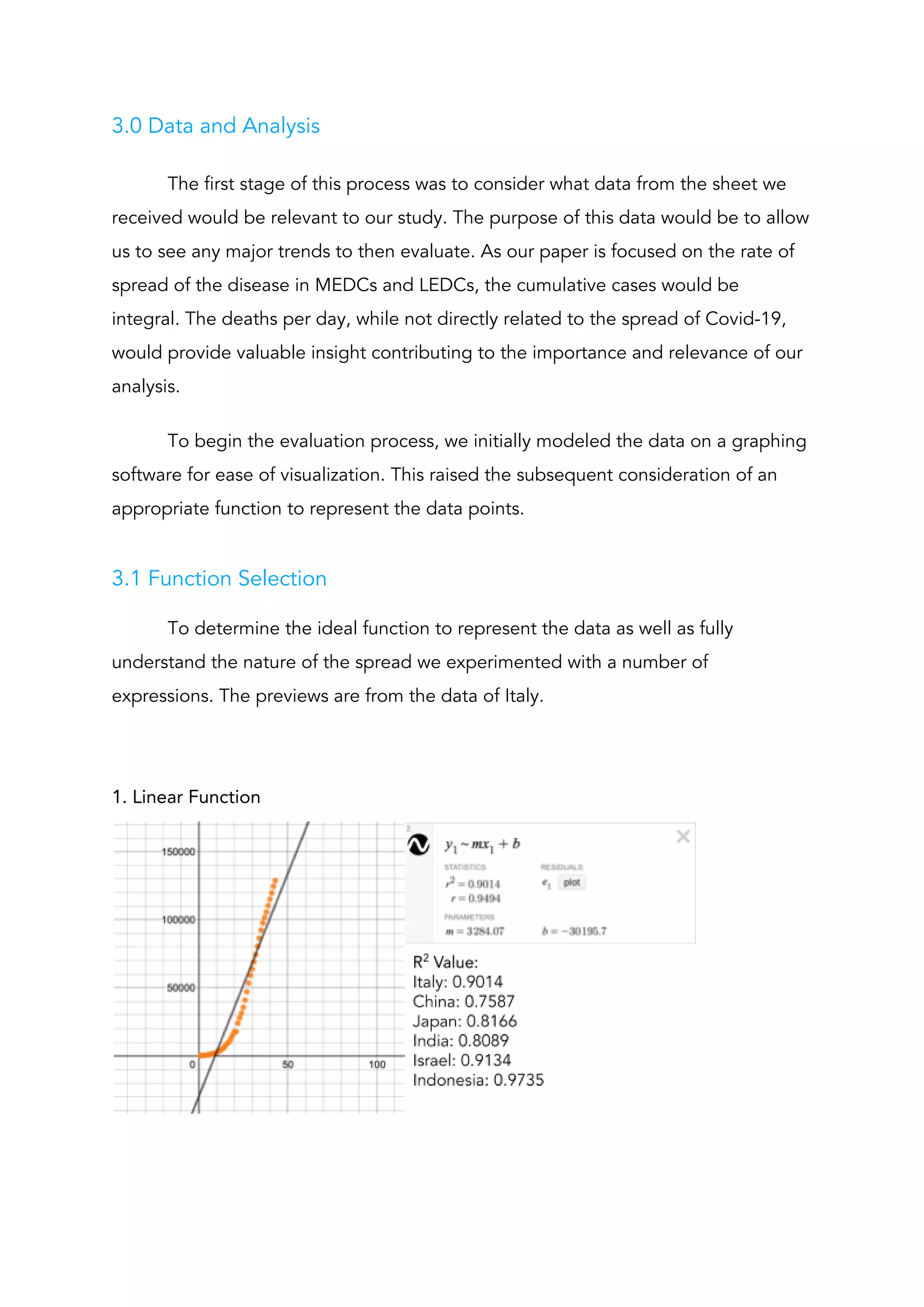
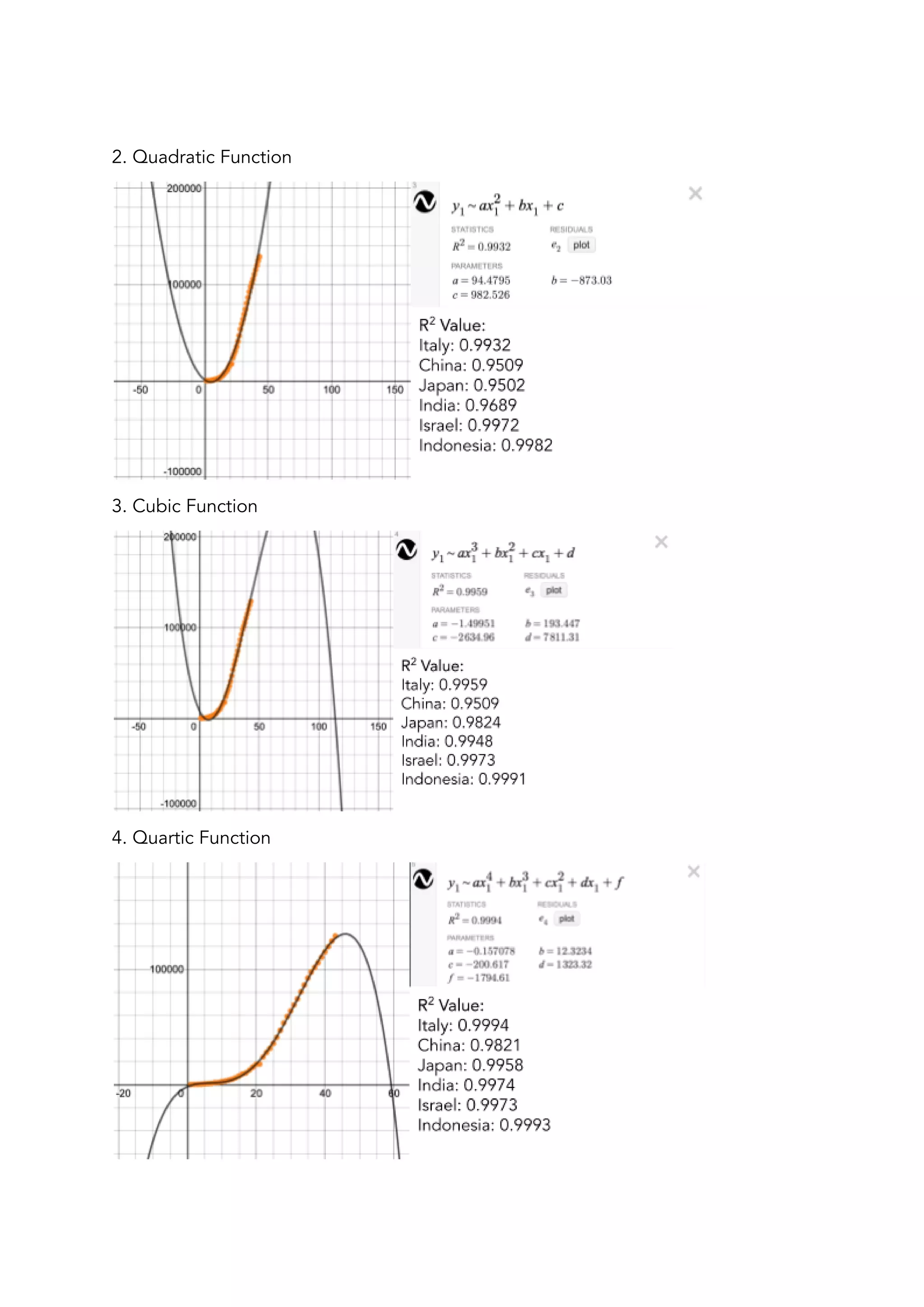
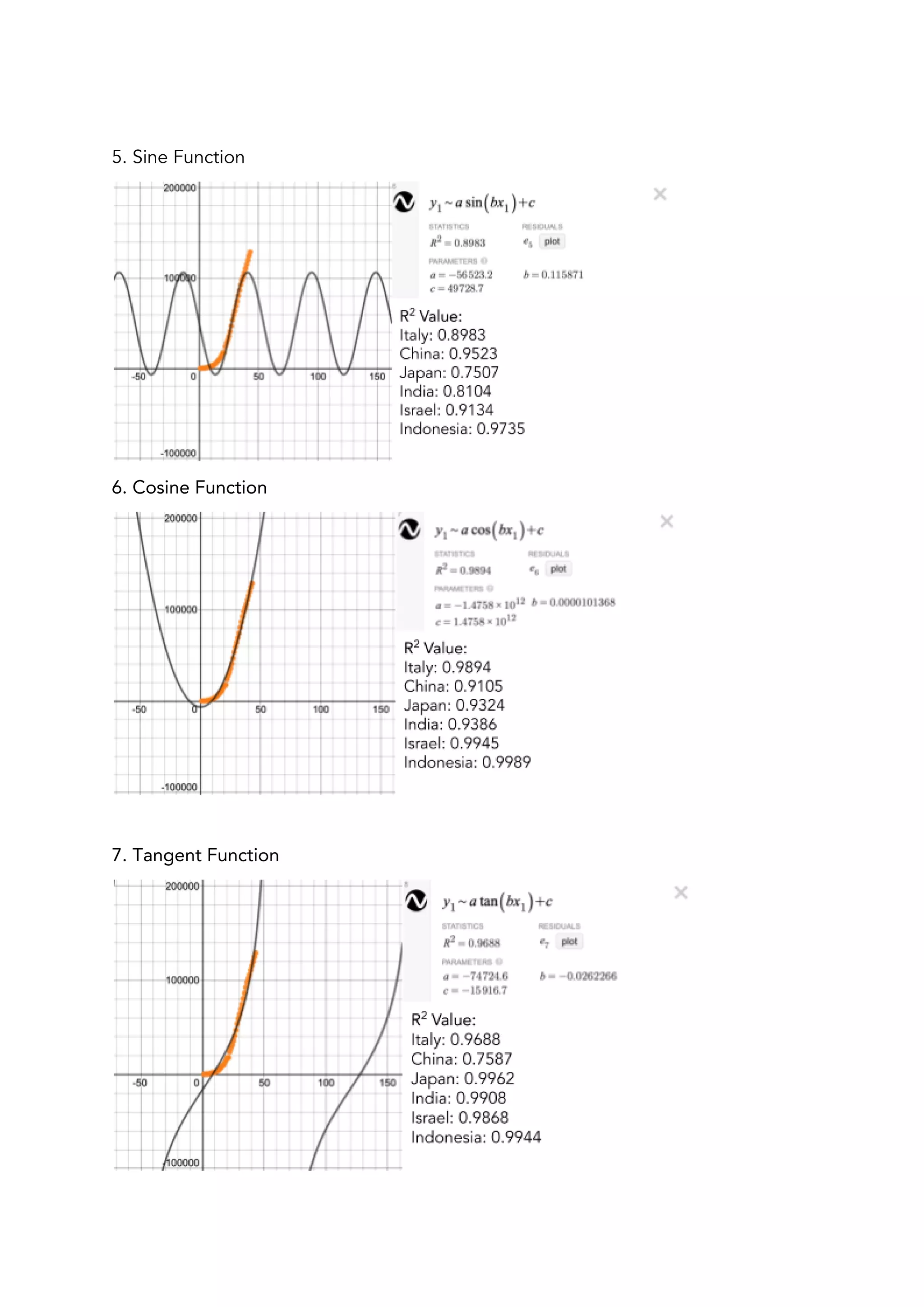
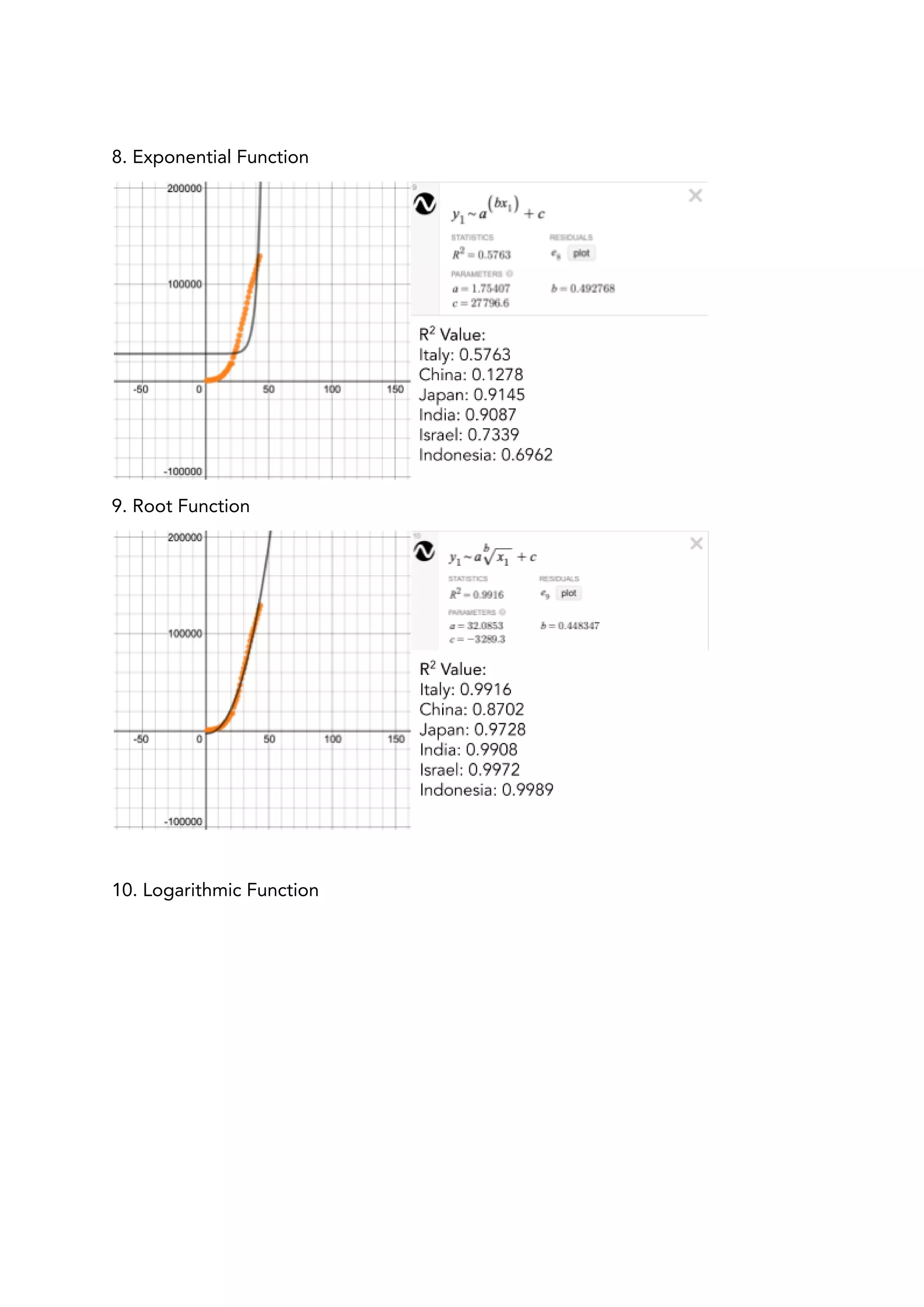
