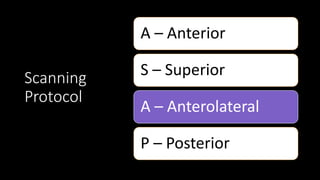
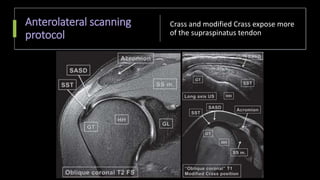
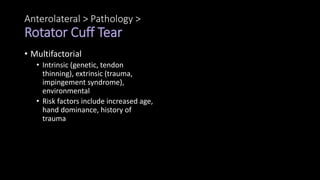
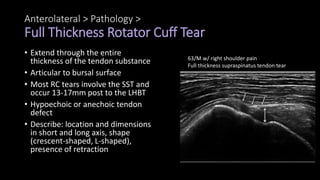
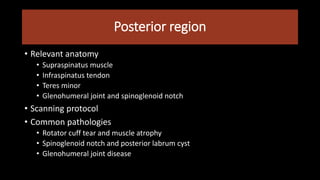
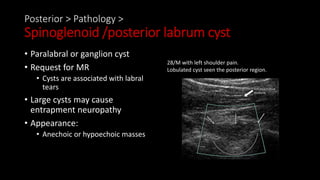
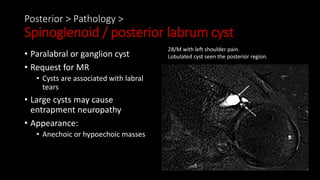
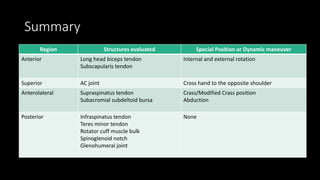
The document outlines a comprehensive approach to shoulder ultrasound examinations, focusing on standardized protocols for imaging various shoulder pathologies. It highlights the advantages of ultrasound, including real-time imaging and cost-effectiveness, while also discussing its limitations and challenges. The study emphasizes the importance of a structured examination framework to improve diagnostic accuracy and clinical implementation of shoulder ultrasound.














![Conclusion
• US is an important and complementary imaging tool for the
evaluation of the superficial soft-tissue structures of the shoulder.
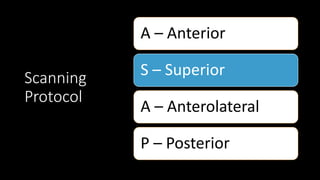
• To facilitate these objectives, the study used a standardized shoulder
US examination framework (ASAP [anterior, superior, anterolateral,
and posterior])
• Using a standardized approach to shoulder US will aid radiologists,
sonographers, and technologists in overcoming the barriers to
implementing shoulder US in clinical practice and help to promote
high-quality diagnostic imaging.](https://image.slidesharecdn.com/comprehensiveshoulderusexamination-240614004131-35bfbefd/85/Comprehensive-Shoulder-US-Examination-pptx-66-320.jpg)