capabilities within 5 years so every US region has crisis hubs. Health payers should recognize and reimburse for crisis services from comprehensive systems.