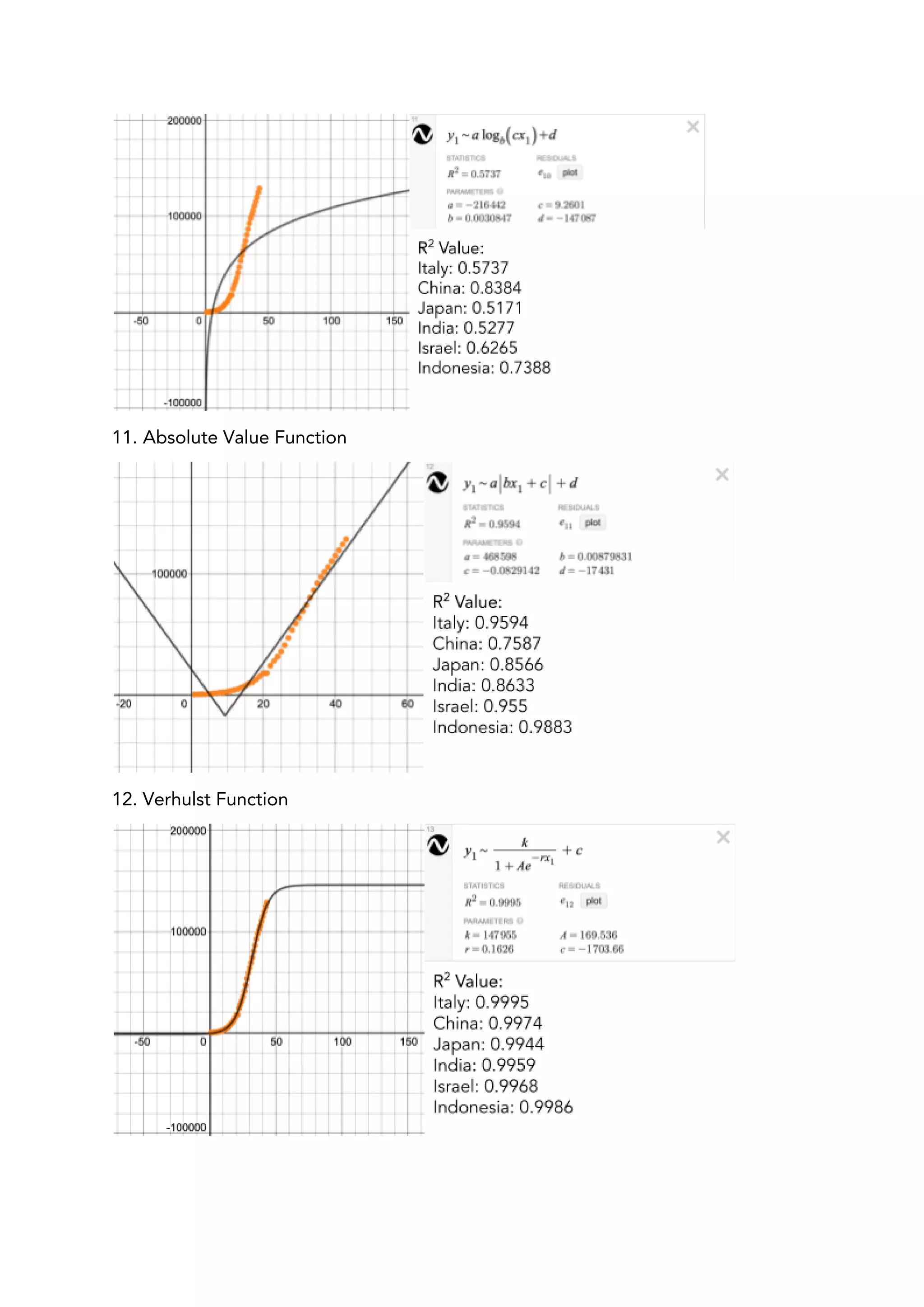
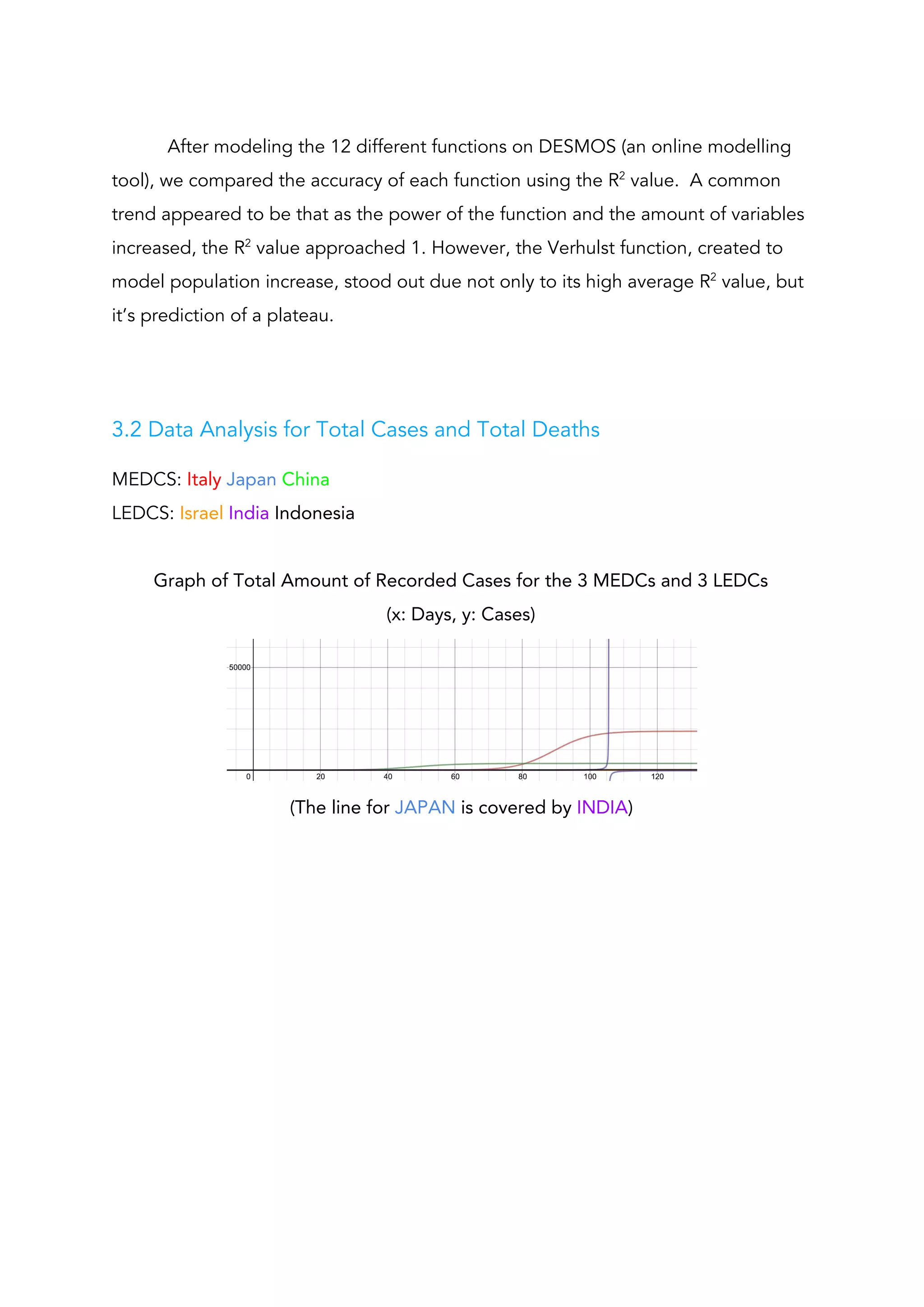
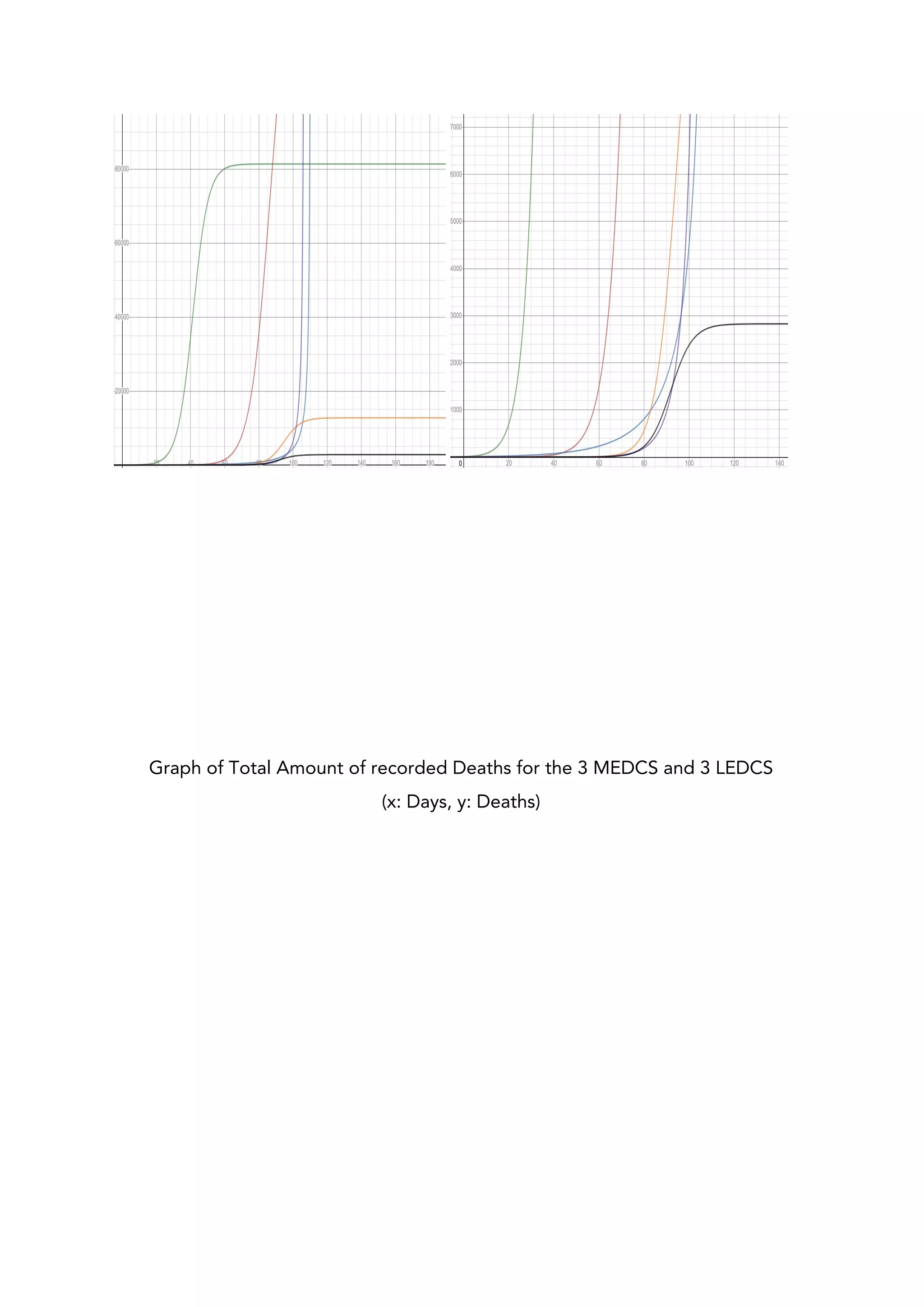
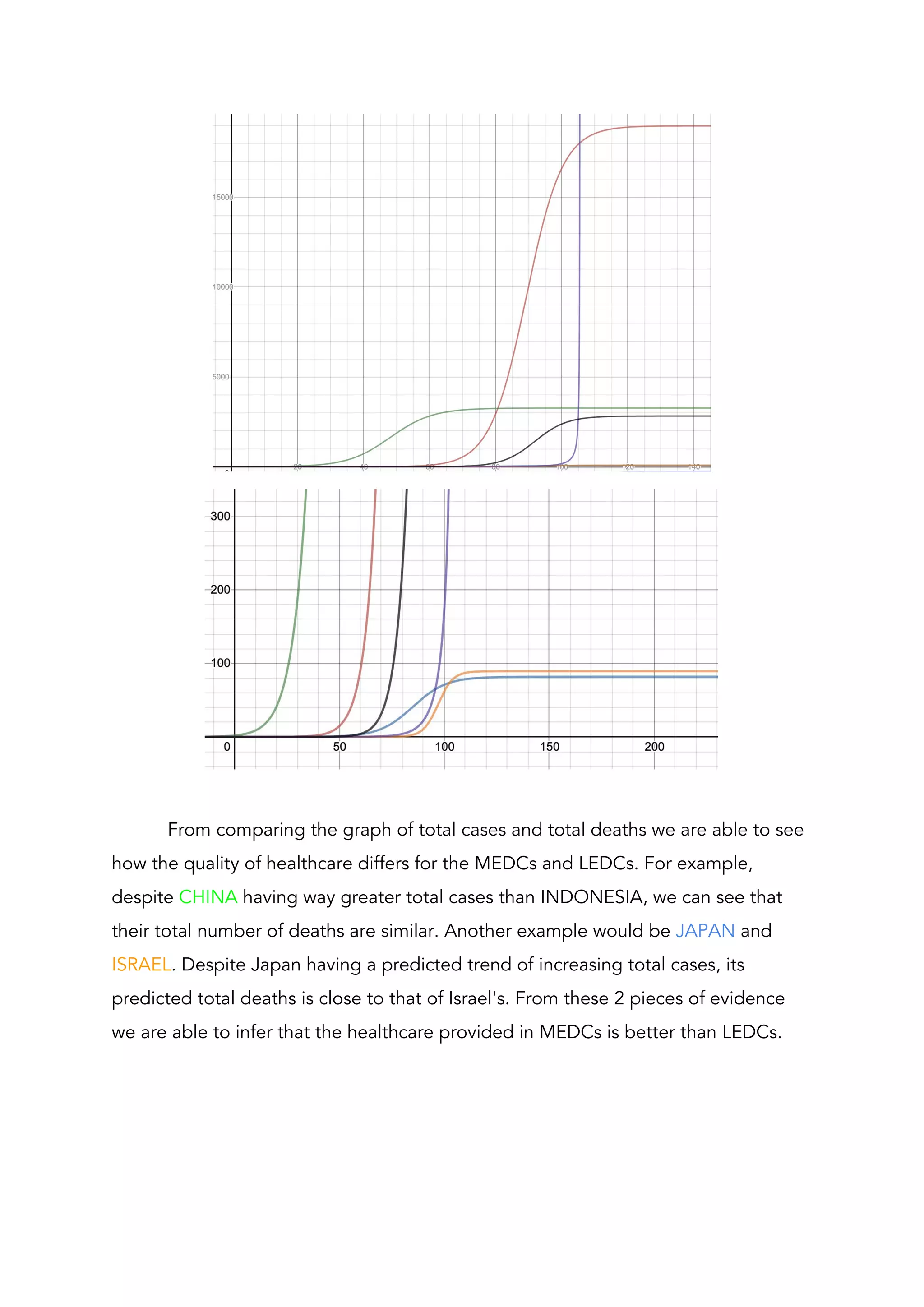
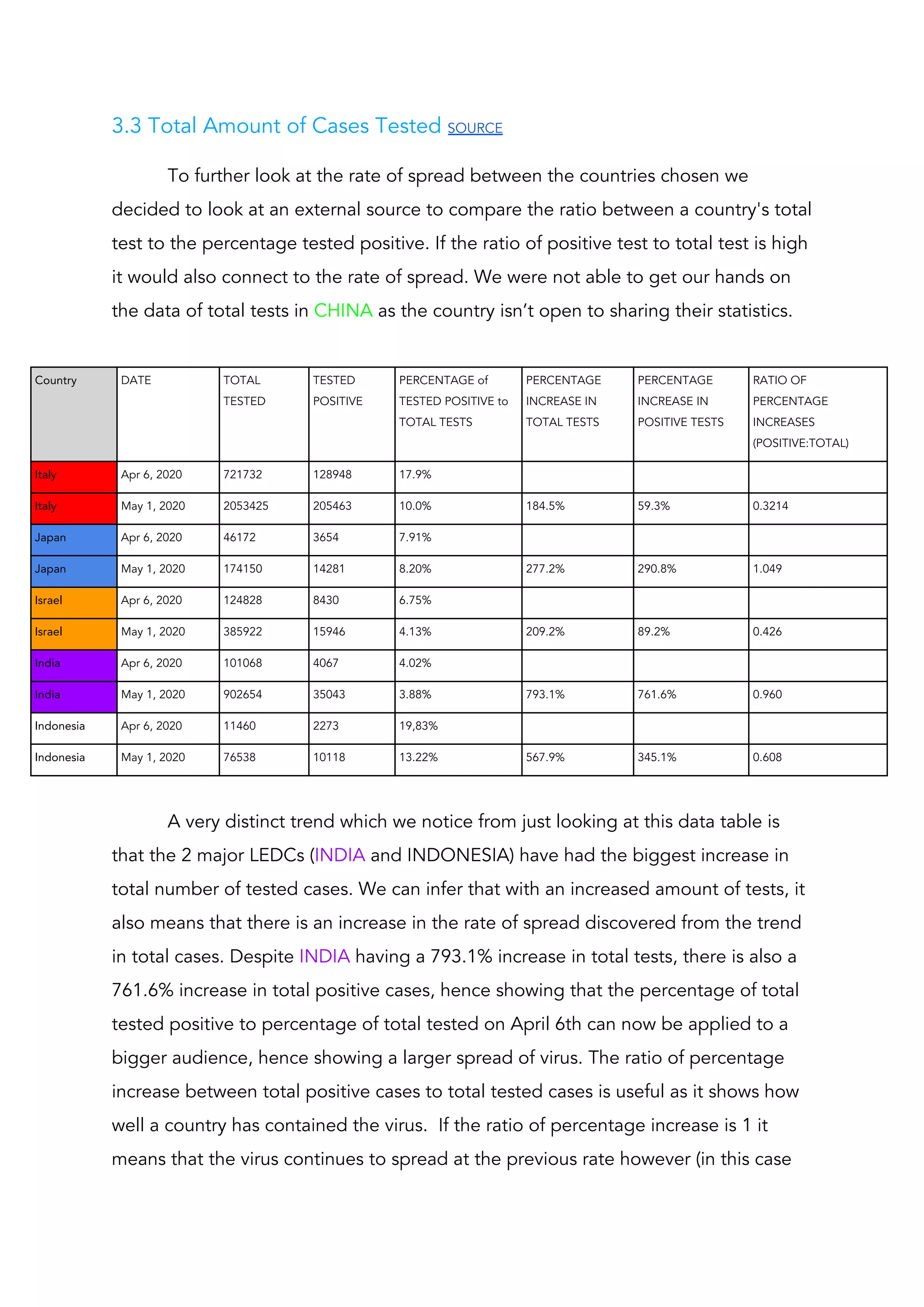
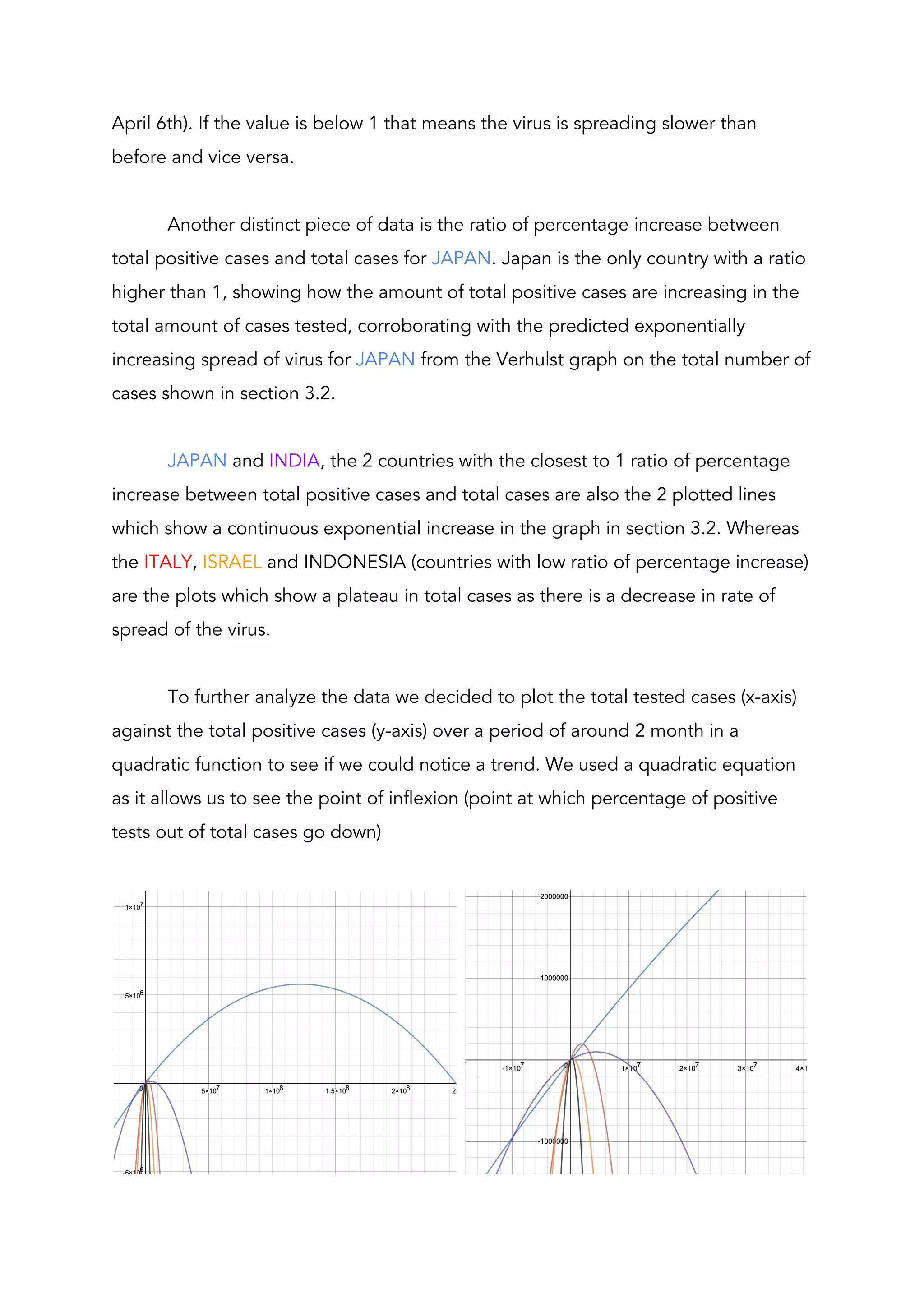
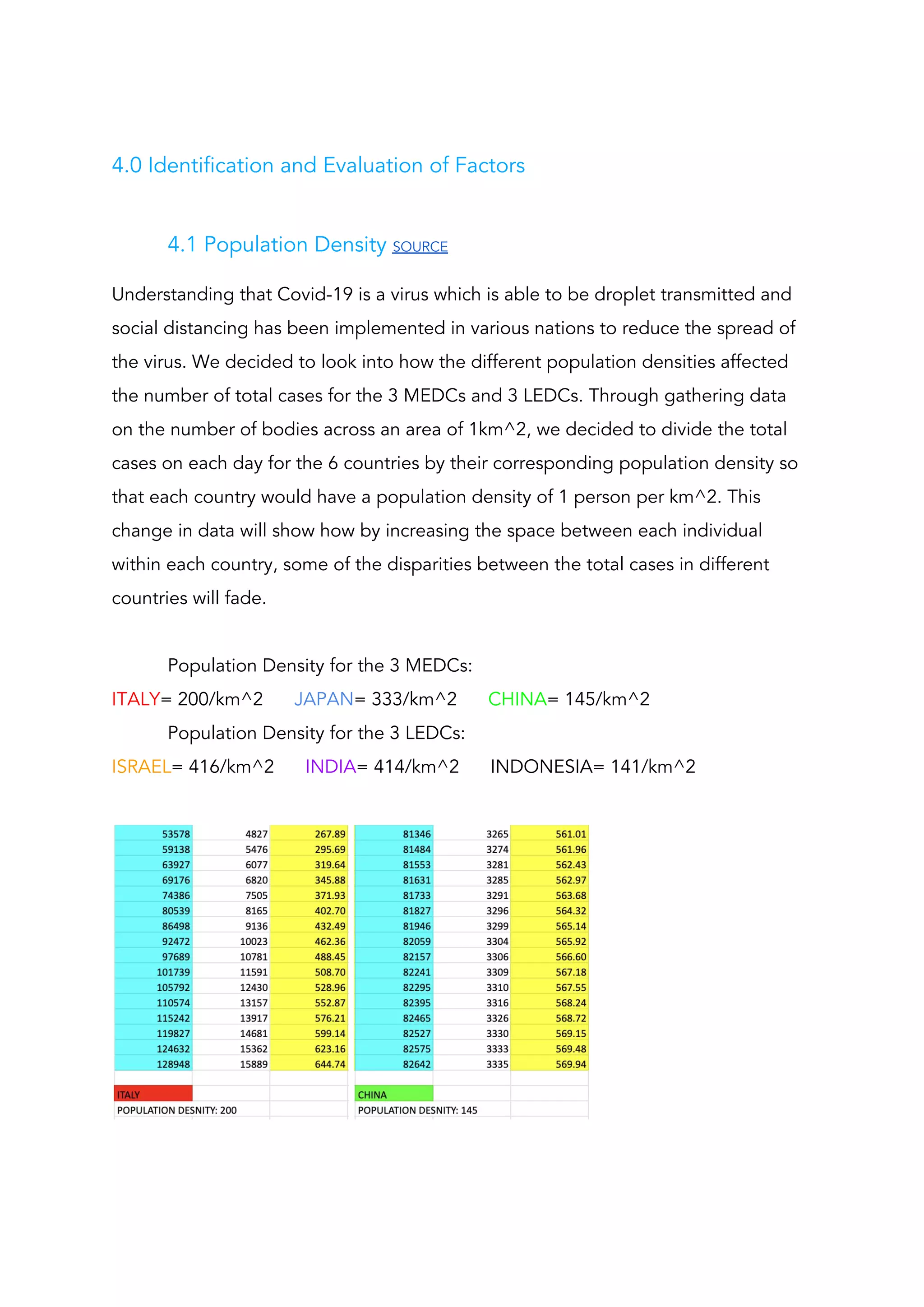
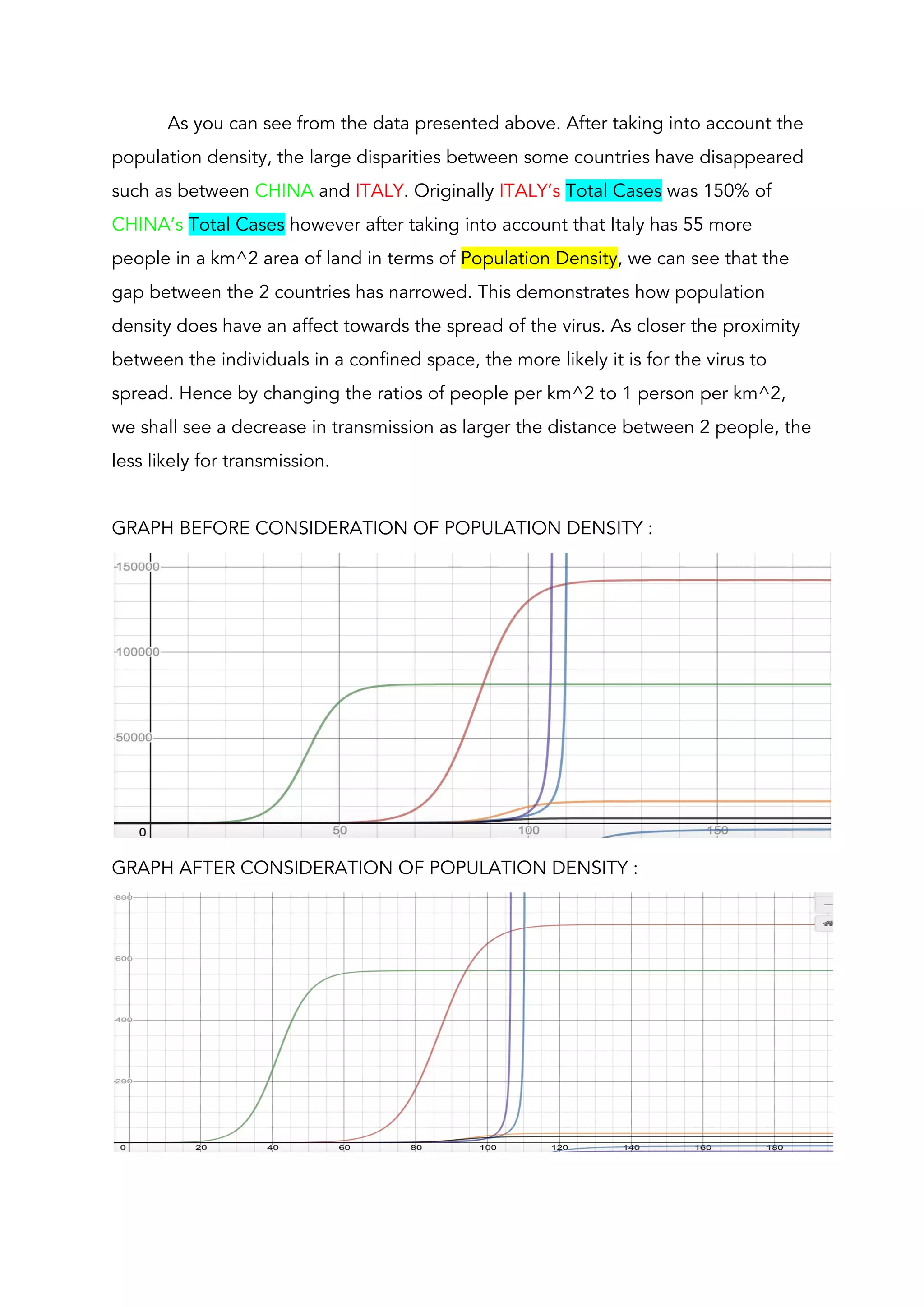
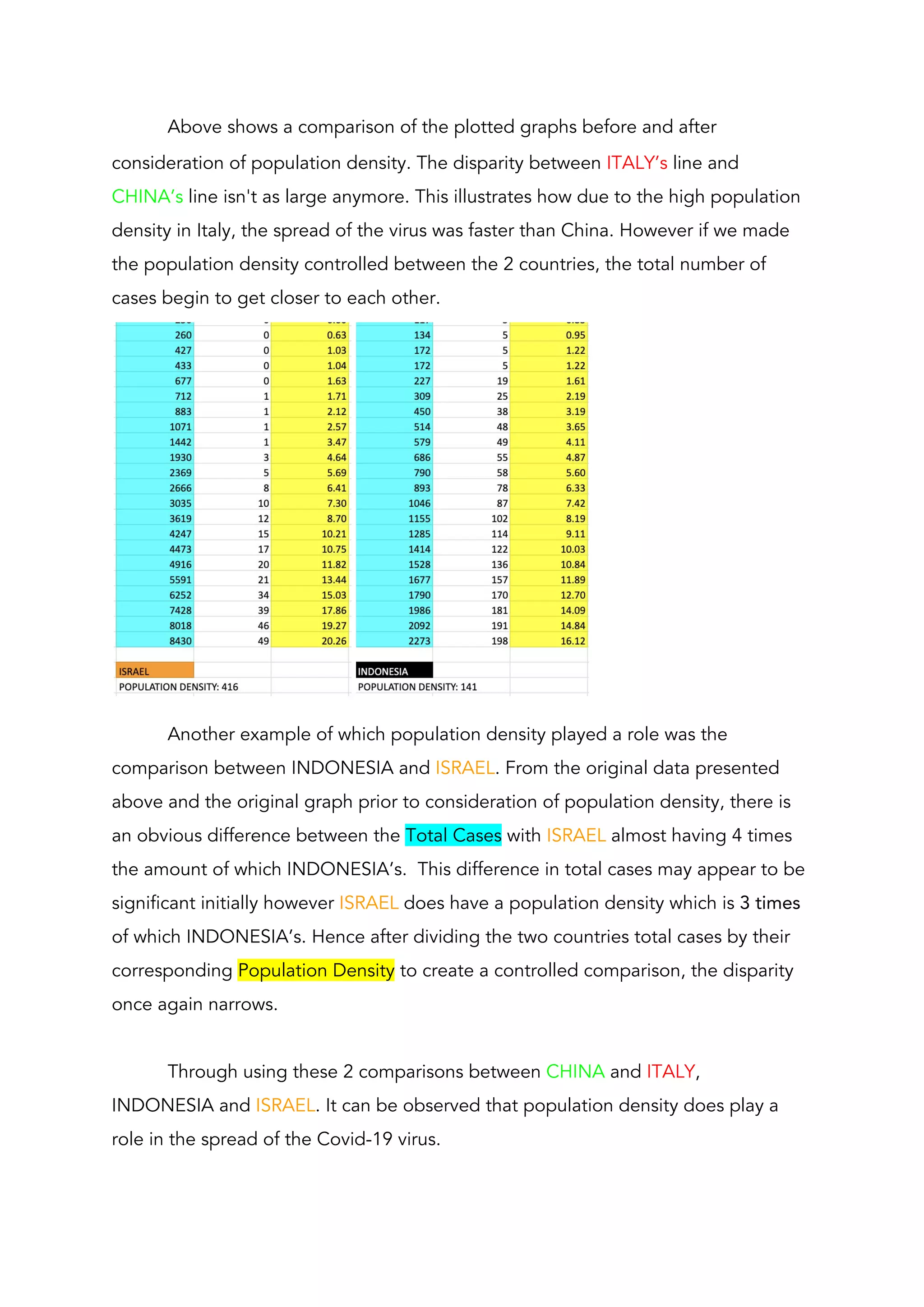
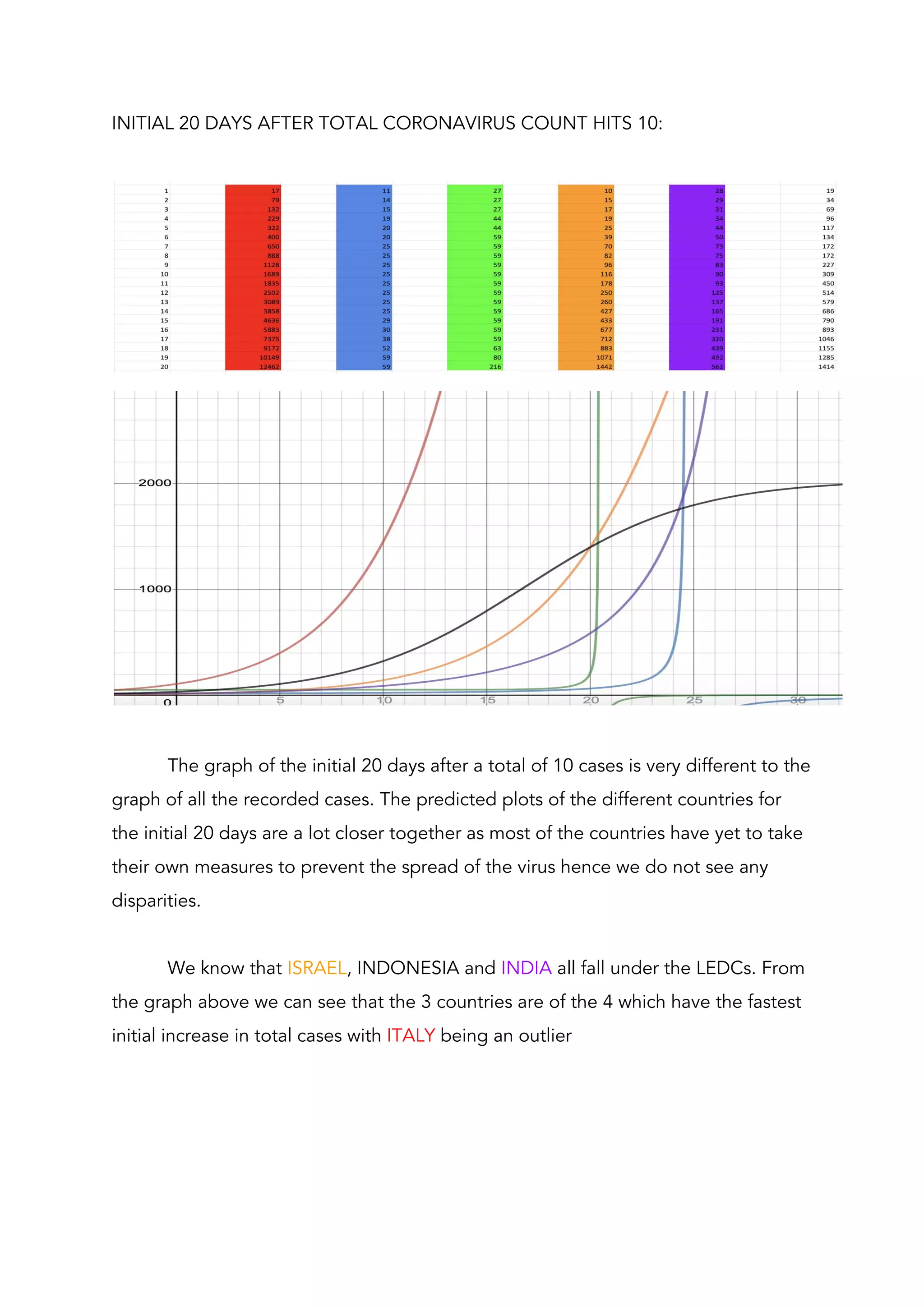
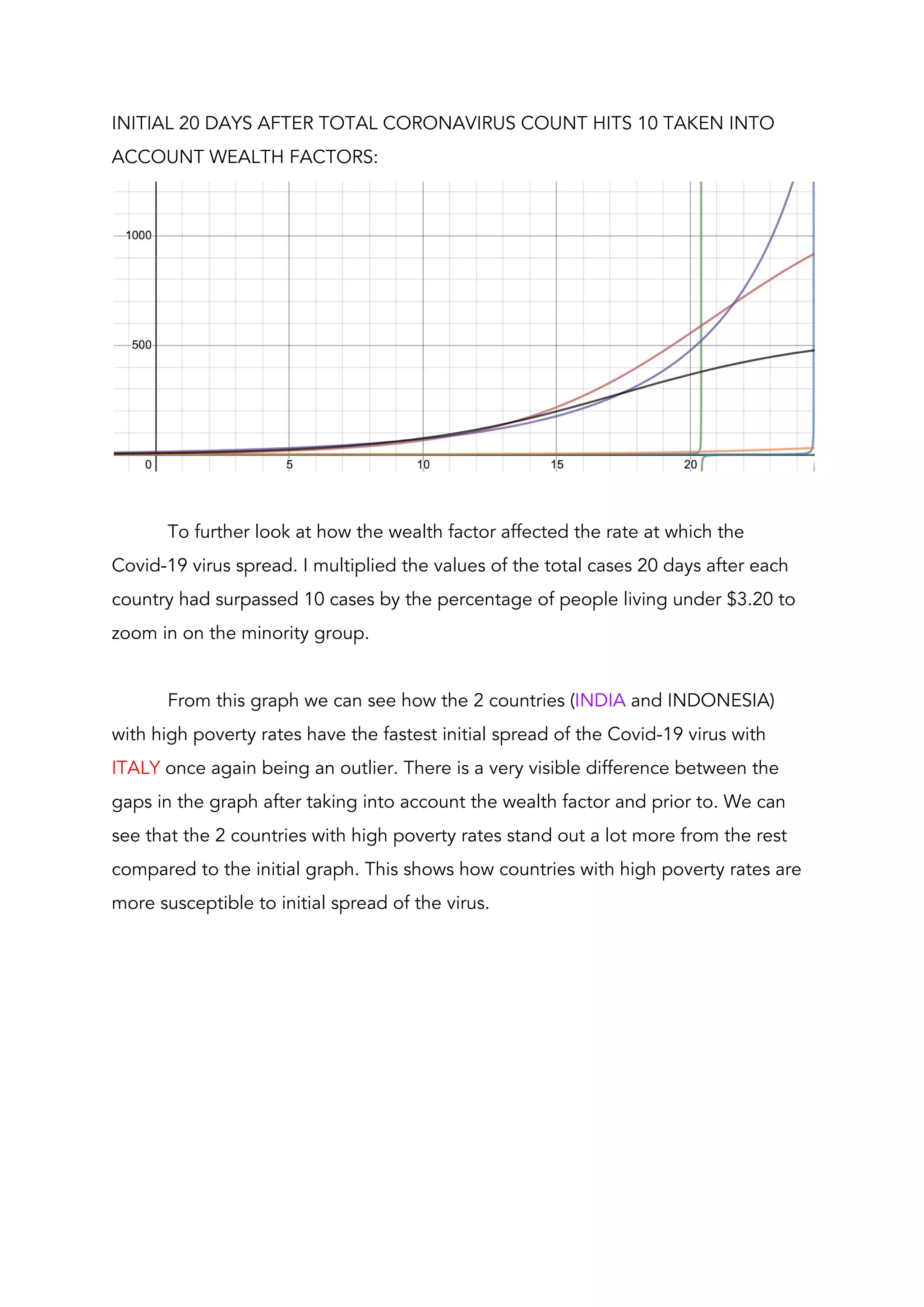
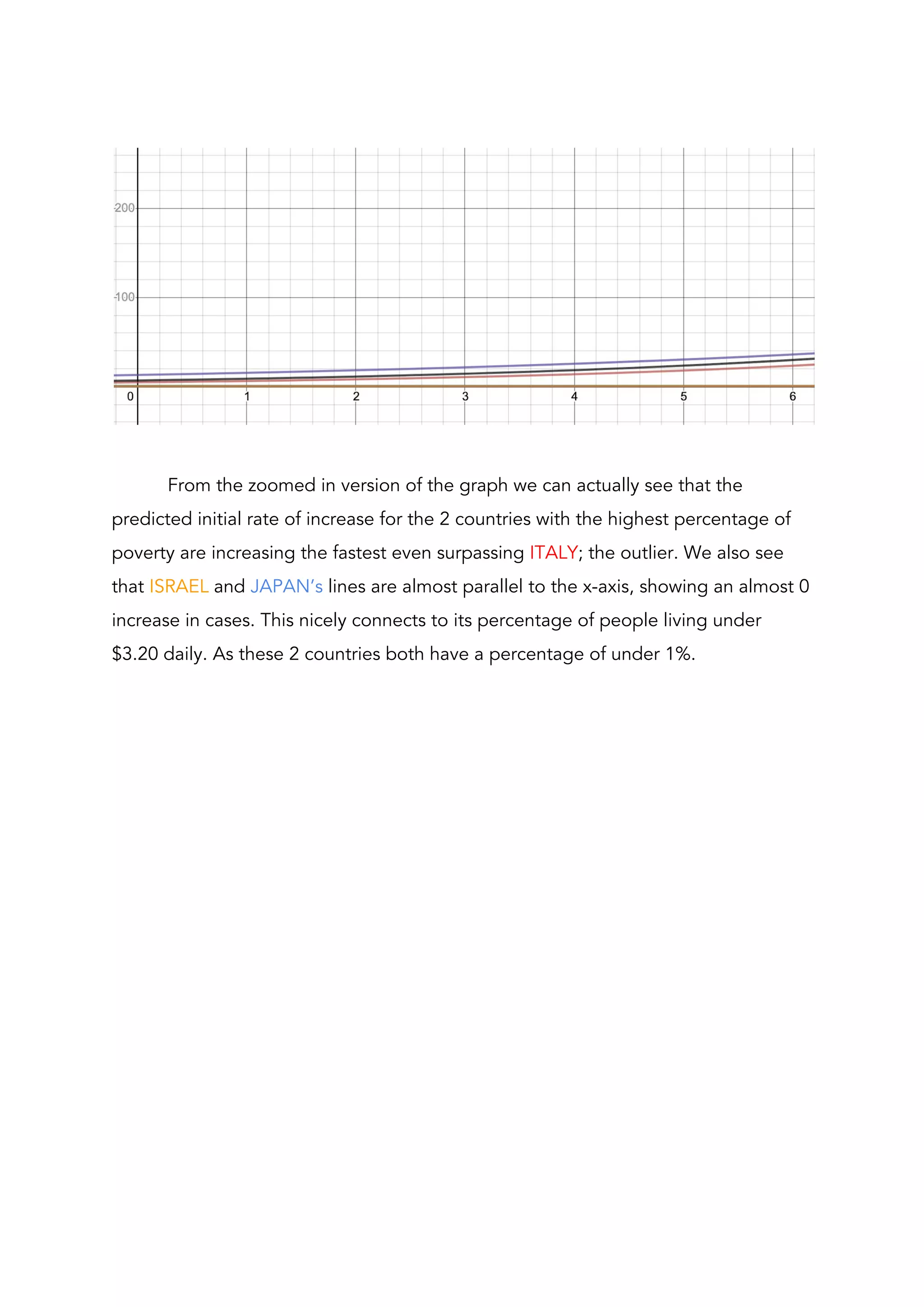
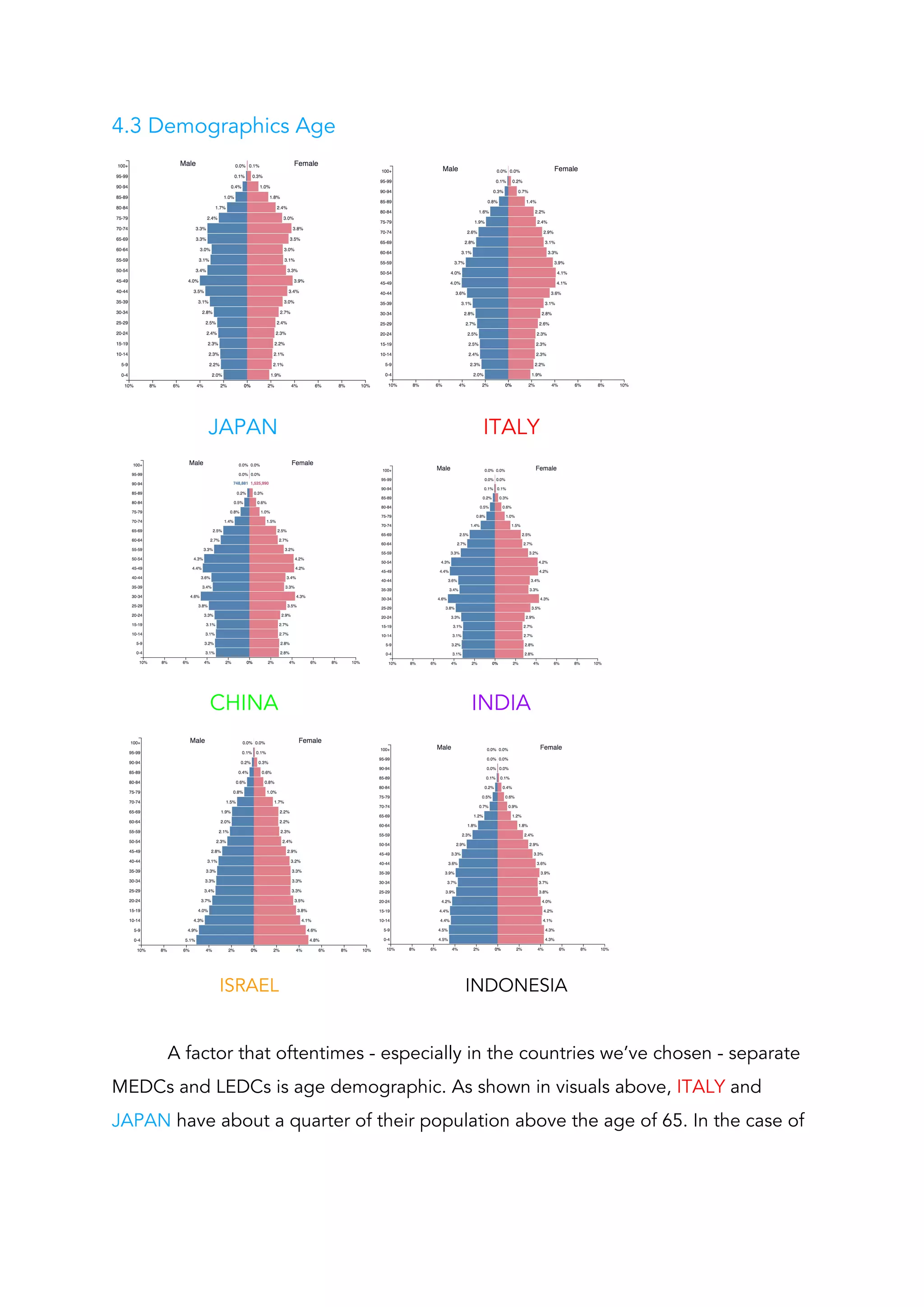
This document analyzes factors that influence the spread of COVID-19 in different countries. It compares the total cases and deaths in 3 more economically developed countries (MEDCs) - Italy, Japan, China - and 3 less economically developed countries (LEDCs) - Israel, India, Indonesia. By modeling the data with different functions, the author finds that a Verhulst function best represents the data, predicting a plateau. Analysis of total tests and positive cases shows Japan having the highest continued spread. Considering population density helps explain differences in case numbers between countries like Italy and China. The document evaluates how factors like population density, healthcare quality, and testing rates impact the spread of COVID-19 in different nations.